Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2021)Volume 10, Issue 2
Background: Measles is one of the world’s most contagious viral diseases that have the potential to be life-threatening. In Ethiopia, measles is among the most common cause for morbidity and mortality in children. Major outbreaks with large attack rates resulting in as high as 15-20% case fatality rates have been reported in this country. There is a paucity of information on measles outbreak response activities and surveillance system performance in Eats Wollega Zone in general and NunuKumba district in particular, Ethiopia.
Methods: A descriptive cross-sectional survey was employed from June 01-05, 2020 at NunuKumba district of East Wollega Zone. The data was collected by three senior technical experts using semi-structured questionnaires, and a secondary data was taken from the line list of cases. Purposive sampling technique was used. Quantitative data was analyzed using Microsoft Excel 2010 while the qualitative data was themed; analyzed and then triangulated with quantitative result. The result was displayed by graphs, tables and Epi-curve.
Results: The overall Attack rate and Case Fatality Rate were 1.05% and 0.41% respectively. The most affected age group was under five year’s children 552(56.55%). The Epicurve indicated the propagation of the outbreak and covered the majority (73%) of Kebeles in the district. The outbreak reached climax at middle of January and declined by the middle of February, 2020.
Conclusion: The AR and CFR of this outbreak were higher than nationally expected target. Age group of 1-4years had higher attack rate. The probable contributing factors for this outbreak were poor health seeking behaviour (poor community awareness and engagement), poor surveillance system, poor PHEM report completeness, lack of operational surveillance guidelines and protocols, and dalliances of lab specimen result written feedback written recommended time period. Therefore, training of human power, and surveillance system should get due attention.
Evaluation, Measles Outbreak, Nunukumba, District, Surveillance Performance, East Wollega Zone
AFR: African Regional Office; AR: Attack Rate; CFRs: Case Fatality Rates; DHO: District Health Office; EHNRI: Ethiopian Health and Nutrition Research Institute; EMDHS: Ethiopia Mini Demographic Health Survey; EPHI: Ethiopian Public Health Institute; EPI: Expanded Program on Immunization; FP: Focal Person; GAM: Global Acute Malnutrition; HCs: Health Centers; HCWs: Health Care Workers; HEWs: Health Extension Workers; HPs: Health Posts; MAM: Moderate Acute Malnutrition; MCV: Measles Containing Vaccine; PHEM: Public Health Emergency Management; PNC: Postnatal Care; RRT: Rapid Response Team; SAM: Severe Acute Malnutrition; SIAs: Supplementary Immunization Activities; WHO: World Health Organization; ZHO: Zonal Health Office
Communicable diseases do not respect national boundaries and are important challenges to health internationally [1]. Measles is one of the world’s most contagious viral diseases that have the potential to be life-threatening and spread by coughing and sneezing, close personal contact or direct contact with infected nasal or throat secretions [2-7]. The most common measles complications includes ear infection, blindness, severe respiratory infections such as pneumonia, severe diarrhoea and related dehydration, brain damage and death [2,3,8]. Even though a safe and cost-effective vaccine is available, in 2018, there were more than 140,000 measles deaths globally, mostly among children under the age of five [8]. In Africa region (AFR), 176,785 confirmed measles cases were reported through case-based surveillance during 2013-2016 [9]. In developing countries, measles case-fatality rates (CFRs) among young children may reach 3-5%, but could be as high as 10% during epidemics [5]. No specific antiviral treatment exists for measles virus. Routine measles vaccination for children combined with mass immunization campaigns in countries with high case and death rates are key public health strategies to reduce global measles deaths. Accelerated immunization activities have had a major impact on reducing measles deaths. Worldwide, during 2000-2018, measles vaccination prevented an estimated 23.2 million deaths [8,9]. In 2011, large measles outbreaks were reported in Ethiopia (3,255 cases) [10]. Surveillance is arguably the most important public health tool used to prevent and control communicable diseases [11]. Surveillance of communicable diseases like measles helps to monitor the trends of diseases and to take the appropriate action in timely manner [12,13]. Public health or Epidemiologic surveillance, often called the cornerstone of public health practice, is the continuous, systematic collection, analysis, description, and interpretation of health-events needed for the planning, implementation, monitoring, and evaluation of public health practices or interventions or programs [14-17]. With rapidly changing ecology, urbanization, climate change, increased travel and fragile public health systems, epidemics or outbreaks will become more frequent, more complex and harder to prevent and contain [18]. Measles outbreaks occur when the accumulated number of susceptible individuals is greater than the critical number of susceptible individuals for a given population to sustain