Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2022)Volume 7, Issue 5
Introduction: Increasing data suggest that neonatal pain has long-term consequences. Non-pharmacological techniques (sucrose taste, pacifier suckling, breastfeeding) are effective and now widely used to combat minor neonatal pain. This study examined the analgesic effect of breast feeding and EBM during a painful procedure in healthy full-term newborns. Objective of the study: Analgesic effect of breast milk during a painful procedure in healthy full-term newborns.
Methodology: A randomized controlled trial was conducted in department of neonatology, BSMMU, Dhaka, Bangladesh. After taking consent from the parents/guardians, information was recorded in a data collection form. Healthy term neonates who visited the NICU during study period for routine investigation was the study population. Newborn who meet the inclusion criteria was randomized by lottery method. A randomized, controlled trial included healthy, full-term newborns born at the BSMMU. Infants were given 2.0 ml EBM 2 minutes before and throughout the procedure, the other group was given breast feeding and 1 group was given nothing. We assessed pain by a pain scale NIPS. Data was analyzed by statistical package for social sciences (SPSS) version 20.
Results: 167 valid data from 179 newborns who visited procedure room of NICU were enrolled randomly constitute the basis of this study. It has been found out that in breast feeding NIPS score is significantly lowest in comparison to EBM(p-value 0.003) and no intervention group(p-value 0.000) and NIPS score of EBM group(p-value 0.000) is lower than no intervention group.
Conclusion: This randomised controlled trial showed the effectiveness of breastfeeding and expressed breast milk on induced pain during a heel capillary prick in term and healthy neonates. We also noted the superiority of the analgesic effect of breastfeeding on expressed breast milk on the score pain during heel prick and phlebotomy.
Breast milk; Relieve pain; Skin; Venipuncture; Term neonates
Increasing data suggest that neonatal pain has long term effect both on growth and development. Pharmacologic interventions for minor pain are ineffective, and no pharmacological techniques (sucrose taste, pacifier suckling, breastfeeding) are effective and now widely used in the developed country but it is still a myth in our part of world. In fact this will be first study of its kind in Bangladesh. Pain is one of the very primary feeling that occurs to any individual be it of any age, size. Pain is a very recognized condition in adult and pediatric age group; a lot is being done for it. It is equally important in neonates. They do feel pain. So alleviation of pain is basic right of every individual regardless of their size and age. The International Association of the Study of Pain (IASP), [1] defines that pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage”. For preterm or ill term-neonates, the experience is very different. They are exposed to repeated procedural pain [2], extensive tissue damage resulting from surgery, or the invasiveness of endotracheal tubes placed for mechanical ventilation. Thus, at a time when most healthy term infants are learning about their environment and preterm infants are growing in the protective uterine environment, approximately 8% of neonates are coping with pain that, if left untreated, will interfere with normal growth and development [3]. Multiple sources of clinical and experimental evidence support the need for providing adequate analgesia/anesthesia for newborns who undergo invasive procedures (medical, surgical, diagnostic, and therapeutic) or develop conditions associated with a significant component of pain (e.g., skin burns, necrotizing enter colitis) [4]. Moreover, pain is a source of concern and distress for new parents and may disturb mother–infant bonding [5]. Pain reduction therapies are often underused for the numerous minor procedures that are part of routine medical and nursing care for neonates. Growing scientific and clinical evidence from both animal and human newborns points to the efficacy of natural, non-pharmacologic interventions to reduce pain due to minor procedures. It seems unbelievable how long it took the medical community to realize that newborns also feel pain. (Pain relief in neonates) [6]. It is the basic right of every individual, irrespective of age or size, to have alleviation of pain. Pain in newborn infants is a ubiquitous phenomenon. All newborns, even normal ones, will experience iatrogenic pain in the first days of life, commencing with vitamin K injection and blood collection for sugars, bilirubin or metabolic screening before discharge from the hospital. Neonates admitted to present day neonatal intensive care units (NICU) are constantly exposed to pain, discomfort or noxious stimuli of variable intensity for a variety of reasons. These include major surgical procedures, needle pricks for blood drawing and annulations. The painful situation may be short lived or chronic as in the case of necrotizing enter colitis and prolonged ventilation. Even apparently innocuous care giving procedures like diaper changes, daily weighing and removal of adhesive tape results in noxious stimuli. Furthermore, because neonates may not have memories of painful experiences, they were not thought capable of interpreting pain in a manner similar to that of adults. Electron microscopy and immunecyto chemical studies show that the development of various types of cells in the dorsal horn (along with their laminar arrangement, synaptic interconnections, and specific neurotransmitter vesicles) begins before 13 to 14 weeks of gestation and is completed by 30 weeks [7]. Lack of myelination has been used as an index of immaturity and often cited as reason for neonates to be incapable of feeling pain. Moreover, pain pathways to the spinal cord, brain stem and thalamus are completely militated by 30 weeks; whereas the thalamo-cortical pain fibers in the posterior limb of the internal capsule and corona radiate are myelinated by 37 weeks [8]. Infants as young as 25 weeks post menstrual age (PMA) have been shown to have cortical responses to noxious stimuli [9,10]. Near infrared spectroscopy studies in preterm infants from 28-36 weeks gestation undergoing tactile, non-noxious and painful stimuli (venipuncture) found that somatosensory cortical activation occurs bilaterally following unilateral stimulation. These suggest that neonates do have the required neuronal connections to experience the affective components of pain.
