Journal of Hematology & Thromboembolic Diseases
Open Access
ISSN: 2329-8790
ISSN: 2329-8790
Research - (2023)Volume 11, Issue 6
Background: Admissions are major events in the life journey of sicklers as it has the potential to jeopardise quality of life.
Method: We carried out a cross-sectional study over a 04 months period at the Mother and Child Center of the Chantal Biya Foundation (MCC-CBF) and Douala General Hospital (DGH). We assessed socio-demographic characteristics of both children and their caregivers, clinical factors, duration of hospital stay, respect of hospital appointments and the outcome hospital admissions and 30-day readmissions in the previous year. The factors associated with admissions and readmissions were determined using the chi square test or fichers exact test were appropriate. The threshold of significance was p<0.05.
Results: Overall, 200 children were included in the study. Most were females n=106 (53%). A majority were admitted n=117 (58.5%) and few n=12 (10.3%) were readmitted. A late age at diagnosis (OR=0.40, 95% CI: 0.21-0.76, P=0.005), being polytransfused (OR=2.70, 95% CI: 1.31-5.54; P=0.007) and respect of hospital appointments (OR=2.20, 95% CI: 1.10-4.40; P=0.027) were significantly associated with admissions. Whereas adolescence (OR=6.36, 95% CI: 1.63-27.89; P=0.014) and a long duration of hospital stay (OR=7.69, 95% CI: 1.62-36.69; P=0.010) were significantly associated with readmissions.
Conclusion: There are potentially modifiable and non-modifiable factors associated with admissions and readmissions. Special attention need to be paid on the care of sicklers who are polytransfused and those in the adolescent period.
Admissions; 30-day readmission; Sickle cell anaemia; Cameroon
CME-FCB: Mother and Child Center of the Chantal Biya Foundation; DGH: Douala General Hospital; SCA: Sickle Cell Anaemia; SCD: Sickle Cell Disease
Sickle Cell Disease (SCD) is a major public health problem [1]. It is a group of inherited erythrocyte disorders which results from a single substitution of glutamic acid for valine at position six of beta globin polypeptide chain found on chromosome 11 [2]. Sickle Cell Anaemia (SCA), Homozygous HbS (Hbss) is the most common and most severe form of SCD [3]. Recent studies estimates suggest that 300,000 children are born with SCD worldwide every year and three-quarters of these births occur in Sub-Saharan Africa [4].In Cameroon, two recent studies of neonatal screening revealed a prevalence of 13.6% for Sickle Cell Trait (SCT), and 0.6% for Sickle Cell Disease [5,6]. It is a chronic illness with acute and chronic necessitating frequent hospital visits [7,8].
Hospital admissions and readmissions among this group of patients put a tremendous strain on limited financial resources of most families with SCA [9]. In the United States, hospital admissions and readmissions are very frequent for individuals with SCD, with approximately 60,000 annual hospital admissions, of which 90% are for acute pain treatment [10]. Thirty day readmission frequency is as high as between 19% and 33% among patients with SCD [11,12]. Low level of education, no outpatient follow-ups, public insurance type, and being an adult are some modifiable and non-modifiable factors that were identified to be associated with these high readmission rates in United States [11,13,14]. In Kenya, hospital admission frequency among these patients was high at 73.57% of which vasoocclusive crisis was identified as the most common cause of hospitalisations [15].
In Cameroon, a study carried out at Mother and Child Centre of the Chantal Biya Foundation, revealed a high yearly admission frequency of 45.2% among sicklers [16]. Anaemic syndrome, acute painful crisis, and septicaemia were identified as the most common causes of admissions [7,17]. Despite high admission frequencies reported worldwide and in our country, to the best of our knowledge, there is paucity of data on readmission frequencies as well as the factors associated with admissions and readmissions among sicklers in Cameroon.
Study design and setting
We carried out a cross-sectional study from March to June 2020 at the sickle cell unit of the Mother and Child Center of the Chantal Biya Foundation (MCC-CBF), and the paediatric unit and haematological outpatient consultation of the Douala General Hospital (DGH).
