Journal of Antivirals & Antiretrovirals
Open Access
ISSN: 1948-5964
ISSN: 1948-5964
Case Report - (2021)
Background: The coronavirus pandemic that started in December 2019 is mainly related to respiratory symptoms. Clinical presentations have been reported, but so far, no definitive therapy has been established. Intracranial haemorrhage has been observed in patients with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection, but the clinical, imaging, and pathophysiological features of intracranial bleeding during coronavirus disease 2019 (COVID-19) infection remain poorly characterized. The occurrence of spontaneous intracranial haemorrhage complicated with aseptic meningitis secondary to COVID-19 is extremely rare.
Case presentation: A 19-month-old with fever, and shortness of breath was admitted to our intensive care unit on an emergency basis. Two weeks later, the patient developed a generalized convulsion with deterioration of consciousness. A computed tomography scan of the brain revealed a bifrontal intracerebral haemorrhage compressing the anterior horns of both lateral ventricles of the brain with a massive intraventricular haemorrhage causing hydrocephalus. Emergency ventriculostomy was performed, and a nasal swab for SARSCoV-2 was positive. Cerebrospinal fluid analysis and culture were negative for microorganisms, and analysis revealed features of aseptic meningitis.
Conclusions: The possible occurrence of spontaneous intracranial haemorrhage and aseptic meningitis should be kept in mind by physicians, especially when treating critically ill young children with COVID-19. Early recognition of central nervous system involvement may be key to providing a better prognosis.
COVID-19; Aseptic meningitis; Intracerebral haemorrhage; SARS-CoV-2; Hydrocephalus
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is the virus responsible for corona virus disease 2019 (COVID-19), which was first discovered in late 2019 in Wuhan, China. Although the predominant clinical presentation is with respiratory disease, neurological manifestations are being recognized increasingly. SARS-CoV-2 infection results in distinct systemic and respiratory symptoms such as dry cough, fever, and breathing difficulty. In severe cases, patients may develop pneumonia, acute respiratory distress syndrome, cardiac injury, and multi-organ failure [1]. It was recently reported that, in addition to systemic and respiratory symptoms, some patients with COVID-19 develop neurological symptoms, including headache, dizziness, anosmia, encephalopathy, seizures, and stroke [2]. Both central and peripheral nervous system symptoms such as encephalopathy, Guillain-Barré syndrome-like manifestations and encephalitis have been reported in COVID-19 patients [3,4]. Herein, we report a case of a 19-month-old child with COVID-19 pneumonia, who presented with spontaneous intracranial haemorrhage (intracerebral and intraventricular) complicated by aseptic meningitis.
Clinical data
A 19-month-old female child presented to our hospital complaining of fever, cough, and tachypnoea. She had previously been diagnosed with collagen gene disease, congenital cytomegalovirus infection, and cerebral palsy and was vaccinated for up to one year. During examination, she was drowsy and had a temperature of 38.9°C, a Glasgow Coma Scale score of 13/15, both pupils dilated at 3 mm and reactive to light, pulse of 100 beat/min Blood pressure of 105/65 mmHg, respiratory rate of 35 breaths/ min, and generalized spasticity with hyperreflexia and hypertonia. Crepitation’s could be heard bilaterally on a chest examination. The patient was admitted to our intensive care unit in mid-July 2020. Chest radiography revealed lung infiltrations (a feature of severe acute respiratory distress). Septic screening was performed for both aerobic and anaerobic microorganisms, but the results were negative. Two weeks later, the patient developed breathing difficulty, transient generalized seizures that lasted about a minute, and hypotension. The patient was immediately intubated under sedation and connected to a mechanical ventilator with a high setting. The haemodynamic status was maintained by vasopressors. Brain computed tomography revealed a bifrontal intracerebral haematoma with a massive intraventricular haemorrhage and an External Ventricular Drain (EVD) was inserted surgically (Figures 1a and 1b). One week later, the patient developed fever; septic screening was again performed for both aerobic and anaerobic microorganisms, but the results were negative. Cerebrospinal fluid samples were collected from the EVD under aseptic conditions for analysis and a culture of bacteria and fungi; the results were negative. However, her nasal swabs were positive for COVID-19. The patient was started on a 10-day course of hydroxychloroquine, azithromycin, and methylprednisolone.