transmission [19]. In 2010, 28 countries in the African Region experienced measles outbreaks [20]. Many countries around the world are experiencing measles outbreaks. As of 5 November 2019, there have been 440,263 confirmed cases reported to World Health Organization (WHO) through official monthly reporting by 187 Member States in 2019. Large measles outbreaks are being reported in several countries in the African region. It is indicated that any community with less than 95% population immunity is at risk for an outbreak of measles [21]. The suspected measles outbreak is the occurrence of five or more reported suspected measles cases in one month in a defined geographic area such as a Kebele, Woreda or health facility catchment area; while the confirmed measles outbreak: occurrence of three or more laboratory confirmed measles cases in one month in a defined geographic area such as a Kebele, Woreda or health facility catchment area [20]. In Ethiopia, measles is among the most common cause for morbidity and mortality in children. Major outbreaks with large attack rates resulting in as high as 15-20% case fatality rates have been reported in this country. Measles related case fatality rates range between 3-5% in non-epidemic circumstances [22]. A study done in Artuma Fursi Woreda of Amhara region, Ethiopia showed that an attack rate (AR) and case fatality rate (CFR) of 11.8/100,000 and 2.6%, respectively [23]. Another similar study conducted in Simada district of Amhara region, Ethiopia showed that a CFR of 13.4%. It revealed that the measles outbreak occurred in remote kebeles (about 7 hour on foot from the main road) in which scheduled immunization delivery was challenging [24]. The information gained from measles surveillance is used to develop measles prevention strategies and to evaluate the impact of these strategies [6]. A literature review suggested that no evaluation of the measles outbreak response activities and surveillance system performance has been conducted in East Wollega Zone. Thus, to fill the existing gaps of an of measles outbreak response activities and surveillance system performance in Nunukumba district of east Wollega zone was conducted with objective to identify strengthens, weakness, understand shortcomings in systems and proposed recommendation.
Effective communicable disease control relies on effective disease surveillance. A functional national communicable diseases surveillance system is essential for action on priority communicable diseases. It is a key part of public health decision-making in all countries (e.g. priority setting, planning, resource mobilization and allocation, prediction and early detection of epidemics, and monitoring and evaluation of disease prevention and control programmes). The core functions in surveillance of any health event are case detection, reporting, investigation and confirmation, analysis and interpretation, action, control or response, policy and feedback. These functions are made possible by support functions that improve core surveillance functions setting of standards (for example case definitions), training and supervision, setting up laboratory support, setting up communications and resource management [25]. The most critical step to prevent and control epidemics effectively is the timely detection of outbreaks, which depends on effective disease surveillance systems [26]. In developed countries the CFR for measles tends to be low, between 0.1 and 1.0 per 1000 cases, while in developing countries the overall CFR has been estimated to be between 3% and 6%. The highest CFR occurs in infants under 12 months of age, among whom it reaches between 20% and 30% [6]. Measles is still common in many developing countries particularly in parts of Africa and Asia. The overwhelming majority (more than 95%) of measles deaths occur in countries with low per capita incomes and weak health infrastructures. According to the latest WHO data published in 2017 the number of measles death in Ethiopia is 25,103(3.95%), death rate (deaths per 100,000 population) is 15.44, that’s about 1 of every 25 deaths in Ethiopia. About 69 people die of measles each day, an average of 1 death every 21 minutes [7]. The study conducted to assess the economic burden of concurrent measles and rubella outbreaks in Romania from 2011-2012 revealed that cost per case was US $439 for measles. Up to 36% of households needed to borrow money to pay for illness treatment. Households incurred a high economic burden compared with their incomes, and the health sector bore most costs [27]. A similar study conducted in Keffa Zone of Ethiopia revealed that the economic cost of the measles outbreak and response was 758,869 United States dollars (US$). Household economic cost was US$29.18/case, equal to 6% of the household median annual income. Hence, Improvement in two-dose measles vaccination coverage above 95% would both reduce measles incidence and save considerable outbreak-associated costs to both the health sector and the households [28]. In East Wollega Zone there is lack of empirical evidences on evaluation of measles outbreak response activities and surveillance system performance. Hence, the aim of this survey is to evaluate of measles outbreak response activities and surveillance system performance in NunuKumba district, East Wollega Zone of Oromia Region, Ethiopia, June 2020.
