Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research - (2023)Volume 14, Issue 5
Rosacea is a common inflammatory disease affecting the face with flushing, papules, pustules and telangiectasias. Granulomatous Rosacea (GR) is infrequent recognized variant of rosacea. Clinically it is a chronic disorder that primarily affects periorificial regions of the face and forehead. The purpose of our work was to systematically review available data about clinical presentation and treatments on granulomatous rosacea. Hence, a systematic review of studies evaluating GR was performed. The search yielded 1363 publications, with 18 eligible for review. Together with our case report, 19 studies were included overall. GR affected 39 males (41%) and 55 females (58%) women, mean age was 47 for males and 48 years for females. Youngest patient of GR was 9 years of age with upper range of 80 years. Cheeks were most common involved (64%), afterwards nose (34%), chin (18%), forehead (9%) and eyelid’s (5%). There is no well-defined treatment protocol when it comes to management of GR. For oral treatments first line of treatment were oral antibiotics such as tetracycline or doxycycline (13 out of 18 studies;72%), second and third lines were isotretinoin (3 out of 18 studies;16%), systemic corticosteroids (3 out of 18 studies; 16%), dapsone (3 out of 18 studies;16%), metronidazole (2 out of 18 studies, 10%), PDT, IPL and Chromophore Gel-Assisted Phototherapy (CGAP) each mentioned once (1 out of 18 studies;5%).
As for topical treatments metronidazole cream (7 out of 18 studies; 39%) was the most prevalent, afterwards tretinoin 0.025% cream, combination of 20% Jessner (Rejuvenize®) and 0.3%, pimecrolimus, topical azelaic acid, benzoyl peroxide, brimonidine and ivermectin were used. The treatment of GR largely depended on the phenotypic presentation that varied in each patient.
Rosacea; Granulomatous rosacea; Demodex
Rosacea, a commonly encountered skin disease, predominantly affects the central part of the face in a symmetric manner. The clinical presentation involves episodes of transient and persistent erythema, edema, papules, telangiectasias and pustules [1]. Different subtypes of rosacea have been established according to the grading system of the National Society in 2002 including:
Papulopustular, erythematotelangiectatic, phymatous, ocular and the granulomatous variant [2]. Among these categories, Granulomatous Rosacea (GR) has been categorized as a separate disease variant mainly because of its specific histopathologic characteristics. GR is different from other forms of rosacea owing to its distinct clinical presentations such as it does not necessarily presents with facial erythema, or facial convexities, shows an asymmetrical distribution, and in most of the cases consist of periocular lesions [1].
GR consist of lesions localized around different areas of face such as nose, eyes and mouth on normal appearing skin, which are in the form of firm, papules or nodules that may be brown, yellow, red or flesh-colored [2]. Interestingly, these papules are located on the lateral side of the face and below the mandibular region, on the neck [3]. It may present with other signs of rosacea such as flushing, telangiectasia, or erythema, however they do not help in its diagnosis [2]. Furthermore, there may be overlap of GR and rosacea in some patients, where the common symptoms include facial swelling, burning or stinging, pruritus or irritation [4]. Evidence suggests that GR can also present with extrafacial lesions on the axilla, shoulder, ears, neck groin, thigh, and knees [3]. GR due to its chronic and unpredictable nature is difficult to treat and standard rosacea treatments do not result in desirable outcomes. According to clinical studies findings, the clinical course can range from 6 months to 4 years [4].
Systemic involvement and engagement of other organ systems is not typically present in GR, however the extent may vary depending on the spectrum of rosacea. For example, it is observed that 50% of patients with cutaneous rosacea also consist of ocular rosacea [5,6]. A case report mentioned that after undergoing treatment with systemic steroids, a patient developed parotid, lacrimal, and submandibular gland swelling, which was resolved after being treated with minocycline [7]. Therefore, it is important to remember that patients who have other systemic complaints should be examined thoroughly to rule out other possible diagnosis in the differentials such as sarcoidosis.
The etiology of GR (as that of rosacea) is still unclear. Researchers and clinicians have hypothesized role of several key factors involved in the pathogenesis of this variant. Demodex folliculorum is considered as one of the important etiologic factors for rosacea [8], as surrounding hair follicles gets infiltrated with noncaseating granulomatous consisting of Demodex folliculorum [9]. Several authors have suggested that other factors also affect pathogenesis of GR and disease progression, such as the quantity and location of the mite, immune response, genetic susceptibility, and host’s defense mechanism against the mite [10].
