Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research - (2023)Volume 14, Issue 4
The classic lipolytic injection technique involves multiple punctures, which causes extreme discomfort due to the needling and the formation of hematomas. We describe a technique in which the lipolytic is delivered to the adipose tissue through cannulas with a blunt tip, minimizing the number of punctures and, therefore, pain and bruising. In addition, one of the most feared complications of the procedure is skin necrosis, caused by intravascular or intradermal injection. The use of blunt tip cannulas minimizes intravascular injection risks and facilitates subcutaneous injection, as the device does not slide easily through the dermis. We have used this application technique with excellent results and without major complications. Because it is less painful and has a more pleasant post-procedure, we have obtained lower rates of treatment abandonment and, therefore, better final results.
Lipolytics; Dermis; Cannulas
The use of lipolytics to reduce small accumulations of fat is already well documented. Despite being formally authorized only for the treatment of Submental Fat (SUB), there are numerous reports of good results in other areas [1-8]. The most established agents are Deoxycholic Acid (DA) and Phosphatidylcholine (PPC), however, other agents with lipolytic potential have also been described, such as caffeine, melilotus, carnitine, yohimbine, aminophylline and isoproterenol, among others [9-11]. The application technique classically described involves the delivery of small aliquots of the active agent in the target tissue, through multiple punctures [12,13]. This technique, although effective, as it involves multiple injections, is quite uncomfortable, in addition to allowing the formation of numerous hematomas and intensifying post-procedure pain and swelling. Besides that, the large number of punctures favors technical failure.
Finally, one of the most feared complications in relation to DA injection specifically is skin necrosis, primarily associated with injection of the agent intravascularly or superficially in the dermis [14]. Injection in an inappropriate site can also lead to muscle and nerve necrosis [15]. The most reported neural lesion is the one in which the marginal mandibular nerve is affected, when injections are made to treat SUB [16]. We believe that the use of the cannula, which reduced the number of punctures, minimized the risk of intravascular injection and facilitated exclusive injection into the adipose tissue, made the procedure safer. We have developed a simple technique for applying facial and body lipolytics through cannulas, which is very well tolerated by patients, with excellent results and without major complications.
We applied lipolytics in different areas of 35 patients, of both sexes, aged between 28 and 48 years, in the last 12 months. We did treat the SUB, the Nasolabial (NL) and Jowl (JWL) fat pads, abdomen, flanks and pubic mound. Due to the cytotoxic potential of DA, for facial treatments, we used a mixture of noncytolytic substances, whose main agents were caffeine and carnitine, which activate lipolysis through non-ablative mechanisms. In the SUB and other areas, the association of DA with Phosphatidylcholine (PPC) was used.
We follow the protocol below for all body areas:
• Disinfection and marking of the skin over the accumulation of fat with dots 1 cm apart.
• Injection of punctual anesthetic points with 1% lidocaine, 1 cm from the outer edge of the area marking.
• Incision with a 24G needle, for entry of a 25G/5 cm, semiflexible, blunt-tipped cannula in the anesthetized points. As many entry ports as necessary would be performed for the cannula to reach all marked points. In general, for larger areas, a maximum of 4 is sufficient.
• Introduction of the cannula into the adipose tissue and delivery of small punctual aliquots of the lipolytic (0.05-0.1 ml) under each marked point.
Regarding body areas, special attention should be given to the suprapubic region, whose marking should start at a minimum distance of 0.5 cm, above the anterior vulvar commissure, to avoid any injury to the clitoral dorsal nerve (Figure 1).