Study area and period
The survey was conducted in NunuKumba district. This district is one of the seventeen districts of East Wollega Zone, Oromia regional State which is found at a distance of 68 Kilometer (km) from Nekemte town, the Zonal capital and 400 km west of the national capital, Addis Ababa. Based on the national population census of 2007; the total population of NunuKumba district in the year 2019/2020 is projected to be 92,514. The estimated number of surviving infant, less than two years and under five years’ children for the year 2019/2020 is 2,979, 5,283 and 15,200 respectively. The public health infrastructure of the district comprises of four functional healthcenters and 21 rural health posts. All health centers and health posts are expected to provide routine EPI services and conduct disease surveillance. These public health facilities in the district are staffed with 73 technical staffs with different professions’; 55 health extension workers; and 52 administrative staffs adding up to 180 total health work force in the district. The district is administratively structured into 21 rural and one urban Kebele (the smallest administrative unit in Ethiopia). NunuKumba district is bounded by WamaHagalo district and Jima Zone by the East, JimaArjo district by the west, LekaDulecha district by the North and BunoBedele Zone by the South [29]. This survey was conducted from June 01-05,2020.
Study design
A cross-sectional descriptive study was employed.
Population
Source population: All public health care workers in the district from June 01-05, 2020.
Study population: Purposely sampled public health care workers; all individuals affected by the measles and filled on the line list during the study period.
Study unit
An individual was taken as the study unit
Eligibility criteria
Inclusion criteria: Health managers of the district health office and health centers, PHEM and EPI focal persons of the district and health centers, disease prevention and control (DPC) case team coordinator of the district health office, and health extension workers were included in the survey.
Exclusion criteria: Health care workers who are on annual and maternity leave and those participants who were not interested to respond were excluded from the survey.
Sample size and Sampling procedures
Sample size determination: District health office, four (all) healthcenters in the district and 7 out of 22 Kebeles in the district which accounts 30 % of the total Kebeles were included in this survey. With regard to participants included in the survey; five participants were purposively included from district health office and each health center. From seven purposely sampled kebeles fifteen (15) health extension workers (HEWs) were included in the survey. Besides, four focus group discussions (1 female and 1 male group) each comprising of 8 members was included in the survey to capture the qualitative data. Finally, a secondary data from line list of 976 measles affected individuals was taken and analyzed after conducting a record review. The total sample size of this assessment was 1,006(30 participants, and a line list secondary data of 976 measles affected individuals) were included in the assessment
Sampling procedures: The required sample was taken from district health office, health centers, and health posts in the district by using purposive sampling techniques and a secondary line list data of 976 measles affected individuals were included in the survey.
Data collection procedures
Data collection tool: The primary data was collected by using semistructured questionnaire which was developed for the purpose of data collection after reviewing previous related and relevant literatures consulting senior thematic experts from East Wollega Zonal Health Office and partners working on this thematic area in the zone [1-46]. Besides, key informant’s in-depth interview, focus group discussion, observation checklist and the record review of secondary data of the surveillance and EPI report from July1, 2018 to February 30, 2020(which is 1 year and 8 months data) was used to attain the objective of the survey.
Data collection procedures: The data was collected by three senior technical experts (two from East Wollega Zonal Health Office and one from USAID Transform: Primary Health Care Project), under the supervision of East Wollega Zonal Health Office Public Health Emergency Management (PHEM) case team. We used face-to-face key informants interview from Woreda Health office Head, PHEM and EPI focal persons), from Health centres (Directors, PHEM and EPI focal persons) and from health posts (health extension workers) by using interview guide and semi-structured questionnaire. Two focus group discussions (purposely sampled HEWs and health care workers). Besides, the record review of the secondary data of surveillance and EPI reports from July1, 2018 to February 30, 2020(which is 1 year and 8 months data) was reviewed and analysed by using MS Excel 2010. Finally, we used observation checklist to verify health facilities previous and current status regarding PHEM preparedness and response activities.
Study variables
Dependent variable
• Measles surveillance system performance
Independent variables
• General information and socio-demographic characteristics of measles affected individuals dis-aggregated by age, sex, date of onset, date of visit to health facilities, treatment outcome, vaccination status, nutritional status, signs and symptoms, residence, and travel history.
• Public health emergency management (PHEM) related activities [availability of Emergency response preparedness plan, training status of PHEM focal person, availability of updated PHEM guidelines and protocols, availability and functionality of rapid response team (RRT), PHEM report status, supportive supervision, outbreak information and response.