As to treatment, currently, there is no standardized treatment of GR, with only few case reports highlighting therapeutic effectiveness in individual patients. GR shares disease similarity with two diseases namely, sarcoidosis and papulopustular rosacea, hence the therapeutic efforts for GR are largely based on the use of medications commonly used for these two. The most accepted treatment modality involves tetracycline family of medications (for example, 250-500 mg of tetracycline thrice a day, 50-100 mg doxycycline or minocycline twice a day). The underlying mechanism of this group of medication prevents granuloma formation by inhibiting protein kinase C, a signaling enzyme in the inflammatory pathway [11]. Several other therapeutic agents that have shown beneficial outcomes in GR include topical corticosteroids, systemic corticosteroids, azelaic acid, topical metronidazole, benzoyl peroxide, and oral erythromycin.
Although GR is considered a distinct clinical entity with varied findings among the patients, but still there is not sufficient clinical evidence to support this hypothesis. Research has demonstrated wide spectrum of clinical presentations and overlapping facial characteristics including different subtypes of rosacea [3]. It is still a challenging situation for dermatologist to specify the clinical picture that could confirm the diagnosis of GR [12-17].
Due to scarce evidence available in the literature, the present systematic literature review aims to elaborate the current clinical findings associated with GR and discuss the latest treatment modalities, including topical agents, oral antibiotics, oral retinoids, laser etc.
The present review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA Checklist 2009). PROSPERO number 252030.
Research objectives
• Elaborate the current clinical findings associated with GR
• Evaluate different therapeutic agents that have shown beneficial results in GR, highlighting the latest evidence in association with their effectiveness.
Search strategy
A computerized literature search was performed in MEDLINE (PubMed), the Cochrane Library, EBSCOhost (Dentistry and Oral Sciences Source) and Embase databases from 1st January 2000 until 31st, March 2022. The Cochrane Handbook for Systematic Reviews of Interventions was used to include relevant controlled trials. References of textbooks and selected articles were screened to identify any relevant studies. The literature search was performed by including following terms related to Granulomatous rosacea: Granulomatous skin diseases, clinical, treatment, granulomatous rosacea, skin diseases, granulomatous dermatitis [18-20].
Eligibility criteria
Inclusion criteria: The full text articles of the relevant studies were then obtained and reviewed by two reviewers (AA and YT) independently to ensure that the studies met the inclusion criteria. The inclusion criteria were as follows:
• Studies published in English language only
• Studies that adequately mentioned clinical features of GR
• Studies examining all types of interventions in people with GR, and their significance.
Exclusion criteria: Studies that have been published in foreign languages.
• Editorials, letters, abstracts, comments and book chapters
• Studies where the in vitro analysis was performed in animal models
• Studies where the clinical features of GR were not clearly demarcated and did not mention relevant findings
Study selection
The relevant studies were selected by initiating search strategy in two stages. Firstly, two authors (AA and YT) were independently involved with the process of this study and extracted the necessary information. All available titles and abstracts were identified and scanned by them such that the included studies met the inclusion criteria. In the second stage, full text articles were thoroughly investigated by both the reviewers independently. Papers that had cited these articles were also identified through Science Citation Index (http:// www.isinet.com) to identify potentially relevant articles subsequent primary research. After study selection, if there were any disagreements then it was mutually discussed, and a consensus was made before inclusion of the study in this review [21-25].
Data extraction and quality assessment
Studies that fulfilled the inclusion criteria were processed for study details and outcome data. The primary focus of the review was the assessment of clinical features, and therapeutic approaches that have been mentioned in the literature. Two reviewers independently extracted the data. The following details were extracted: Study design, year of publication, country of origin, sample size, sex and age of participants, dropouts and losses to follow-up, clinical features, baseline data , any other systemic involvement, intervention, treatment time period, clinical outcomes, and adverse events. Two authors (AA and YT) independently assessed risk of bias using the Cochrane Collaboration’s domain-based assessment tool (Figure 1).