The Sickle Cell Unit at MCC-CBF is made of 04 admission rooms, with a total bed capacity of 11 beds. They receive an average of 45 patients monthly from all regions of the country.
The Douala General hospital is a tertiary and referral hospital. It offers a variety of specialised services in which we count haematology and paediatrics. These both play an active role in the management of Sickle Cell Disease. The average number of sicklers at haematologist consultation is 5 weekly.
Participants
We included all children (age<18years) with a confirmed diagnosis of SCA on haemoglobin electrophoresis and their caregivers while we excluded caregivers who did not give their assent and children newly diagnosed in 2020.
Sampling and data collection procedure
Participants were selected using consecutive non probability sampling. We pre-tested our questionnaire on a group of 10 patients prior to the commencement of data collection. The patients who took part in the pre-test were excluded from the study.
Questions were asked to the caregivers in their first language and responses were filled by the principal investigator.
Outcome variables
Our main outcomes were admissions and 30-days readmissions at our study sites in the year 2019.
Independent variables
The following variables were evaluated for association with admissions and 30-days readmissions among children with SCA: Demographic information of the children.
Age(years) and gender(male/female); Caregiver information: marital status (single/married), level of education, residence (urban/rural); Clinical history; age of diagnosis of SCA (months); history of blood transfusion; drinking water habits; duration of hospital stay; respect of clinic appointments.
Bias
The accuracy of self-reported admissions and readmissions and their reasons were compared to the medical health record of our participants in order to limit recall bias.
Sample size calculation
The sample size was calculated at 107 sicklers, using the prevalence of SCD in Cameroon [5]. This was estimated using the Cochran formula.
Operational terms
Hospitalisation was any admission into MCC-CBF or DGH within the year 2019, while a 30 day readmission was an admission to MCC-CBF or DGH within 30 days of discharge from these hospitals in 2019. Drinking water habit was categorised as good (≥ 2 Litres) and poor (<2 litres) according to the Centre of Disease Control and Prevention recommendations on daily water intake for a sickler [18]. Frequency of past blood transfusion was categorised as polytransfused when he/she had received ≥ 2 blood transfusions in the previous year [16].
Statistical methods and data analysis
Data collected were entered and analysed using EPI info. Results were presented as means and Standard Deviation (SD) for continuous variables and frequencies and percentages for categorical variables. At bivariate analysis, we used the Chi square/Fisher exact test where appropriate test to obtain crudes Odd Ratios (OR) of factors associated with admissions and 30- days readmissions. Multivariate logistic regression was used to identify independent associations with admissions and 30-days readmissions. This was presented as adjusted odd ratios along with their p-values. A p-value of <0.05 was used as cut off for statistical significance.
Baseline characteristics of the population
A total of 220 children and their caregivers completed the survey. After excluding patients that met our exclusion criteria, our final sample for analysis included 200 children and their caregivers. The mean age of children was 8.01 ± 4.22 years and the mean age at diagnosis was 31.93 ± 30.97 months. Most of the children were female (53%). Majority of caregivers were married (64%) and (73%) had lower level of education. Almost all participants lived in urban (86.5%). Tables 1 and 2 summarises the baseline characteristics of the children with SCA and their care givers respectively.
| Variables children | Overall | Male | Female |
|---|---|---|---|
| n(%) | 200 | 94(47) | 106(53) |
| Mean age, year, (SD) | 8.01(4.22) | 7.34(4.13) | 8.59(4.23) |
| Mean Age at diagnosis,months, (SD) | 31.93(30.97) | 29.80(29.94) | 33.82(31.87) |
| Mean quantity of drinking water, litres, (SD) | 1.81(0.86) | 1.77(0.85) | 1.84(0.87) |
| Past history of blood transfusion n (%) | Yes; n=162(81) | 78(8.98) | 84(79.25) |
| No; n=38(19) | 16(17.02) | 22(20.75) | |
| Respect of appointment n (%) | Yes; n=143(71.5) | 63(67.02) | 80(75.47) |
| No; n=57(28.5) | 31(32.93) | 26(24.53) |
Table 1: Socio-demographic characteristics of children with SCA.