Operational definitions
• Suspected measles outbreaks: taken as the occurrence of five suspected measles cases in one month in a defined geographic area such as Kebele, District or Health facility catchment.
• Confirmed measles outbreaks: taken as presences of 3 or more laboratory confirmed measles cases in a one month time per Kebele or District or Health facility.
• Suspected measles case: any person with generalized maculopapular rash and fever plus one of the following:-a cough or coryza (a runny nose) or conjunctivitis (red eyes).
• Laboratory confirmed cases: A suspected case, which has laboratory results, indicating infection (IgM positive or isolated for a measles virus).
Data processing and analysis procedures
The quantitative data obtained were entered and analysed using Microsoft Excel 2010 and epidemiological-curve (Epi-curve). Before the final analysis we performed data cleaning by looking at the distribution of the data and its completeness, identifying outliers and checking back against the original data and analysis of descriptive statistics was carried out. The qualitative data was themed; analysed and triangulated with quantitative result. From line list of 976 measles affected individuals descriptive statistics like attack rate and case fatality rate were calculated and results were presented using graphs, tables and Epi-curve.
Data quality control
After developing the standard data collection tools by senior thematic experts from East Wollega Zonal Health Office and partners working on this thematic area; two days detail discussion was conducted on the comprehensiveness; clarity and applicability of the tools for the participants and thereby to attain the objective of the assessment at respective study set up and then some modifications was made to the tools accordingly. Brief orientation was also provided to the data collectors by East Wollega Zonal Health Office PHEM case team on the interview procedure for one day. Besides, data collectors were instructed to check the completeness of each questionnaire at the end of each interview to maintain the data quality daily.
Ethical consideration
Before data collection; letter of approval to conduct the survey was obtained from East Wollega Zonal Health Office, Oromia Regional State, Western Ethiopia. Besides, each participant involved in the survey was informed about the purpose of the survey; the right to refuse to participate in the survey; and confidentiality of the information was kept. They assured that they will not be penalized for not participating if they wishes not to participate; and their responses to the questions had no effect on their care. Finally, verbal consent was obtained from each participant.
Dissemination and utilization of the assessment result
First, the final result was presented to NunuKumba district Health Office staffs; catchment primary healthcare unit staffs and other concerned bodies in the district. After approvals of the survey result by the district health office and reached on the final consensus; copy of the finding was submitted to NunuKumba district health office. Then, the result of the survey was presented to East Wollega Zonal Health Office staffs; laterally operating partners on the thematic area and others stakeholders. After final approval was made by East Wollega Zonal health office senior management team; PHEM and Family health case team; Zonal senior technical experts and concerned partners in the zone; and the copies of the survey finding was submitted to East Wollega Zonal Health Office, Oromia Regional Health Bureau(ORHB), concerned partners and stakeholders that have direct and in-direct contribution to improve the healthcare delivery services in general; surveillance and EPI program in particular at primary health care unit level. Moreover the result of the finding was presented in different workshops, seminars, and health symposium. Finally it will be published in reputable international scientific journal.
Outbreak profile and characteristics
The total of 976 suspected measles cases from 30/09/2019 to 02/04/2020, with one community and three facility deaths reported from NunuKumba district of East Wollega Zone, Western Ethiopia. From these 976 cases; 8 cases were from adjacent LimuSeka district of Jimma Zone, Western Ethiopia. Therefore a total of 968 cases reported from NunuKumba district, and the overall Attack rate (AR) and Case Fatality Rate (CFR) were 1.05% and 0.41% respectively.
Of the 976 suspected cases reported on the line list; four specimens collected and sent to Ethiopian Public Health Institute (EPHI) and tested IgM positive; while the others 972 were confirmed by epidemiologically linked and clinically compatible cases fulfilling suspected the measles case. The major signs and symptoms reported by all of suspected 972(100%) and deceased cases (4) were fever, rash, cough, conjunctivitis (red eyes), and coryza (runny nose). Three (3) facility and one (1) community deaths were reported giving a case fatality rate (CFR) of 0.3% and 0.10% respectively with the total AR and CFR of 1.05% and 0.41% respectively. The ratio of AR for males and females was almost one to one.