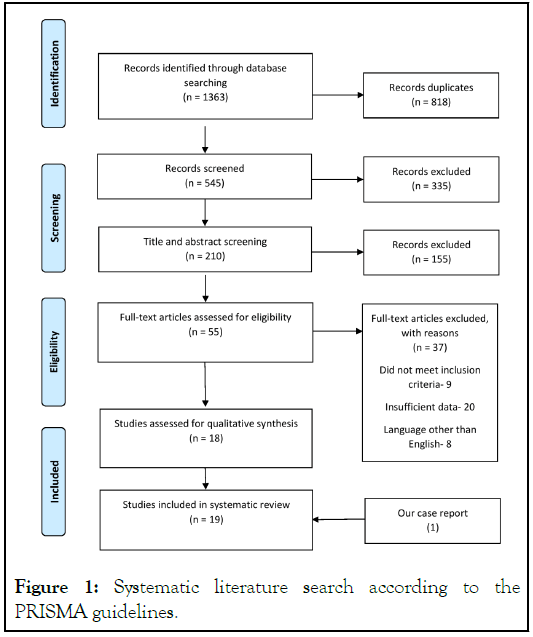
Figure 1: Systematic literature search according to the PRISMA guidelines.
Index case
A 24 -year-old male patient, present to our dermatology clinic in the June 2020. Previously, a year ago, single asymptomatic erythematous papule had appeared on his forehead and was biopsied to rull out proliferative condition. In pathology, lymphohistiocytic infiltrate with granulomatous pattern [26]. No leishmania particles were detected. After several months similar papular erythematous eruptions emerged on his forehead. Physical examination revealed normal skin face, with red discrete papules and nodules on his forehead (Figure 2A).
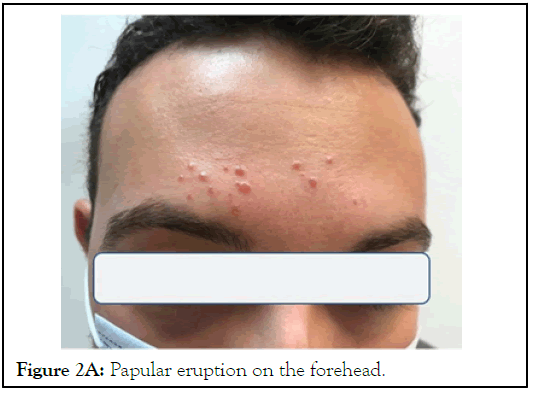
Figure 2A: Papular eruption on the forehead.
No ocular involvement or telangiectasia was noted. Under dermoscopy, gelatinous filaments protruding out of the follicular openings known as “Demodex tails” were observed. He was initially treated with oral metronidazole 250 mg three times a day for 2 weeks and topical polycutan (clotrimazole/ neomycin/dexamethasone) for a week followed by benzoic acid for two months, but there was no improvement. A skin biopsy was performed and the histology report revealed atrophic epidermis. Within the dermis, non-caseating granulomatous inflammation, composed of lymphocytes, epithelioid histiocytes and some foreign body type multinucleated giant cells, was seen. The Gram, Ziehl-Neelsen and PAS stains on histology were negative [27-29]. Further evaluation included ACE levels and chest Xray ruled out sarcoidosis. A diagnosis of Granulomatous Rosacea (GR) was made. The oral isotretinoin 40 mg/day together with topical ivermectin 1% cream was started. Marked improvement was showed significant clinical improvement was noted after two months. Isotretinoin was gradually tapered over 16 weeks and complete remission was achieved (Figure 2B).
Figure 2B: Resolution of lesions. No recurrence was seen 3 months after the cessation of therapy. Note: Informed consent for photo has been obtained from the patient.
Systematic review
The process of retrieving and screening the studies which were included for in this systematic review is shown in Figure 3. After an initial search a total of 1363 articles were identified. After screening the titles and abstracts, only 210 were found to be relevant. The remaining studies were excluded as some of them were duplicated, irrelevant and others did not justify the inclusion criteria. Then, 55 studies which were full-text articles were critically reviewed by two reviewers (AA and YT) independently for eligibility. Finally, 18 studies which met all the inclusion criteria were included in the review.
Figure 3: Shown flow chart summarizing approach to granulomatous rosacea workout.