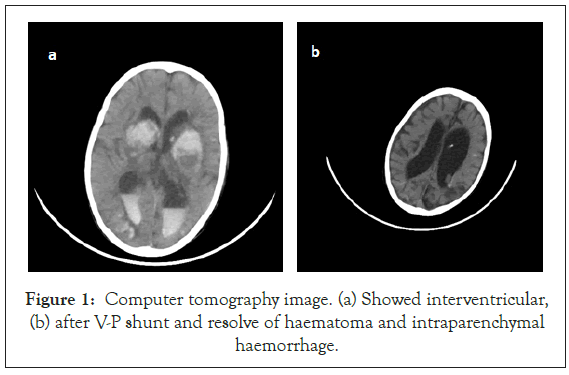
Figure 1: Computer tomography image. (a) Showed interventricular, (b) after V-P shunt and resolve of haematoma and intraparenchymal haemorrhage.
Laboratory data (including both blood tests and cerebrospinal analysis) during period of infection
Blood testing revealed, erythrocyte sedimentation rate of 135 mm/h (reference range, 0-20 mm/h), C-reactive protein level of 12 mg/L (reference range, <8.0 mg/L), haemoglobin level of 9.85 g/dL (reference range, 12-16 g/dL), D-dimer level of 0.897 mg/Dl (reference range, <0.5 mg/d/L), international normalize ratio of 0.9(reference range, 0.8-1.2), platelet account level of 72.34 × 103/L (reference range,15,000-450,000/uL), lymphocyte percentage of 11.1% (reference range, 20%-40%). Cerebrospinal fluid analysis revealed a viral pattern, clear and colorless, glucose level of 110 mg/dL (reference range, 45-80 mg/dL), elevated level of protein 63 mg/dL (reference range <45 mg/dL), White cell count of 100 cells/cubic milliliter (reference range, 0-5 cell/cubic milliliter), with more than 70% activated lymphocytes, (reference range is less than 70%) (Table 1). Cultures for both bacterial and fungal samples were negative, gram staining using Giemsa stain was negative, latex test for bacterial antigen was negative, and polymerase chain reaction for mycobacterium tuberculosis is negative. Another nasal swab for COVID-19 was taken, which was also positive. The third nasal swab at the beginning of September 2020 was negative for COVID-19. Viral screening for hepatitis A, B, and C was negative, TORCH screening (Toxoplasmosis, Rubella, Cytomegalovirus, and Herpes Simplex) was negative, and haemophilus influenza type A screening was negative. The EVD was replaced by a ventriculoperitoneal shunt. The patient was discharged home without neurological complications.
| Sample | Test | Result | Reference values |
|---|---|---|---|
| CSF from EVD | Colour | Colorless | |
| Glucose | 110 mg/dL | 45-80 mg/dL | |
| Protein | 63 mg/dL | 15-45 mg/dl | |
| WBC | 100 | 0-5 cells/mm3 | |
| Lymphocyte percent | More than 70% | 60%-70% | |
| Monocyte percent | 10% | 30%-40% | |
| AFB PCR | Negative | ||
| Latex test | No reaction | ||
| Culture for both bacterial and fungal | No growth after 48 hr incubation | ||
| Gram stain | No micro- organism seen |
Abbreviations: WBC: White Blood Cells; AFB: Acid Fast Bacilli; PCR: Polymerase Chain Reaction
Table 1: Cerebrospinal fluid result during COVID-19 infection.