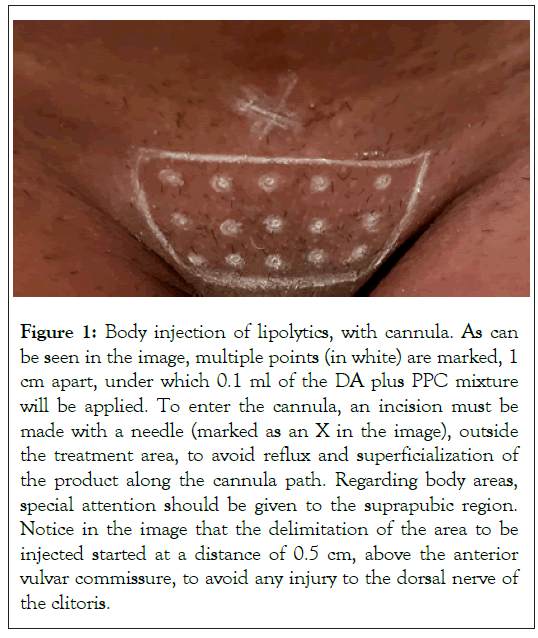
Figure 1: Body injection of lipolytics, with cannula. As can be seen in the image, multiple points (in white) are marked, 1 cm apart, under which 0.1 ml of the DA plus PPC mixture will be applied. To enter the cannula, an incision must be made with a needle (marked as an X in the image), outside the treatment area, to avoid reflux and superficialization of the product along the cannula path. Regarding body areas, special attention should be given to the suprapubic region. Notice in the image that the delimitation of the area to be injected started at a distance of 0.5 cm, above the anterior vulvar commissure, to avoid any injury to the dorsal nerve of the clitoris.
For the injection of lipolytics in the SUB, before marking the injection site, the patient is asked to contract the platysma so that the fat, superficial to the muscle, can be palpated. From then on, the area to be treated will be delimited by the Submental Fold (SMF) anteriorly, by the Hyoid Bone (HB) posteriorly and by a bilateral lateral line that continues from the Labiomental Fold (LMF). If necessary, the lateral limits of the injection can be expanded, using a line that connects the anterior border of the Masseter Muscle (MM) to the lateral limit of the HB. We maintain a minimum distance of 1.0 cm from the Lower Border of the Mandible (LMB), mainly on the anterior border of the MM, through which the marginal Mandibular Nerve (MN) passes. We mark multiple dots with a distance of 1.0 cm and make the incision for the entry of the cannula in the midline of mentus (Figures 2 and 3).
Figure 2: Treatment of Submental Area (SUB). For the treatment of SUB, the area will be delimited by the Submental Fold (SMF) anteriorly, by the Hyoid Bone (HB) posteriorly, and by a bilateral lateral line that continues from the Labiomental Fold (LMF). We maintain a minimum distance of 1.0 cm from the Lower Border of the Mandible (LMB) to avoid injuries to the mandibular Marginal Nerve (MN). If necessary, as can be seen in the image, the lateral limits of the injection can be enlarged, using a line that connects the anterior border of the Masseter Muscle (MM) to the lateral limit of the HB. We marked multiple points (in black in the image) with a distance of 1.0 cm and made the incision for the entry of the cannula in the midline of the mentus (marked in X in the image).
Figure 3: Lipolytic injection in the SUB, with cannula. Note that the cannula is positioned superficially, reaching the preplatysmal fat. In order to avoid accumulation of product and irregularities, we do not do retroinjection, but the application of 0.1 ml of the AD plus PPC mixture, mimicking the classic technique of multiple punctures.
For injection into the JWL, we marked an area that had the anterior limit of the LMF, posterior the anterior border of the MM and superior a continuous line between the Mental Sulcus (MS) and the Ipsilateral Earlobe (EL). We maintain a minimum distance of 0.5 cm from the anterior limit, so as not to deepen the LMF, and of 1.0 cm from the LMB. The injection will be performed within these limits, in a grid, with points every 1cm if DA is injected [17,18] and every 0.5 cm if non-cytotoxic lipolytics are used (Figure 4).
Note that we maintain a minimum distance of 0.5 cm from the anterior limit, in order not to deepen the LMF, and 1.0 cm from the LMB, to protect the marginal mandibular nerve. The injection will be performed within these limits, in a grid, with points every 1 cm if DA is injected and every 0.5 cm if noncytotoxic lipolytics are used. For injection into the NL, we marked multiple points, with a distance of 0.5 cm, avoiding injecting at a distance of less than 0.5 cm from the upper and lower edges of the NL to avoid deepening the Lacrimal (LF) and Nasolabial (NLF) folds. For NL and JWL injections, we used the intersection between a line running down from the outer corner of the eye towards the mandible and a line between the corner of the lip and the earlobe as the incision point for the cannula entry (X mark on the image).