Characteristics of studies included in the systematic review
The included studies were assessed on several factors around clinical presentation and treatment approaches as mentioned in Table 1. The following parameters were included: The author and year, gender, number of study participants, study design, clinical characteristics including demodex detection, ladder of treatments and comments.
| Ref. and study design | Gender/Age (years) | Clinical signs and (demodex presence) | Treatment | Notes |
|---|---|---|---|---|
| Helm, et al. [3] Retrospective study |
53 patients (36 female/17 male) mean of 50 years (range 26 to 80 years) |
Cheeks were most common involved (77%), afterwards chin (22%), nose (36%). Demodex presence-demodex folliculorum was identified in 9 of the 53 biopsy specimens (17%). | First line: Tetracycline, erythromycin, and minocycline. Topical steroids Second line: Ayres' ointment, Nomland's solution, tretinoin (Retin-A), benzoyl peroxide, sulfa preparations. |
|
| Ohata , et al. [6] Case report |
Male 59 years old |
Erythematous papules on the cheeks chin and nose. Swelling of the lacrimal, parotid, and submandibular glands. Demodex presence-not mentioned |
First line: Prednisolone 20 mg/day PO deteriorated the lesions Second line: Minocycline 200 mg/day PO improvement after 1 month |
This study is believed to be the first case report where GR was shown to affect lacrimal and salivary glands |
| Trindade Neto, et al. [17] Case report |
Male 39 years old |
Right temporal region a reddish plaque, demodex presence-not mentioned | First line: Topical steroids Second line: Limecycline (300 mg/day) PO for 30 days. Metronidazole gel (0.5%) administered for 2 months |
Lymecycline, effective tetracycline derivate, which has minimal side-effects |
| Sanchez, et al. [22] Retrospective histological study |
24 patients (Male:Female ratio 1:1) mean of 46 years range 9 to 75 years |
Papules, pustules, erythema, and telangiectasias common locations cheeks (46%) and nose (21%) demodex Presence-demodex folliculorum was identified in 7 of the 24 biopsy specimens (29%) | Not mentioned | |
| Winter, et al. [20] Case report |
Female 73 years old |
History of psoriasis treated with etanercept for 4 weeks. Erythematous, reddish-brown papules and nodules on the face. Demodex presence-not mentioned | First line: Metronidazole topically Second line: Etanercept was discontinued and changed to Humira with complete remission |
This is one of the first reported study where etanercept therapy led to granuloma formation, and eventually diagnosed as GR |
| Gul, et al. [19] Case report |
Male 43 years old |
Papules and pustules on the nose, forehead, cheeks, and lower eyelids. Demodex presence-not mentioned | First line: Clindamycin and doxycycline PO (dosages unmentioned) Second line: Pimecrolimus cream (1%) after 4 months |
|
| Mahony, et al. [24] Case report |
Female 49 years old |
Dark grey papules on face' some of the coalescing into plaques, demodex presence-not mentioned | Doxycycline (100 mg twice daily) for 2-4 months. Metronidazole topically | |
| Lane, et al. [27] case report |
Female 55 years old |
Erythematous symmetrical plaques involving the cheeks, with scattered, erythematous papules. Demodex presence-not mentioned | First line: Doxycycline (100 mg twice day for 4 months). Clindamycin topical Second line: Dapsone 150mg Topical tacrolimus, corticosteroids, metronidazole and azelaic acid Third line: Six Pulsed light (IPL) treatments, at 4-week intervals |
|
| Baglieri, et al. [28] Case report |
Male 50 years old |
Facial erythema with multiple brownish-red papules involving the chin, cheeks, neck below the mandibular demodex presence-not mentioned | First line: Tetracycline Second line: 6 sessions of PDT with δ-aminolaevulinic acid 20% (ALA). At 2 weeks intervals |
PDT resulted in demonstrating significant improvement in erythema and lesions. |
| Fernandez, et al. [18] Case report |
Male 54 years old |
Erythematous papules forehead, eyelids and cheek involving plaques with scales; demodex presence-not mentioned |
First line: Isotretinoin 20 mg | |
| Rallis, et al. [26] Case report |
Female 28 years old |
Erythematous papules involving medial and lateral regions of the face. Diascopy, yellowish-brown color was observed in the papules, demodex presence-not mentioned | First line: Tetracyclines and macrolides PO. Metronidazole, clindamycin and pimecrolimus topical Second line: Isotretinoin 0.7 mg/kg/d, satisfactory results after 12 weeks. |
isotretinoin at a dose of 0.3 mg/kg proved to be effective in patients resistant to standard therapies. |
| Ehmann, et al. [14] case report |
Male 62 years old |