A randomized controlled trial was conducted in department of neonatology, BSMMU, Dhaka, Bangladesh. After taking consent from the parents/guardians, information was recorded in a data collection form. Healthy term neonates who visited the NICU during study period for routine investigation was the study population. Newborn who meet the inclusion criteria was randomized by lottery method. A randomized, controlled trial included healthy, full-term newborns born at the BSMMU. Infants were given 2.0 ml EBM 2 minutes before and throughout the procedure, the other group was given breast feeding and 1 group was given nothing. We assessed pain by a pain scale NIPS.
Inclusion criteria:
1. Healthy, full term newborns.
2. Parents who consented for the study
Exclusion criteria:
1. Preterm birth (<37 weeks’ completed gestation),
2. Birth weight <2.5 kg
3. Any APGAR score<6 (at 5 minutes)
4. Congenital abnormalities
5. Exposure to analgesics
Participants were healthy, full-term newborns born at the BSMMU. I randomly assigned each infant selected for the study into EBM, breast feeding or no intervention group by using a lottery method for randomization. For randomisation by lottery method I made 156 chits in 52 EBM group were written in the second 52 breast feeding group and the third 52 was for no intervention group. The lottery was picked by a parent; whatever group they pick they were assigned to that group and this was done till I got my desired number of sample and it was done by replacement method. This interventional randomized controlled trial was conducted among term neonates those who were delivered at BSMMU and attended neonatal OPD for routine procedure like heel lance prick, phlebotomy for different routine investigation such as thyroid function test, serum bilirubin, complete blood count. Then the babies who fulfilled the inclusion criteria were divided into three different groups randomly by lottery method namely EBM, Breast feeding and no intervention group. The parents were well explained regarding the study and its procedure and written informed consent were taken and neonates were enrolled in the study. For scoring of pain Neonatal Infant Pain Scale (NIPS) was used. All the babies were in care givers lap during entire procedure and while scoring of NIPS scale. The babies in breast feeding group received breast feeding 2 minute before and throughout the procedure, similarly the EBM group will receive 2 ml of Expressed breast milk 2 minutes before and throughout the procedure and the third group received nothing. The procedure was done by trained NICU nurse and the NIPS were scored by the principal investigator. The entire procedure was observed by one of the faculty member.
Data analysis
Data will be analyzed using the SPSS software for Windows (version 20.0) (SPSS Inc., Chicago, IL).Quantitative data will be expressed as mean (± SD) and qualitative data will be expressed as proportion. Analysis of variance (ANOVA) test will be done to see the relationship between NIPS score and EBM group, breast feeding group and No intervention group. Other’s test will be done as appropriate. P value of <0.05 will be considered as significant.
Operational definitions
Appropriate for gestational age (AGA): Birth weight between the 10th and 90th percentiles for the infant’s gestational age [11].
Gestational age: Will be calculated by total duration of pregnancy in weeks from first date of the last menstrual period (LMP) to birth of the baby.
Large for gestational age (LGA): Birth weight above the 90th percentile for the infant’s gestational age [11].
Low birth weight: Birth weight <2500 g.
Major congenital anomalies: The anomalies that are involved in major organs or system.
NICU: A facility in which a neonatologist provides primary care for the infant.
Small for gestational age (SGA): Birth weight below the 10th percentile for the infant’s gestational age [11].
Term: 37 completed weeks.
We enrolled 179 term neonates who were randomly selected into three groups namely breast feeding, expressed breast milk and no intervention group. 5 of the parents did not give consent and another 7 withdrew consent, so finally we had 167 neonates as sample. 59 of them were in breast feeding group and 56 and 52 in EBM and No Intervention group respectively (Figure 1).
