Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Case Report - (2022)Volume 13, Issue 1
Cardiac tamponade is a cardiac emergency requiring prompt diagnosis using adequate clinical history and bedside echocardiography. Immediate relief of theintrapericardial tension by pericardiocentesisis life saving and reduces mortality. This case demonstrates the echocardiographic findings of cardiac tamponade pre (large pericardial effusion, swinging heart, collapse of right atrium and ventricle) and immediate post pericardiostomy in a 44-year old Nigerian man who presented with sudden onset breathlessness, easy fatiguability, abdominal swelling and beck’s triad (jugular venous distention, hypotension, and muffled heart sounds). About 2000 mls of haemorrhagic fluid was drained following which there was spontaneous resolution of his vital signs and normalization of the echocardiographic findings. Further evaluation of the patient could not demonstrate the aetiology of the haemopericardium and patient has remained symptom free 3 months post discharge.
Congenital foregut cyst; Mediastinal-intrapulmonary bronchogenic cyst; Lung abscess
Cardiac tamponade is a life-threatening, slow or rapid compression of the heart due to fluid, pus, blood, clots or gas accumulation within the pericardium as a result of inflammation, trauma, and rupture of the heart or aortic dissection [1]. Cardiac tamponade may present as acute heart failure and requires a high index of clinical suspicion with prompt echocardiography, as early diagnosis impact treatment positively and reduce mortality. The incidence of cardiac tamponade based on a large sample size of about 216 million emergency admissions was about 115,638(0.05%) [2]. There is paucity of data regarding the incidence and prevalence in sub-Saharan Africa. The leading cause of tamponade in developed countries is cancer while it is tuberculosis in developing countries [3]. Cardiac tamponade mortality rate is significantly different due to its underlying cause, but overall, hospitalized mortality rate is around 14.3% [4].
We present a case of idiopathic cardiac tamponade presenting as acute heart failure in a 44-year old Nigerian man with estimated haemopericardium of 2000 mls and a triage cardiac tamponade score >6. Immediate bedside echocardiography showed a swinging heart in a severe circumferential echo free space with obvious diastolic collapse of both the right atrium and ventricle. Immediate pericardial tap showed a non-clotting haemorrhagic fluid, but was offered an urgent surgical tube pericardiostomy.
Mr B.C.O is a 44-year old Nigerian man who presented with sudden onset breathlessness, cough and easy fatiguability. He had orthopnea, abdominal swelling and pain but no leg/facial swelling. Patient has significant history of alcohol abuse, and smokes cigarette and smoked Indian hemp heavily. Patient had no history of recent surgery, long distance travel, fever, weight loss and haemoptysis. He is not a known hypertensive and diabetic. He was acutely ill looking, not febrile, not cyanosed, not jaundiced, nil lymphadenopathy, nil leg oedema. He was tachypneic, tachycardic, hypotensive (80 mmHg/50 mmHg), neck veins were distended and heart sounds were muffled. There was a bi-basal coarse crackle and oxygen saturation (SPO2) was 92%. His abdomen was distended with visible veins, moves with respiration and tender hepatomegaly was present. A tentative diagnosis of acute heart failure in cardiogenic shock from pericardial effusion to rule out pulmonary embolism was made. Blood samples were collected for kidney and liver function test, full blood count, erythrocyte sedimentation rate and human immunodeficiency virus 1 and 2 screening. Sputum was collected for GeneXpert MTB/RIF. Immediate bedside echocardiography Video 1 showed a swinging heart surrounded by a massive echo free space and a diastolic collapse of right atrium and ventricle. Figure 1 shows the picture of the patient about one post pericardiostomy. A confirmed diagnosis of cardiac tamponade was made in correlation with the clinical presentation. Immediate blind pericardial tap was done and about 60 mls of haemorrhagic fluid was removed. A decision was made for tube pericardiostomy and pericardial biopsy; hence cardiothoracic consult. A total of about 2000 mls of haemopericardial fluid was removed. Pericardial tissue was sent for histology, while the fluid was sent for acid fast bacilli staining, GeneXpert MTB/RIF, culture and cytology but results were not suggestive of any pathology (Figures 2-5). Immediate post tube pericardiostomy echocardiography showed disappearance of echo free space, normal contracting heart and no diastolic collapse of the right atrium and ventricle (Figure 6). Patients clinical features improved remarkably but steadily following the procedure. He had chest radiography post pericardiocentesis which showed right pleural effusion +/- consolidation and cardiomegaly in Figure 4. He was however continued on tabs azithromycin, IV ceftriaxone (1 g daily), metronidazole (500 mg 8 hourly) and frusemide (40 mg daily) for five days and discharged. He has visited the clinic thrice and has remained symptomless.