| Variables caregivers | Frequency(n=200) | Proportion (%) |
|---|---|---|
| Marital status | ||
| Married | 128 | 64 |
| Single | 72 | 36 |
| Occupation | ||
| Employed | 150 | 75 |
| Unemployed | 50 | 25 |
| Residence | ||
| Urban | 173 | 86.5 |
| Rural | 27 | 13.5 |
| Level of education | ||
| Lower education | 146 | 73 |
| Higher education | 54 | 27 |
Table 2: Socio-demographic characteristics of caregivers of children with SCA.
Frequency of previous admission and 30-day readmission
A majority of the children were admitted in the previous year (n=117; 58.5%) and fewer were readmitted (n=12; 10.3%) (Figures 1 and 2).

Figure 1:Frequency of admissions. Note: (  ): Admitted; (
): Admitted; (  ): Not admitted.
): Not admitted.
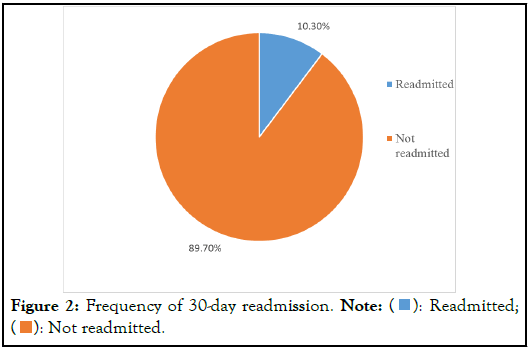
Figure 2:FFrequency of 30-day readmission. Note: ( ): Readmitted;
(
): Readmitted;
( ): Not readmitted.
): Not readmitted.
Factors associated with hospitalisations
On bivariate analysis a late age at diagnosis, a history of blood transfusion and being polytransfused, were significantly associated with admissions.
A late age at diagnosis (adjusted Odds Ratio (aOR) 0.36; 95% CI: 0.20-0.66: p<0.001) being polytransfused (OR 2.81; 95% CI: 1.43-5.50: p=0.02) and Missed clinic were predictive factors of admission (Table 3).
| Variables | OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-value |
|---|---|---|---|---|
| Age(years) | ||||
| = 11 | 0.85(0.46-1.56) | 0.60 | - | - |
| Gender | ||||
| Female | 0.61(0.34-1.07) | 0.083 | 0.68(0.36-1.26) | 0.215 |
| Marital status | ||||
| Married | 1.21(0.67-2.17) | 0.526 | - | - |
| Occupation | ||||
| Employed | 1.28(0.67-2.43) | 0.456 | - | - |
| Level of education | ||||
| Lower education | 0.86(0.46-1.63) | 0.649 | - | - |
| Residence | ||||
| Urban | 1.04(0.45-2.36) | 0.931 | - | |
| Age at diagnosis(months) | ||||
| >12 | 0.36(0.20-0.66) | <0.001 | 0.40(0.21-0.76) | 0.005 |
| Past history of blood transfusion | ||||
| Yes | 2.60(1.26-5.38) | 0.008 | 0.25(0.04-1.55) | 0.136 |
| Number of blood transfusions | ||||
| >2 | 2.81(1.43-5.50) | 0.002 | 2.70(1.31-5.54) | 0.007 |
| Quantity of drinking water(litres) | ||||
| = 2 | 1.17(0.66-2.07) | 0.589 | - | - |
| Respect of clinical appointment | ||||
| Yes | 0.58(0.31-1.08) | 0.08 | 2.20(1.10-4.40) | 0.027 |
Table 3: Bivariate analysis and multivariate analysis of factors associated with admissions.