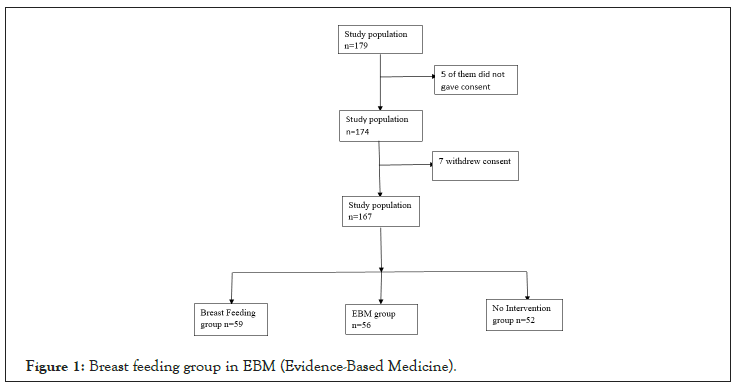
Figure 1: Breast feeding group in EBM (Evidence-Based Medicine).
The distribution of neonate’s gender and age wise was almost equal; almost half those in each group (Figures 2 and 3).
Figure 2: Gender distribution among neonates. Note: Half of the babies were girl child.

Figure 3: Gender distribution among neonates. Note: Half of the babies were girl child.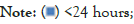

Most of the mother of enrolled neonates were multiparous, followed by prim parity and the least were grand multiparous. More than one third of the mothers recruited, had a graduate level of education, slightly less than one third had completed HSC and rest were SSC or below (Tables 1-4).
| Characteristics | Breast feeding n=59 | EBM n=56 | No intervention n=52 | |
|---|---|---|---|---|
| Gender | Male (n) | 24 | 31 | 27 |
| Female (n) | 35 | 25 | 25 | |
| Age | <24 hours (n) | 27 | 27 | 33 |
| >24 hours (n) | 32 | 29 | 19 | |
| Procedure | HLP* (n) | 17 | 18 | 24 |
| Phlebotomy (n) | 42 | 38 | 28 | |
| NIPS category | No pain (n) | 14 | 5 | 1 |
| Mild (n) | 43 | 37 | 6 | |
| Moderate (n) | 1 | 13 | 14 | |
| Severe (n) | 1 | 1 | 31 | |
| NIPS Score | 0 (n) | 13 | 5 | 1 |
| 1 (n) | 31 | 7 | 1 | |
| 2 (n) | 13 | 30 | 5 | |
| 3 (n) | 1 | 9 | 6 | |
| 4 (n) | 0 | 4 | 8 | |
| 5 (n) | 0 | 0 | 7 | |
| 6 (n) | 0 | 1 | 19 | |
| 7 (n) | 1 | 0 | 5 | |
Note: *HLP=Heel Lance Prick.
Table 1: Neonatal characteristics in breast feeding (N=179).
| Characteristics | Breast feeding n=59 | EBM n=56 | No intervention n=52 | |
|---|---|---|---|---|
| Gravida | Primi (n) | 21 | 24 | 15 |
| Multi (n) | 29 | 25 | 33 | |
| Grandmulti (n) | 9 | 7 | 4 | |
| Para | Primi (n) | 24 | 29 | 15 |
| Multi (n) | 30 | 21 | 33 | |
| Grandmulti (n) | 5 | 6 | 4 | |
| Education | Illiterate (n) | 3 | 3 | 1 |
| <class 5 (n) | 10 | 7 | 5 | |
| SSC (n) | 10 | 13 | 6 | |
| HSC (n) | 16 | 17 | 20 | |
| Graduate (n) | 20 | 16 | 20 | |
Table 2: Characteristics of breastfeeding in maternal and infant (N=179).
| Characteristics | Breast feeding n=59 | EBM n=56 | No intervention n=52 | P value | |
|---|---|---|---|---|---|
| Gender | Male n (%) | 24 (40.7) | 31 | 27 | 0.257 |
| Female n (%) | 35 (59.3) | 25 | 25 | ||
| Age | <24 hours n (%) | 27 (45.8) | 27 | 33 | 0.137 |
| >24 hours n (%) | 32 | 29 | 19 | ||
| Procedure | HLP* n (%) | 17 | 18 | 24 | 0.135 |
| Phlebotomy n (%) | 42 | 38 | 28 | ||
Note: There was no difference between the baseline characteristics of the neonates in different group.