Video 1: Video of the patient’s echocardiogram showing swinging heart in a large echo free space.
Figure 1: Showing the patient 1 hour post-pericardiostomy.
Figure 2:Showing the result of the acid fast bacilli using the pericardial fluid.
Figure 3: Showing report of the chest radiograph post pericardiostomy.
Figure 4: Showing result of the histology of the pericardial tissue biopsy.
Figure 5: Showing the result of the pericardial effusion fluid.
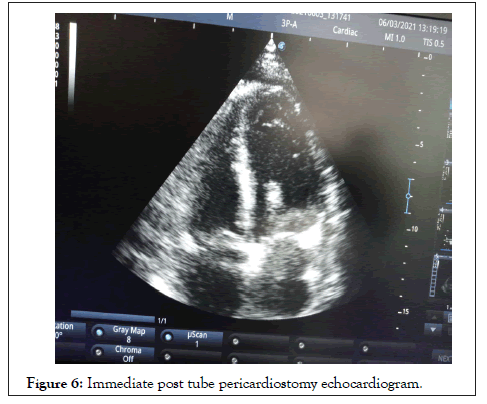
Figure 6: Immediate post tube pericardiostomy echocardiogram.
Cardiac tamponade is a clinical diagnosis defined as a lifethreatening, slow or rapid compression of the heart due to fluid, pus, blood, clots or gas accumulation within the intrapericadial space, often due to inflammation, trauma, and rupture of the heart or aortic dissection [1]. The clinical presentation could be acute or chronic, but this depends on several factors including the rate of fluid accumulation, mechanism of accumulation and compliance of the pericardium [5]. Clinical features may include history of weight loss, fatigue or anorexia (malignancy), chest pain (pericarditis or myocardial infarction), musculoskeletal pain or fever (connective tissue disease), history of renal failure (uremia), medications (drug-related lupus), recent cardiovascular surgery/ intervention or surgery, shortness of breath, easy fatiguability, cough/haemoptysis, orthopnea, excessive sweatiness and fever. On examination, patient may have tachypnea, tachycardia,pulsusparadoxus, muffled heart sound, raised jugular venous pressure, hypotension etc [5,6,7]. Our patient presented acutely with cough, shortness of breath, easy fatiguability, orthopnea, and hypotension, muffled heart sound, abdominal distention, raised jugular venous distension and dysphoria (restlessness with a sense of an impending doom). Common causes of cardiac tamponade include pericarditis, tuberculosis, iatrogenic (invasive procedurerelated, post-cardiac surgery), trauma and neoplasm/malignancy while the uncommon causes are collagen vascular diseases (systemic lupus erythematosus, rheumatoid arthritis, and scleroderma), radiation induced, postmyocardial infarction, uremia, aortic dissection, bacterial infection and pneumopericardium [8]. In sub Saharan Africa, cardiac tamponade are largely from tuberculosis [9], but the cause in our patient is unknown.