For injection into the NL, we marked multiple points, with a distance of 0.5 cm, avoiding injecting at a distance of less than 0.5 cm from the upper and lower edges of the NL to avoid deepening the Lacrimal (LF) and Nasolabial (NLF) folds (Figure 4).
Figure 4: Delimitation of the injection areas in the Jowl (JWL) and Nasolabial (NL) fat pads. For the JWL injection, the area has the anterior boundary of the Labiomental Fold (LMF), posteriorly the anterior border of the Masseter Muscle (MM) and superiorly a continuous line between the Mental Sulcus (MS) and the Ipsilateral Earlobe (EL).
Special attention should be given to the presence of the infraorbital foramen, classically described as being 1 cm below the inferior orbital bone border, medially or over the pupillary midline. Injections in this area should remain in superficial subcutaneous (Figure 5).
Figure 5: Superficial positioning of the cannula for injection in the Nasolabial fat pad (NL). Extra care must be taken to keep the cannula in the NL, which is a superficial fat pad, to avoid damage to infraorbital vessels and nerves.
For NL and JWL injections, we used the intersection between a line that descends from the outer corner of the eye towards the mandible and a line between the corner of the lip and the earlobe as an incision point for the cannula to enter (Figure 4). We reduced the distance between the points from 1 cm to 0.5 cm when using non-cytotoxic products to increase the effectiveness of the treatment. It is also important to emphasize that we always avoid the association of lidocaine to lipolytics, as the anesthetic decreases the action of the agents [10].
The results were evaluated by photographic documentation and by the Subject Self Rating Scale questionnaire (SSRS) [12] (Table 1). All patients showed satisfaction with the results obtained, according to the SSRS (Table 2) and showed a decrease in fat, perceptible by photographic documentation, after 30 days of 2 treatment sessions, with an interval of 1 month (Figures 6-10) with all injected substances, despite the results obtained with the DA/PPC association being more expressive.
| Variables | n | % | |
|---|---|---|---|
| Gender | Male | 17 | 48.6 |
| Female | 18 | 51.4 | |
| Treated area | Abdomen | 8 | 22.9 |
| Flanks | 3 | 8.6 | |
| JWL | 3 | 8.6 | |
| NL | 7 | 20 | |
| Pubic | 3 | 8.6 | |
| SUB | 11 | 31.4 | |
| Drug | CC | 10 | 28.6 |
| DA, PPC | 25 | 71.4 |
Table 1: Characteristics of patients (n=35).
| Age | Drug quantity (mL) | SSRS pre treatment | SSRS after 30 days of 2nd session | |
|---|---|---|---|---|
| Minimum | 27 | 2.0 | 0.0 | 3.0 |
| Maximum | 48 | 10 | 2.0 | 5.0 |
| Median | 37 | 2.0 | 1.0 | 4.0 |
| 1st quartile | 32 | 2.0 | 0.0 | 3.0 |
| 3rd quartile | 44 | 5.0 | 1.0 | 4.0 |
| Mean | 37.7 | 3.3 | 0.8 | 3.8 |
| Standard deviation | 6.6 | 2.1 | 0.7 | 0.7 |
Note: p-value<0.0001* was statistically significant difference (Wilcoxon signed-rank test).
Table 2: Characterization of patients (n=35) according to the SRSS (Subject Self Rating Scale) for the assessment of patient satisfaction.
Figure 6: Upper image before and lower image after 2 injection sessions of non-cytotoxic lipolytics, with cannula, in the Nasolabial fat pad (NL). We asked the patient to place her chin against the sternum to highlight the NLs. Realize that there is a discreet result with non-ablative lipolytics, not comparable to can reach with cytotoxic lipolytics, but capable of bringing aesthetic benefit to patients, in a safe way, in risk areas such as the NL due to the presence of infraorbital vessels and nerves.
Figure 7: Image on the left before and image on the right after 2 injection sessions of nonablative lipolytics in the Jowls (JWL) and cytotoxic agents in the Submental fat (SUB). Notice the improvement in the facial contour, with the reduction of fat in the SUB and JWL.
Figure 8: Image on the left before and image on the right after 2 injection sessions of cytotoxic lipolytics in the Submental fat (SUB). Notice the improvement in the facial contour, with the reduction of fat in the SUB.