Factors associated with 30-day readmission
Adolescence (aOR 7.83; 95% CI: 1.63-37.44: p=0.010) and a long length of hospital stay (OR 7.30; 95% CI: 1.43-37.29: p=0.017) were significantly associated with readmissions on bivariate analysis as well as multivariate analysis (Table 4).
| Variables | OR (95% CI) | p-Value | Adjusted OR (95%CI) | p-value |
|---|---|---|---|---|
| Age(years) | ||||
| = 11 | 6.08(1.69-21.84) | 0.005 | 6.36(1.45-27.89) | 0.014 |
| Gender | ||||
| Female | 2.38(0.67-8.37) | 0.226 | - | - |
| Marital status | ||||
| Married | 2.84(0.59-13.62) | 0.216 | - | - |
| Occupation | ||||
| Employed | 0.37(0.11-1.28) | 0.107 | 0.62(0.13-3.04) | 0.553 |
| Level of education | ||||
| Lower education | 0.86(0.46-1.63) | 0.738 | - | - |
| Residence | ||||
| Urban | 0.55(0.07-4.54) | 1 | - | - |
| Age at diagnosis(months) | ||||
| >12 | 0.73(0.22-2.44) | 0.606 | - | - |
| Past history of blood transfusion | ||||
| Yes | N/A | 0.343 | - | - |
| Number of blood transfusions | ||||
| >2 | 2.59(0.53-12.61) | 0.327 | - | - |
| Quantity of drinking water(litres) | ||||
| = 2 | 2.88(0.82-10.18) | 0.125 | 2.23(0.49-10.14) | 0.3 |
| Respect of appointment | ||||
| No | 0.61(0.13-2.95) | 0.728 | - | - |
| Long length of hospital stay | ||||
| >7 days | 6.55(1.66-25.76) | 0.007 | 7.69(1.62-36.59) | 0.01 |
| Admitted and transfused | ||||
| Yes | 3.06(0.78-11.93) | 0.13 | 0.42(0.82-2.11) | 0.29 |
Table 4: Bivariate and multivariate analysis of factors associated with 30-days readmissions.
The relationship between health care cost and admissions and readmissions among sicklers is directly proportional and real, therefore this worsens the burden of this public health issue. The objectives of this study were to determine the frequencies of admissions and 30 day readmissions, and identify the factors associated with admissions and readmissions among sicklers in two hospitals in Cameroon.
The frequency of previous admissions and 30-day readmissions in 2019 was 58.5% and 10.3% respectively in our study. This finding was similar to the admission frequency reported by Chetcha, et al. in Cameroon (45.2%), and Ogol, et al. in Kenya (73.57%) [15,16].
However, the readmission frequency obtained in our study was lower than in prior studies reported by Sobota, et al. in United States (17%) and by Jencks, et al. in United States (19.6%) [19,20]. The high standard of care in the United States compared to our setting could explain this difference observed, given the fact that they have more specialised centers for the management of Sickle Cell Disease. Futhermore, both studies were multicentre retrospective studies, while our study was carried out in two hospitals and the short study duration could not enable us to sample all previous admissions and readmissions in 2019.
Polytransfussion was a predictive factor for admissions. To the best of our literature search, there is paucity of data to support this finding. Children with SCA who regularly require blood transfusion, are usually the sick and unstable ones who have underlying complications of the disease such as chronic anaemia, infections, vaso-occlusive crisis, and stroke necessitating admissions. Thus, explaining our finding. Moreso, blood transfusion is not without risks. Blood transfusions among sicklers have been associated with complications such as infections, iron overload, and alloimunization which might motivate an admission [21-24]. This result highlights the importance that special care should be paid on sicklers who are polytransfused. Further studies are encouraged to evaluate a causal effect association between polytransfusion and admission among sicklers.
We also found that, children diagnosed after the age of 12 months had less admission. This could be explained by the fact that these groups of children probably had a persistently high level of fetal haemoglobin. This therefore protected them from having frequent crisis hence fewer admissions. Moreso most of the children with SCD related complications in our study were those age at diagnosis less than 12 months therefore supporting the possibility of persistently elevated fetal haemoglobin in the opposite group. However further studies are needed to establish the true correlation between the age, biological parameters of Sicklers (i.e. level of fetal haemoglobin) and admissions.