Table 3: Baseline characteristics of neonates (N=179).
| Characteristics | Breast feeding n=59 | EBM n=56 | No intervention n=52 | P-value | |
|---|---|---|---|---|---|
| Gravida | Primi n (%) | 21 (35.6) | 24 (42.9) | 15 (28.8) | 0.308 |
| Multi n (%) | 29 (49.2) | 25 (44.6) | 33 (63.5) | ||
| Grandmulti n (%) | 9 (15.3) | 7 (12.5) | 4 (7.7) | ||
| Para | Primi n (%) | 24 (40.7) | 29 (51.8) | 15(28.8) | 0.116 |
| Multi n (%) | 30 (50.8) | 21 (37.5) | 33 (63.5) | ||
| Grandmulti n (%) | 5 (8.5) | 6 (10.7) | 4 (7.7) | ||
| Education | Illiterate n (%) | 3 (5.1) | 3 (5.4) | 1 (1.9) | 0.627 |
| <class 5 n (%) | 10 (16.9) | 7 (12.5) | 5 (9.6) | ||
| SSC n (%) | 10 (16.9) | 13 (23.2) | 6 (11.5) | ||
| HSC n (%) | 16 (27.1) | 17 (30.4) | 20 (38.5) | ||
| Graduate n (%) | 20 (33.9) | 16 (28.6) | 20 (38.5) | ||
| Mode of delivery | NVD n (%) | 10 (16.9) | 42 (21.4) | 9 (17.3) | 0.795 |
| LUCS n (%) | 49 (83.1) | 44 (78.6) | 43 (82.7) | ||
Note: There was no difference between the baseline characteristics of the mother in different group.
Table 4: Baseline characteristics of mothers (N=179).
Most of the babies that is two third of them had their vein punctured and rest of them underwent heel lance prick. Half of the neonates experienced mild pain while undergoing different procedure, least were in the group who experienced no pain (Figure 4).
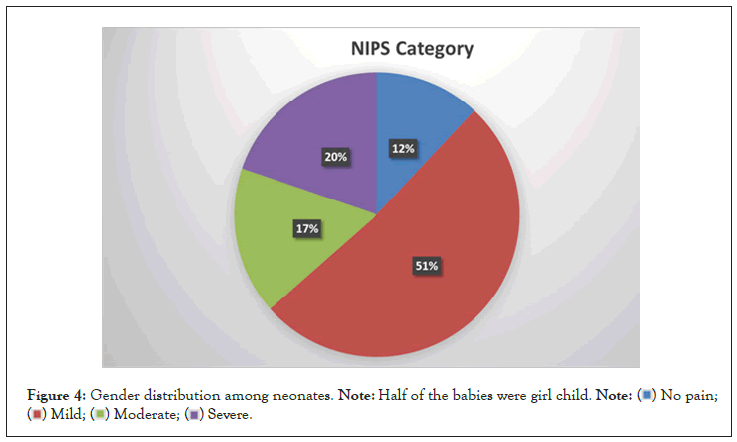
Figure 4: Gender distribution among neonates. Note: Half of the babies were girl child.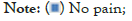
There was significant difference in the NIPS score among the three groups. The null hypothesis is rejected, which means there is significant difference among the three groups. It has been found out that in breast feeding NIPS score is lowest in comparison to EBM and no intervention group and NIPS score of EBM group is lower than no intervention group (Figure 5). Method of procedure had no significant effect on pain score by NIPS (Figure 6).
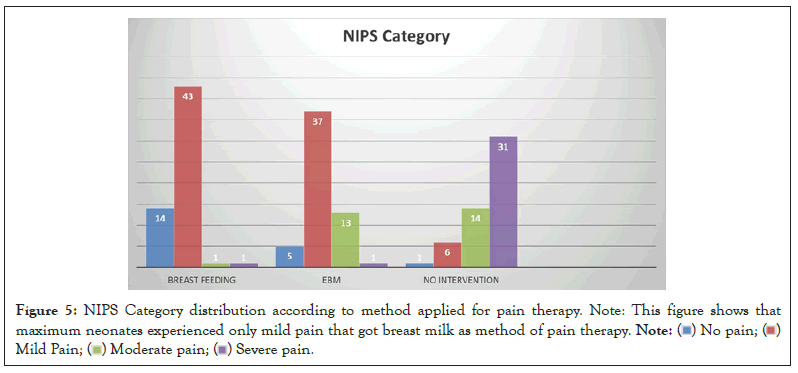
Figure 5: NIPS Category distribution according to method applied for pain therapy. Note: This figure shows that
maximum neonates experienced only mild pain that got breast milk as method of pain therapy.