Three of the four deceased cases were females, and one was male. Among these three of them were unvaccinated. Three of deceased cases belong to Adare and one was from Birinkas primary health units (PHCUs). The median age was 5.9years (range, 1 month to 38 years) and 46.7% of cases were 1 to 4 years. Patients with under fifteen years (<15years) of age accounted for 90.1% of all the studied measles cases. The sex disaggregated distribution of cases based on the line list was:- male (492, 50.40%) and female (484, 49.60%) (Table 1).
| Variables | Number of cases(N=976) | Percentage (%) |
|---|---|---|
| Age Group | ||
| < 9 months | 71 | 7.3 |
| 9 to 11 month | 31 | 3.2 |
| 1 to 4 years | 456 | 46.7 |
| 5 to 14 years | 321 | 32.9 |
| >15years | 97 | 9.9 |
| Total | 976 | 100 |
| Sex | ||
| Male | 492 | 50.4 |
| Female | 484 | 49.6 |
| Total | 976 | 100 |
Table 1: Distribution by age and sex of 976 measles cases investigated in NunuKumba District, East Wollega Zone, Oromia Regional State, Western Ethiopia, June 2020.
From the total of twenty two kebeles in the district; sixteen (73%) of them were reported the cases with varying magnitudes. For example; Wama Adare, Wama Gudattu, Jano Gure and Hawi Bekumsa was among Kebeles reported the majority of the measles which accounts (666, 68.4%) of total cases (Figure 1).
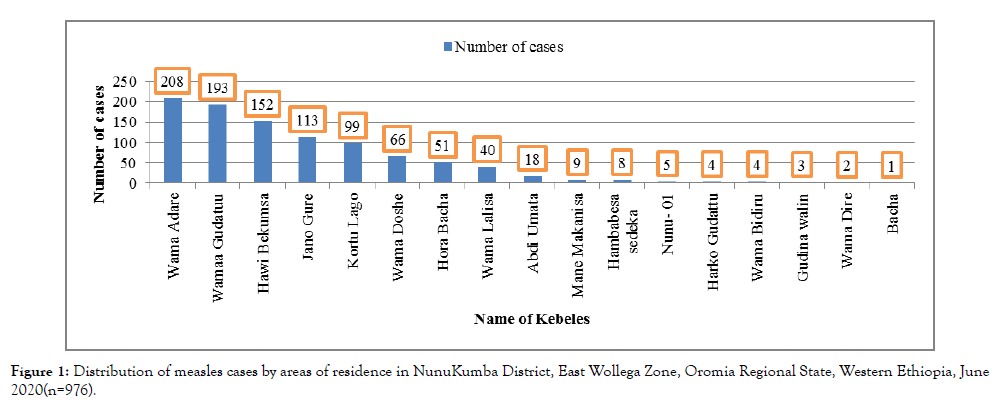
Figure 1. Distribution of measles cases by areas of residence in NunuKumba District, East Wollega Zone, Oromia Regional State, Western Ethiopia, June 2020(n=976).
High attack rate (AR) was reported from WamaGudattu, HawwiBekumsa, WamaAdare and KortuLago Kebeles (Table 2).
| S.no | Name of Kebeles | Total Population | Total cases reported | AR /100 |
|---|---|---|---|---|
| 1 | Nunu-01 | 4,585 | 5 | 0.1 |
| 2 | Bachu | 1,402 | 1 | 0.1 |
| 3 | HarkoGudatu | 4,898 | 4 | 0.1 |
| 4 | GudinaWalini | 2,040 | 3 | 0.1 |
| 5 | WamaDire | 1,977 | 2 | 0.1 |
| 6 | WamaAdare | 5,209 | 208 | 4 |
| 7 | KortuLago | 2,503 | 99 | 4 |
| 8 | WamaDoshe | 2,780 | 66 | 2.4 |
| 9 | WamaLalisa | 3,680 | 40 | 1.1 |
| 10 | WamaBidiru | 3,121 | 4 | 0.1 |
| 11 | AbdiUmata | 2,752 | 18 | 0.7 |
| 12 | WamaGudatu | 2,770 | 193 | 7 |
| 13 | JanoGure | 2,606 | 113 | 4.3 |
| 14 | HawiBekumsa | 3,005 | 152 | 5.1 |
| 15 | ManeMakanisa | 2,179 | 9 | 0.4 |
| 16 | HoraBacha | 4,547 | 51 | 1.1 |
| Total | 50,053 | 968 | 1.9 | |
| Note: The total population in Table 2 is not the total district population by Kebeles but age specific population from each Kebeles of the district. |
||||
Table 2: The distribution of cases by its Attack rate in Kebeles of NunuKumba district, East Wollega Zone, Oromia Regional state, Western Ethiopia, June 2020(n=968).