Scattered red-brown papules and nodules around ocular and centro facial regions, demodex presence-not mentioned | First line: Doxyline 40 mg (Oraycea) PO Second line: Isotretinoin 30 mg PO Corticosteroids 60 mg PO Third line: Complete resolution with dapsone 100 mg PO. Tacrolimus topical |
Patient who are resistant to normal therapeutic approaches can be managed by dapsone. |
| Hu, et al. [15] Case report |
Female 21 years old |
History of atopic dermatitis treated with tacrolimus 0.1%. Erythema, papules, and nodules around the ocular and central region of face demodex presence- not mentioned | First line: Tacrolimus discontinued Second line: Doxycycline 200 mg/day PO Topical including: Metronidazole cream, tretinoin 0.025% cream, combination of 20% Jessner (Rejuvenize®) and 0.3% retinoic acid peels |
severe granulomatous rosacea because of increased use of tacrolimus. |
| Mitoma, et al. [13] Case report |
Male 15 years old |
Erythema of forehead, cheeks, lower eyelids, and perioral region, demodex presence- not mentioned | First line: Prednislone 5 mg/day PO; Doxycycline 200 mg/day PO for 2 weeks Second line: Roxithromycin 300 mg PO; Azaleic acid 20% topical |
|
| Kelati, et al. [21] Case report |
Male 54 years old |
Erythematous, talengiectatic, confluent papules on lateral side of the eyes without any scales or pustules, demodex presence-presence of Demodex folliculorum on the biopsied tissue | First line: Metronidazole topically | |
| Kok, et al. [16] Case report |
Female 61 years old |
Erythematous papules coalesced to plaques on the cheeks, nose, glabella and chin, demodex presence-not mentioned | First line: Tetracycline 250 mg twice daily PO. Metronidazole topical for two months Second line: Doxycycline 100 mg twice daily PO Prednisolone 0.5 mg/kg/day gradually tapered (8 weeks) brimonidine gel resulted in reducing erythema. |
topical brimonidine gel, is an alpha-adrenergic vasoconstrictor it greatly helped in reducing erythema |
| Liu, et al. [25] Case report |
Female 50 years old |
Tumid papules and pustules in the glabella. Malar erythema, and fine telangiectasia, demodex presence-not mentioned | First line: Minocycline 50 mg PO was stopped due to headache. Modest improvement on topical metronidazole, ivermectin and brimonidine. Second line: Chromophore Gel-Assisted Phototherapy (CGAP) 12 treatments during 6 months |
Chromophore gel-assisted phototherapy showed effective results in treatment of GR that are resistant to traditional therapies. |
| Merlo, et al. [29] Case report |
Male 42 years old |
Multiple papulopustular lesions on the cheeks, nose, zygomatic and mandibular areas demodex presence-not mentioned |
First line: Doxycycline 100 mg/day PO topical metronidazole Second line: Dapsone 100 mg/day |
|
| Our case report | Male 24 years old |
Multiple papules on his forehead demodex presence-mentioned | Topical clotrimazole/neomycin/dexamethasone and benzoic acid Second line: Isotretinoin 40 mg/day PO topical ivermectin1% cream |
Table 1: Patients’ main characteristics; including: Reference and study design, gender, clinical signs, treatments and notes; and demodex presence if mentioned in clinical presentation.
Out of 19 studies, 17 were case reports and 2 retrospective studies. All together studies included 39 males (41%) and 55 females (58%), mean age was 47 for males and 48 for females, with the youngest male and female participant diagnosed with GR of age 15 years and 21 years respectively. In the 19 studies, different clinical characteristics were observed including presence of erythema on the forehead, cheeks, lower eyelids, and perioral region [15,16], scattered papules and nodules located around the ocular region [16], telangiectasia, facial eruption in response to overuse of tacrolimus ointment [17], and areas of desquamation [19]. In one of the studies along with presence of erythematous papules on the cheeks, nose and chin, swelling of the lacrimal, parotid, and submandibular glands was also present [20-22]. In another study, in respon
e to etanercept therapy administration in a psoriasis patient resulted in granuloma formation, and eventually diagnosed as GR [23]. As to follicular openings and demodex tails, demodex was mentioned twice in case reports and in 16 of 77 in retrospective studies, therefore in demodex was mentioned in 19% of all cases.
There is no well-defined treatment protocol when it comes to management of GR.
In the present systematic review several steps of interventions were administered; for oral treatments first line of treatment were oral antibiotics such as tetracycline or doxycycline (13 out of 18 studies; 72%), second and third lines were isotretinoin (3 out of 18 studies; 16%), systemic corticosteroids (3 out of 18 studies; 16%), dapsone (3 out of 18 studies; 16%), metronidazole, PDT, IPL and Chromophore Gel-Assisted Phototherapy (CGAP) each mentioned once (1 out of 18 studies; 5%).