Respect of clinical appointment was significantly associated with more admissions. Clinical appointments are very important component in the care of SCD because, it enables the early identification and management of health issues related to SCD or not [25,26]. Our finding could be explained by the fact that, attending an appointment fixed by the primary care physicians implies he will be able to identify any emergent health issues which might warrant an admission for proper care and follow up hence more admissions. However, our finding is in contrast with reports from Cronin, et al., and Frei Jones, et al. in United States who reported respect of outpatient attendance to be implicated with less admissions [13,25]. This difference could be explained by a difference in methodologies. In these studies, an outpatient appointment was a follow up visit within 30 days or 14 days following a discharge which was attended. Where as in our study, an outpatient appointment was considered as any follow up visit respected over the previous year.
Adolescence and a long length of hospital stay were predictive factors for 30 day readmission. Adolescence were more likely to be readmitted in our study, which is accordance with the available literature [20,25,27]. The increased likelihood of readmission with increasing age has been demonstrated with complications of aging [20,25,28]. Age is not a modifiable factor, however, by identifying patients at higher risk for readmissions, clinicians can better focus interventions designed to reduce preventable readmissions.
Duration of hospital stay greater than our mean length of stay (6.7 ± 2.77 days), was associated with more readmissions. This could be explained by the fact that reasons for admissions which required a hospital stay of greater than 7 days were more severe in nature, and had a greater chance of recurrence. This highlights the importance of the establishment and implementation of clinical guidelines for the detection and management of Sickle Cell Disease related complications. Although our findings are important they should be considered and interpreted in the light of some limitations: (1) the short study duration could not allow us to sample all admissions and readmissions in our study sites in 2019 which could be improved in a multicentre prospective study. (2) List of factors potentially associated with admissions and readmissions is by no means exhaustive and (3) the lack of biological parameters which is a strong parameter to understand the relationship between age at diagnosis of SCA, and frequencies of admissions and readmissions.
Despite these limitations, to the best of our literature search this is the first study to provide evidence based information on the frequency of admission and readmission as well as factors associated with these among children with SCA in two hospitals in Cameroon. The observed high frequency of admission and few readmissions highlight the necessity for a national harmonised management care for these patients with emphasis paid on preventive counselling especially in groups at risk. However, the responsibility ensuring adequate management and follow up of these patients does not rest on healthcare personnel as evidence suggest the role of a robust family support to be invaluable.
The frequency of admissions and 30-days readmissions among sicklers are high in our setting. Poly transfusion, a late age at diagnosis and attending clinic appointments were significantly associated with admissions, while adolescence and long hospital stay were significantly associated with readmissions. Special attention should be paid on the care of sicklers who are polytransfused and adolescent.
The authors would like to thank the staff of the Sickle cell unit of the Mother and Child Center of the Chantal Biya Foundation as well as the staff of the Pediatrics and Hematological units of the Douala General Hospital for their cooperation and assistance in data collection for the study. We also thank the individuals with SCA and their care givers who participated in the study.
TSLA and MEM conceived and designed the study; TSLA collected data and MEM, NDTE, and FY supervised data collection; TSLA and MEM analysed data; TSLA drafted the manuscript; MEM, NDT, and FY substantively revised the manuscript. All authors read and approved the final manuscript.
This research did not receive fund from any organization.
The datasets used for this study are available from the corresponding author on reasonable request.
Not applicable.
The authors declare that they have no competing interests.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Armelle TSL, Mungyeh ME, Yolande F, Tsakeu ND (2023) Factors Associated with Hospitalisations and 30-Day Readmissions among Patients with Sickle Cell Anemia in Two Hospitals in Cameroon. J Hematol Thrombo Dis.11:553.
Received: 01-Jun-2023, Manuscript No. JHTD-23-25268; Editor assigned: 05-Jun-2023, Pre QC No. JHTD-23-25268 (PQ); Reviewed: 19-Jun-2023, QC No. JHTD-23-25268; Revised: 26-Jun-2023, Manuscript No. JHTD-23-25268 (R); Published: 03-Jul-2023 , DOI: 10.35248/2329-8790.23.11.553
Copyright: © 2023 Armelle TSL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.