The attack rate (AR) of the measles outbreak was higher among age group ranging from 1-4years old 3.7 %( 452/12,194) followed by <1years 3.3 %( 100/3,006, 3.3%) and also higher among male than female with 50.41% and 49.59% respectively. High CFR was reported from those 1-4years and >15years. Besides, CFR was higher among female than male with 0.60% and 0.20% respectively (Table 3).
| Variable | Population at risk | Number of cases | Number deaths | AR/100 | CFR/100 |
|---|---|---|---|---|---|
| Age group | |||||
| < 1year | 3,006 | 100 | 0 | 3.3 | - |
| 1 to 4 Year | 12,194 | 452 | 3 | 3.7 | 0.7 |
| 5 to 14 year | 20,573 | 320 | 0 | - | - |
| >15 Years | 14,280 | 96 | 1 | 0.7 | 1.04 |
| Total | 50,053 | 968 | 4 | 1.9 | 0.41 |
| Sex | |||||
| Male | 45,033 | 492 | 1 | 1.09 | 0.2 |
| Female | 47,481 | 484 | 3 | 1.02 | 0.6 |
| Total | 92,514 | 968 | 4 | 1.05 | 0.41 |
| Note: Total population used in Table 3 for sex disaggregated is the projected population of the district in the year 2019/2020. |
|||||
Table 3: Distribution of measles cases by its Attack rate, Case fatality rate and Sex disaggregated at NunuKumba district of East Wollega Zone, Oromia Regional state, Western Ethiopia, June 2020(n=968).
With regard to the distribution of cases by admission status; the majority 712(73%) of the cases managed at outpatient department (OPD) and the remaining (27%) was managed at inpatient department (IPD).
From the line list result; we have seen that the day difference between the date they saw sign and symptom of the diseases and the date they visited health facilities took 0 to 16 days. The majority of them seek health care services within the 3rd and 4th days. The mean date difference was 3.1 days (Figure 2).
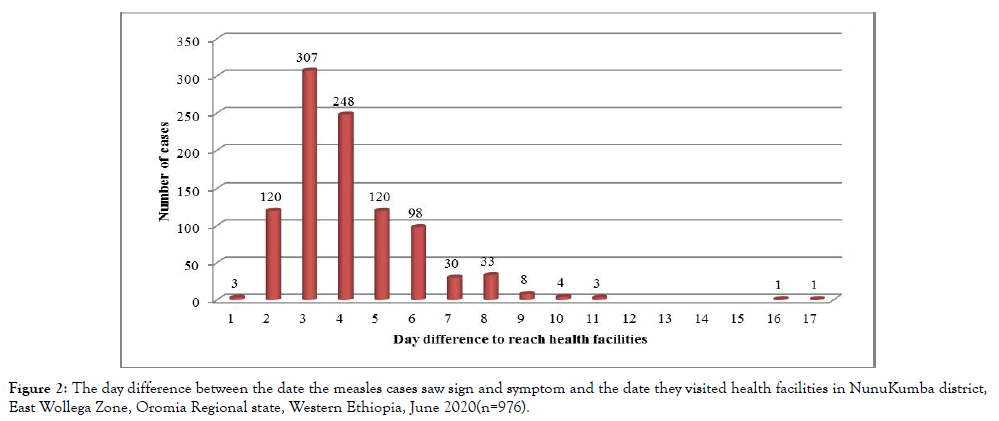
Figure 2. The day difference between the date the measles cases saw sign and symptom and the date they visited health facilities in NunuKumba district, East Wollega Zone, Oromia Regional state, Western Ethiopia, June 2020(n=976).
Distribution of cases by time
The outbreak reached climax at middle of January and declining by the middle of February. Measles vaccination campaign was initiated after the declining of an outbreak. Had the intervention occurred earlier, it is clear that its impact would have been greater. Even though it occurred late in the outbreak, the intervention might have contributed to improving population immunity, shortening the duration of the outbreak and preventing some severe cases and probable deaths (Figure 3).