Figure 9: Image on the left before and on the right after 2 sessions of cytotoxic lipolytics in the abdomen. Previously submitted to abdominal liposuction, the patient remained dissatisfied with a slight accumulation of peri-umbilical fat, successfully treated with ablative lipolytics.
Figure 10: Mean and standard deviation (n=35 patients) of according to the SRSS (Subject Self Rating Scale) for the assessment of patient satisfaction. Note: p<0.0001* was statistically significant difference.
Table 1 shows that data from n=35 patients who answered the SSRS Questionnaire. Most patients are female (51.4%). The most frequent treated area was SUB (31.4%). The drugs used were CC (28.6%) and DA PPC (71.4%).
Table 2 shows how the sample data (n=35 patients) who answered the “Subject Self Rating Scale (SSRS)” questionnaire were analyzed. After being analyzed, we obtained the following results: The age of the participants ranged between 27 and 48 years old with a mean of 37.7 ± 6.6 years old. The Drug quantity (mL) ranged between 2.0 and 10.0 mL with a mean of 3.3 ± 2.1 years. The SSRS pre-treatment presented scores in the range between 0.0 and 2.0 points with a mean of 0.8 ± 0.7 years. The SSRS after 30 days of 2nd session ranged between 3.0 and 5.0 points with an average of 3.8 ± 0.7 years. The comparison between SSRS pre-treatment (mean=0.8) and SSRS after 30 days of 2nd session (mean=3.8) resulted in p-value <0.0001* (statistically significant difference).
The only reported complications were discrete hematomas at the cannula entry ports. When DA/PPC was injected, there was still a burning sensation at the time of application, in addition to mild discomfort and swelling after the procedure, which resolved spontaneously within 72 hours.
Although the injection of lipolytics is a simple and effective treatment with a low rate of complications, the conventional application technique has not been modernized, remaining are very uncomfortable for patients. DA is currently considered the first-choice injectable drug for SUB reduction, representing a minimally invasive alternative to liposuction for moderate SUB [1]. We chose to use it in association with PPC not only in reducing the double chin, but in all non-facial treatment areas.
The association of DA with PPC is interesting because, although the isolated use of DA is effective, its combination with PPC decreases edema and accelerates the resolution of post-procedure inflammation. It is believed that DA is actually the effective lipolytic agent, however PPC would be useful to obtain a posterior emulsification of the fat, helping in the transport of free fatty acids after the breakdown [19-21].
Non-cytotoxic lipolytic agents have already been reported as efficient in reducing small fat accumulations. Among these actives, we did inject caffeine, which stimulates lipolysis by increasing intracellular cAMP [19,22] and L-Carnitine, which induces the expression of lipolytic genes and the suppression of adipogenic genes [23]. Caffeine should be used with caution due to reports of intoxication described in the literature [24]. Lcarnitine, in turn, had its intradermal application related to the onset of systemic lupus erythematosus, which requires a request for ANA prior to the procedure [24]. We used the association of these agents to decrease NL and JWL. We emphasize that although our choice was for non-cytolytic agents, there are already studies describing the injection of DA in the JWL [17,18].
We obtained excellent results with the different associations of lipolytics mentioned, mainly with DA plus PPC, without any loss of efficacy when the agents were applied with cannulas. The patients had less bruising and edema and considered the application and post-procedure quite tolerable. We have developed a safe technique that considerably reduces patient discomfort during and after the application of lipolytics, with effective results and a low rate of side effects. We have routinely used it as our technique of choice, with greater patient adherence to treatment and better results.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Amaral VDC (2023) Facial and Body Application of Lipolytics through Cannulas: A New Strategy that is Safe, Effective and Better Tolerated by Patients. J Clin Exp Dermatol Res. 14:645.
Received: 29-Aug-2023, Manuscript No. JCEDR-23-25307; Editor assigned: 01-Sep-2023, Pre QC No. JCEDR-23-25307 (PQ); Reviewed: 15-Sep-2023, QC No. JCEDR-23-25307; Revised: 22-Sep-2023, Manuscript No. JCEDR-23-25307 (R); Published: 29-Sep-2023 , DOI: 10.35841/2155-9554.23.14.645
Copyright: © 2023 Amaral VDC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.