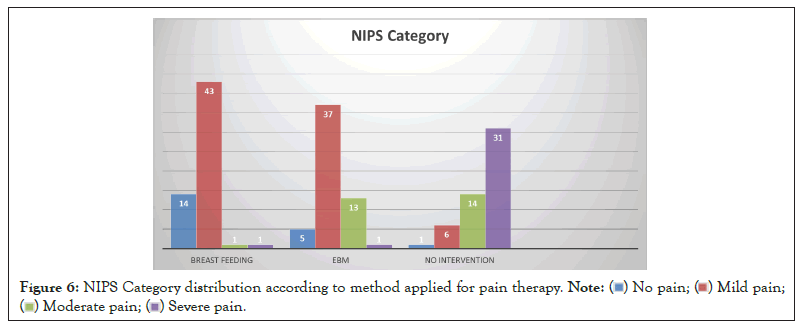
Figure 6: NIPS Category distribution according to method applied for pain therapy.

The analgesic mechanisms of breastfeeding and expressed milk are complex. The various components of breastfeeding, such as the taste of breast milk, suction, touch, smell or maternal warmth may have a role; however, opioid mechanism is not excluded. Comparing the two methods in our setting appeared important because mother is not always available. Using breast milk was advantageous because it is acceptable medically, socially and ethically and is always available. It does not interfere with exclusive breast feeding and we are not introducing anything foreign. This is the first study of its kind in Bangladesh. Babies who experience pain during neonatal period have neurodevelopmental and behavioral problem later in the life. There was significant difference in the NIPS score among the three groups. The null hypothesis is rejected, which means there is significant difference among the three groups. It has been found out that in breast feeding NIPS score is lowest in comparison to EBM and no intervention group and NIPS score of EBM group is lower than no intervention group. We could also find that method of procedure did not affect the NIPS. In fact, in the absence of analgesic treatment Osinaike et al., obtained a median pain score of 4, using the same scale, in newborns undergoing peripheral venipuncture [12]. The median pain score was 1.5 times higher in the 30% glucose solution group compared to the breastfeeding group. The significant difference noted reflects the analgesic superiority of breastfeeding on glucose 30% in case of heel prick in term neonates as found [13]. Also demonstrated the analgesic efficacy of the two methods by having a median pain score 3 times higher in the 30% glucose solution group compared to the breastfeeding group, but newborns in the 30% glucose group received the solution associated with the sucking of a pacifier [8]. In addition, it has been shown that nonnutritive sucking alone provides some analgesic effect in acute pain in term neonates [3]. The meta-analysis of Shah et al., on 10 studies evaluating the analgesic efficacy of breastfeeding in the newborn ultimately found a similar overall efficacy with 30% glucose solution [14]. Gray et al. have demonstrated the benefits of breastfeeding beyond the analgesic effect compared to 30% glucose solution. They found a reduction of grimaces and crying time, and a slight increase of heart rate during single painful procedures among breastfed neonates as compared to those on 30% glucose, reflecting less stress with breastfeeding [15]. Analysis of pain scores after procedure shows the analgesic efficacy of both methods on perception of pain and the return to calm, even though with a slight superiority of breastfeeding [16]. No maternal factor had an influence on the painful expression. In other studies, maternal age and parity were considered only as demographics characteristics [14,17,18]. However, a limitation of our study is that it was not possible to have video recording equipment at the completion of the painful procedure to assess pain scores by an external observer. In addition, we used a protocol of 30% glucose solution with different doses depending on the weight, which may have influenced the perception and expression of pain in neonates <3000 g.
• Single center study.
• There was no blinding.
This randomized controlled trial showed the effectiveness of breastfeeding and expressed breast milk on induced pain during a heel capillary prick in term and healthy neonates. We also noted the superiority of the analgesic effect of breastfeeding on expressed breast milk on the score pain during heel prick and phlebotomy. We thus recommend that the medical staff in charge of newborns: Preferentially use breastfeeding in the management of acute pain in term neonates undergoing a single painful procedure, and finally the use of expressed breast milk for the reduction of acute pain in term neonates only when breastfeeding is not possible.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Gupta SK, Karki B, Verma V, Jahan I, Shabuj MKH, Moni SC, et al. (2022) Feeding of Breast Milk to Relieve Pain During Skin and Venipuncture in Term Neonates: A Randomized Controlled Trial. Clin Pediatr. 7:217.
Received: 22-Aug-2022, Manuscript No. CPOA-22-16561; Editor assigned: 24-Aug-2022, Pre QC No. CPOA-22-16561 (PQ); Reviewed: 07-Sep-2022, QC No. CPOA-22-16561; Revised: 13-Sep-2022, Manuscript No. CPOA-22-16561 (R); Published: 22-Sep-2022 , DOI: 10.35248/2572-0775.22.7.217
Copyright: © 2022 Gupta SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.