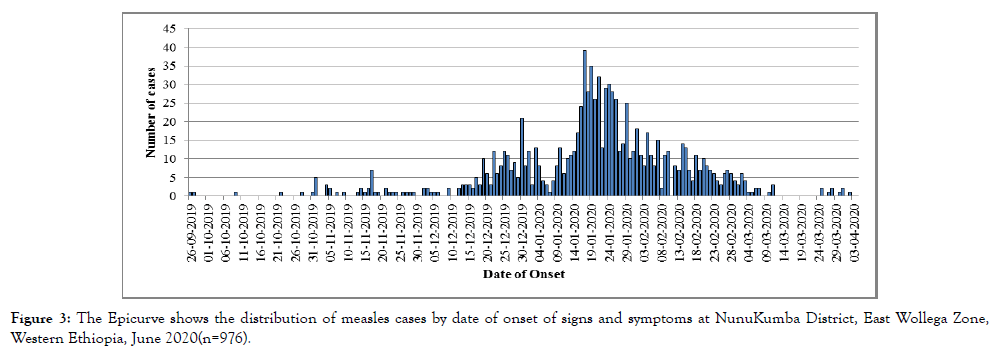
Figure 3. The Epicurve shows the distribution of measles cases by date of onset of signs and symptoms at NunuKumba District, East Wollega Zone, Western Ethiopia, June 2020(n=976).
The Epi week shows us that due to lack of immediate response; the outbreak covered majority of district kebeles. In Epi week 4 the outbreak reached climax and down over the past four weeks. Deaths were reported in week 50 of 2019, week 2 and week 3 of 2020 (Figure 4).
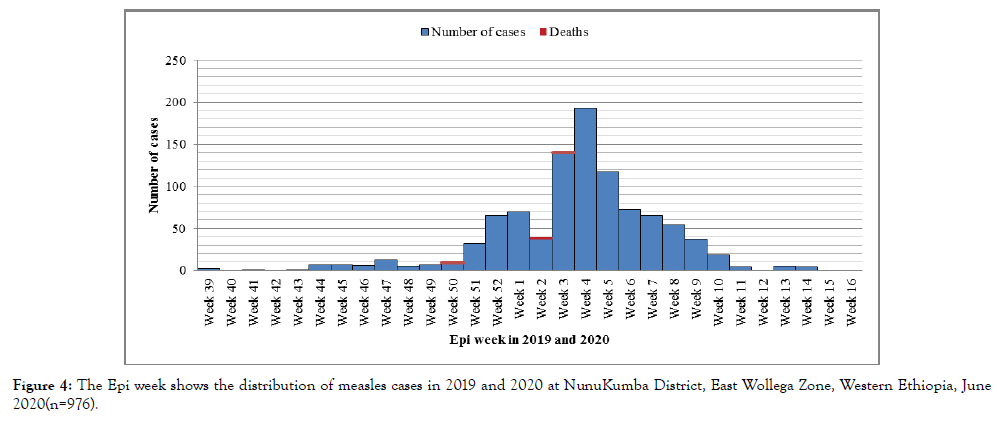
Figure 4. The Epi week shows the distribution of measles cases in 2019 and 2020 at NunuKumba District, East Wollega Zone, Western Ethiopia, June 2020(n=976).
Measles outbreak response
East Wollega Zonal Health (ZHO) responded to an outbreak in different ways. These were- deployed physicians and pediatricians from Nekemte specialized and Arjo Primary Hospitals and managed the cases; mobilized supplies for cases management and conducted capacity building for health workers and health extension workers. Social mobilization was conducted at school, Churches and Mosques after preparing key messages on measles prevention and control measures. Besides; ZHO strengthened surveillance: activated Zonal epidemic preparedness and response plan and team; Zonal PHEM assigned surveillance officer to support the district, alert letter disseminated for all districts in the Zone, active case searches and weekly incidence monitoring were conducted in the district. With regard to logistic and resources mobilization; the ZHO mobilized supplies from adjacent districts and partners for the support. Moreover, following the current outbreak, measles vaccination campaign and jointly nutritional mass screening campaign has been conducted for whole districts in the Zone. The age groups targeted during the campaign for both vaccination and nutritional mass screening was those under five years children, accordingly a total of 13,639 children were targeted. The overall measles vaccination and nutritional mass screening campaign coverage for the under-five was 102.3% and 102% respectively. The district has 21 kebeles and 4 PHCUs. The campaigns were divided into four clusters according to the number of PHCUs. The coverage is various among the PHCUs and all of them have achieved above expected recommended coverage of 95%. High performance was reported from Brinkas PHCUs; while the least was from Nunu PHCUs (Table 4 and Table 5).