In tamponade, there are several hemodynamic changes including impaired diastolic filling, altered systemic venous return, right arterial collapse, right ventricular collapse and reduction in cardiac output [10]. These changes occur because the excessive accumulation of fluid in the intra-pericardial space makes the transmural distending pressures insufficient to overcome it, thereby leading to impaired diastolic filling. The fluid also causes compression of the heart throughout the cardiac cycle, leading to impairment of systemic venous return and collapse of both right atrium and ventricle. Blood accumulates in the pulmonary bed at the expense of the left ventricle, leading to reduced cardiac output [10]. In cardiac tamponade, echocardiography, electrocardiography (ECG), chest radiography, cardiac catheterization, cardiac computed tomography (cardiac CT), cardiac magnetic resonance imaging (cardiac MRI), cause-specific testing including GeneXpert MTB/RIF, Antinuclear Antibody (ANA), Rheumatoid Factor (RF) serum electrolyte, urea/ creatinine (s/e/u/cr), full blood count, culture and sensitivit etc, are some of the investigations that may be required but our patient did few of them. The ECG findings may include low amplitude voltages, electrical alternans, sinus tachycardia, changes in ST-T wave patterns and PR segment depression, but unfortunately we lost the ECG tracing of our patient [11]. Echocardiography will show an echo free space, a swinging heart, early diastolic right ventricular collapse (high specificity), systolic (late diastolic) right artrial collapse (earliest sign), a plethoric inferior vena cava with minimal respiratory variation (high sensitivity), and exaggerated respiratory cycle changes in mitral and tricuspid valve in-flow velocities as a surrogate for pulsusparadoxus [12]. Our patient had swinging heart, large circumferential echo free space, diastolic collapse of both right atrium and ventricular and a plethoric inferior vena cava. Interestingly an immediate post-operative echocardiography was performed and all these signs had disappeared. Although chest radiography has been shown to be poorly diagnostic of large pericardial effusion; however,water bottle sign, a predominant leftsided pleural effusion and a pericardial fat stripe are suggestive, but not diagnostic [13]. Because of the emergent nature of our patient, chest radiography was done post pericardiocentesis in search of aetiology. His pericardial tissue biopsy result was also not contributory. Other investigations including culture and GeneXpert MTB/RIF of the haemorrhagic fluid, thyroid function test, s/e/u/cr and full blood count were not contributory. It is known that in developing countries, the complete armamentarium in investigating the aetiology of massive pericardial effusion is lacking, however, idiopathic causes have been put at 15.8% [9].
The life-threatening nature of cardiac tamponade warrants an emergent treatment to reduce mortality. In this regard, immediate relief of the compression is the hallmark of treatment. This approach may entail ultrasound guided needle pericardiocentesis or subxiphoidpericardiostomy which our patient had [14]. This also supports the view of surgical management of acute heart failure where cure may be established [15].
The aetiology of the large effusion may be treated after the compression is relieved if known to prevent fluid re-accumulation. Cardiac tamponade is associated with high mortality if not diagnosed early and promptly treated. Therefore, high index of clinical suspicion and immediate bedside echocardiography is important for early diagnosis. Subxiphoidpericardiostomy is life saving and afford the opportunity for further investigation using the pericardial tissue biopsy.
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar] [Pubmed].
[Crossref] [Google Scholar].
[Crossref] [Google Scholar].
Citation: Nwako OF, Okonta KE; Nwako AB; Nwako CA (2022) Haemopericardium with Cardiac Tamponade in a Nigerian Man Residing in Owerri: A Case Report. J Clin Exp Cardiolog. 13:711.
Received: 14-Mar-2022, Manuscript No. JCEC-22-15357; Editor assigned: 17-Mar-2022, Pre QC No. JCEC-22-15357(PQ); Reviewed: 31-Mar-2022, QC No. JCEC-22-15357; Revised: 05-Apr-2022, Manuscript No. JCEC-22-15357(R); Published: 12-Apr-2022 , DOI: 10.35248/2155-9880.22.13.710
Copyright: © 2022 Nwako OF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.