As for topical treatments metronidazole cream (7 out of 18 studies; 39%) was the most prevalent, afterwards tretinoin 0.025% cream, combination of 20% Jessner (Rejuvenize®) and 0.3%, pimecrolimus, topical azelaic acid, benzoyl peroxide, brimonidine and ivermectin were used. The treatment of GR largely depended on the phenotypic presentation that varied in each patient.
GR, a variant of rosacea which particularly involves central part of face, is usually characterized by discrete papules and nodules, while sometimes erythema and telangiectasia. Studies report that it is primarily observed among women in their 30’s and 40’s [24]. Our study is in line with previous observations, female to male ratio was 1 to 1.4, while mean age was 47 years for men and 48 years for women. Varies clinical features tend to have a chronic nature, resistant to commonly used conventional therapies. Therefore, it is crucial to identify specific treatment modalities that could completely help in the resolution of the lesions.
The present systematic review study summarizes and elaborates findings associated with its clinical presentation, differential diagnosis and treatment methods.
In a 15 year old male boy, childhood rosacea was diagnosed [15]. In this study, erythema was resolved after topical azaleic acid was used. It has shown effective outcome in the management of papulopustular rosacea as it inhibits microbial growth, regulates epidermal differentiation and diminishes the release of reactive oxygen species. This study highlights the adoption of approaches that can decrease the inflammatory response by reducing messenger RNA involved in progression of GR such as cathelicidin and kallikrein 5 messenger RNA. In another 61-yearold Chinese women, topical brimonidine gel (an alpha-adrenergic vasoconstrictor) greatly helped in reducing erythema Aronovich A, et al. and facial rashes. In recent times, there have been an increased use of brimonidine gel [18].
In one of the case report [17], patient had a long term history of atopic dermatitis. For past few years, tacrolimus ointment 0.1% was applied on face inconsistently. However, the new eruptions on the face increased when the cream was applied frequently and in increased quantity. Hence, tacrolimus ointment was discontinued. Her condition improved when multiple medication were prescribed. Similar findings have been reported in few other case reports, where topical tacrolimus resulted in various dermatologic side effects such as skin burning, pruritus, and erythema. This demonstrates that GR is associated with topical tacrolimus use.
Novel modalities have gained a lot of popularity due to their beneficial outcomes and minimal side-effects. In one patient [21], Pimecrolimus cream (1%) significantly improved the erythema and significantly reduced the papules. Conventional therapies may not be helpful in patients that are resistant to standard therapies. In such situations [21] for effective management of GR, pimecrolimus may be a good alternative. It is non-steroid calcineurin inhibitor which targets T-cells and mast cells, prevents the formation of inflammatory mediators and cytokines. The cream is safe and well-tolerated which makes it suitable for management of facial lesions in GR [21].
There is an urgent need to conduct quality research studies which are properly designed, consist of a large sample size and are followed for a sufficient time period in order to thoroughly understand this condition. With recent advances in our understanding, novel treatment modalities will provide an effective approach to manage GR.
GR is a clinical variant which is closely associated with rosacea, sharing common clinical signs and symptoms, along with presence of Demodex folliculorum and actinic elastosis. The present systematic review is the first study to define the wide spectrum of clinical characteristics of GR. The treatment interventions were identified and the effectiveness of each of these was evaluated. New therapies such as PDT, and low-level laser have shown beneficial results as compared to traditional methods. The impact of different medications should be assessed by conducting additional clinical trials that will help to bring a comparative view between rosacea patients. Furthermore, potential genetic susceptibility for this chronic cutaneous syndrome should be considered to understand the etiopathogenesis of GR. We hope our review will help in the development of effective therapeutic regimen which will result in beneficial outcomes in rosacea patients.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Aronovich A, Taieb Y, Segal R, Hodak E (2023) Granulomatous Rosacea: A Systematic Review of Clinical Presentations and Treatments. J Clin Exp Dermatol Res. 14:647.
Received: 29-Aug-2023, Manuscript No. JCEDR-23-25062; Editor assigned: 01-Sep-2023, Pre QC No. JCEDR-23-25062 (PQ); Reviewed: 15-Sep-2023, QC No. JCEDR-23-25062; Revised: 22-Sep-2023, Manuscript No. JCEDR-23-25062 (R); Published: 29-Sep-2023 , DOI: 10.35841/2155-9554.23.14.647
Copyright: © 2023 Aronovich A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.