Our report described a case of spontaneous intracranial haemorrhage complicated with aseptic meningitis in a young child with COVID-19. Aseptic meningitis describes a clinical syndrome characterized by meningeal inflammation not caused by an identifiable bacterial pathogen in the cerebrospinal fluid [5]. Unexpectedly, acute cerebrovascular disease is also emerging as an important complication that happen during period of illness. Patients with COVID-19 infection develop stroke during period of illness have been described. Cerebrovascular manifestations were reported for 13(6%) of 221 COVID-19 patients in an early retrospective case series from Wuhan [6]. 11(5%) patients developed ischaemic stroke, one (<1%) had intracerebral haemorrhage, and one (<1%) had cerebral venous sinus thrombosis Most patients were older than 60 years, and many had known risk factors for cerebrovascular disease, especially hypertension, diabetes, hyperlipidemia, and vascular disease, in contradistinction to our case report, doesn’t have any risk factor for intracranial haemorrhagic event, this is raise possibility of the occurrence of intracranial haemorrhage during COVID-19 infection without previously known risk factors. It had been noted that COVID-19 may increase risk for acute cerebrovascular events through many postulated hypotheses regarding possible mechanisms for virus to gain access in to the nervous system [7]. These include direct invasion of SARS-CoV-2 into the nervous system, as evidenced by the discovery of the viral protein in cerebrospinal fluid of a patient with COVID-19, who was suspect of developing encephalitis. The route of viral entry to the brain through cribriform plate of ethmoid bone and travel through the olfactory bulb is one feasible route for SARS-CoV-2 as evidence by symptom of hyposmia, Alternative possible entry routes include carriage across the blood-brain barrier through infected leukocytes [8]. The angiotensin converting enzyme 2 receptor, to which SARS-CoV-2 bind for entry in to cells is found in brain vascular endothelium and smooth muscle may facilitate the movement of the virus through the blood brain barrier [9-11]. Brain express ACE2 receptors which may increase their susceptibility as potential target of SARS-CoV-2. Moreover, the adhesion of SARS-CoV2 to ACE2 receptors gains significant importance in the cases of intracerebral haemorrhage, due to the inactivation of the receptor and later autoregulatory dysfunction, which may be the pathophysiological mechanism behind the intracranial bleeding, observed in SARS-CoV-2 infection [12]. However, the exact mechanisms not fully understood. Contamination of the CSF by the patient’s blood or other biological secretions that contained the genetic material of SARS-CoV-2, cannot be entirely excluded as a leading mechanism to develop aseptic meningitis in context of intraventricular haemorrhage. The cerebrospinal fluid picture described in our patient laboratory result, highlight the importance in considering aseptic meningitis as an extrapulmonary complication of SARS-CoV-2 infection in pediatric patients, especially during the COVID-19 pandemic [13].
It is imperative to be aware of the nervous system related extrapulmonary manifestations of COVID-19 in critically ill patients to avoid delayed diagnosis. In sedated and mechanically ventilated patients, newly developing seizures or changes in pupil size and reaction to light should raise red flags, prompting investigations that might detect the occurrence of brain damage. Temporary ventriculostomy is a safe neurosurgical intervention in COVID-19 patients with acute hydrocephalus caused by intraventricular haemorrhage.
Ethics approval and consent to participate
Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying image and laboratory results.
Consent for publication
The patient parents have consented for online submission and publication, written informed consent for publication was obtained from all participants.
Availability of data and materials
All data generated or analyzed during this case study are included in this article and its supplementary information files.
Competing interests
No potential competing interest was reported by the author.
Funding details
No financial support
Author Contributions
The author contributed to the study conception and design. Patient management, data collection, and analysis, surgical management, all co-authors read and approved for final manuscript.
Acknowledgment
I would like to thank my colleague, Dr. Abdulaziz Abulla Hamad(Emergency physician), for his valuable support in the completion of this article.
Citation: Mohamed MA, Alawaad AO, Almesedin G, Assaggaf SA, Alshammary ZA, Ahmed MAM. (2021) Impact of COVID-19 on the Central Nervous System: Are Spontaneous Intracranial Hemorrhage and Aseptic Meningitis Extra-pulmonary Manifestations of COVID-19? A Rare Case Report and Literature Review. J Antivir Antiretrovir. S17:003. DOI: 10.35248/1948-5964.21.S17.003
Received: 02-Feb-2021 Accepted: 16-Feb-2021 Published: 23-Feb-2021 , DOI: 10.35248/1948-5964.21.s17.003
Copyright: © 2021 Mohamed MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.