| Name of primary health care units(PHCUs) |
Total Population |
Number of Kebeles |
Target 6-59 months |
Total Vaccinated |
Coverage (%) |
|---|---|---|---|---|---|
| Nunu PHCUs | 35,176 | 9 | 5,276 | 5,269 | 99.9 |
| Adare PHCUs | 33,066 | 7 | 4,960 | 5,033 | 101.5 |
| Birinkas PHCUs | 8,071 | 2 | 1,211 | 1,445 | 119.3 |
| Dalati PHCUs | 14,610 | 3 | 2,192 | 2,210 | 100.8 |
| Total | 90,923 | 21 | 13,639 | 13,957 | 102.3 |
Table 4: The distribution of measles vaccination campaign done during the outbreak at primary health care units of NunuKumba District, East Wollega Zone, Western Ethiopia, June 2020 (n=13,957).
| S.no | Name of PHCUs | Screening 6-59 months | Screening pregnant and lactating women(PLW) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Plan | Achievement | % | MAM | SAM | Plan | Achievement | % | MAM | SAM | ||
| 1 | Nunu PHCUs | 5276 | 5269 | 99.9 | 172 | 64 | 7758 | 7493 | 97 | 145 | 6 |
| 2 | Adare PHCUs | 4960 | 5033 | 101 | 150 | 49 | 6864 | 6441 | 94 | 97 | 8 |
| 3 | Birinkas PHCUs | 1211 | 1445 | 117 | 104 | 23 | 1650 | 1575 | 95 | 27 | 0 |
| 4 | Dalati PHCUs | 2,192 | 2210 | 101 | 98 | 56 | 2,982 | 2798 | 94 | 111 | 15 |
| Total | 13638 | 13957 | 102 | 524 | 192 | 19254 | 18307 | 95 | 380 | 29 | |
| Note: The Global acute malnutrition (GAM) is the summation of moderate and severe acute malnutrition (GAM=MAM+SAM). |
|||||||||||
Table 5: The distribution of nutritional screening results at NunuKumba district, East Wollega, Western Ethiopia, June 2020(n=2192+2982=5174).
The nutritional mass screening conducted during the outbreak response showed that among the children 6-59 months screened for malnutrition about 3.8% and 1.4% of them had moderate and severe acute malnutrition respectively with a global acute malnutrition (GAM) of 5.1% (Table 5).
Post outbreak assessment finding
Public Health Emergency Management (PHEM) activities: The main activities undertaken on PHEM events were thoroughly assessed. At the district there is epidemic preparedness plan of the year 2019/2020. However, there was no separated and written epidemic preparedness plan at health centers level; forexample in Birinkas and Dalati catchment areas.
There is no regional or national PHEM written guidelines. The PHEM focal person of Dalati health center did not take basic training on PHEM. We also found that there was a standard case definition of common epidemic prone diseases like measles, neonatal tetanus, and acute flaccid paralysis posted on the wall at different health care service units in the district and at primary health care units.
The district PHEM experts were not providing technical support to the health centers service providers for the last one year. Likewise, the health centers PHEM experts were not supporting their catchment health posts by using the standard checklist. There was no written feedback from DHO to health centers; and health centers to catchment health posts on PHEM activities.
In the year 2018/2019 and the first eight months of 2019/2020 the PHEM report completeness of health centers was 81% and 91% respectively. Likewise health posts level PHEM report completeness during the same period was 70% and 93% respectively. Besides, we found that at both district and primary health care units’ levels there is no PHEM report timelines tracking system at all.
Outbreak related activities
In the district the two suspected measles cases were reported from Bacu and HarkoGudetu Kebeles of Nunu PHCU on 30/09/2019 and date of illness onset were 28/09/2019. The samples were collected from these suspected cases and sent to Ethiopian public health institute (EPHI). The lab result feedback was not received and the cases were treated by antibiotics and vitamin A and they get relieved. There was no search done for contact history and the probable epidemiologically linked cases.
The first index case for the current outbreak was reported from HoraBaca Kebele of Dalati PHCUs. This case was a vaccinated 2.6years old female. The date of illness onset was 28/10/2019 and the date examined at Dalati health center was 30/10/2019. This case was reported to DHO within 24 hours and treated by antibiotic and Vitamin A and get relieved. However, the district delayed for about two weeks and they started to respond after the cases surge and spread to Adare PHCUs and reported to the district. HoraBaca Kebele is bounded by Meta and Gerjeja Kebeles of JimmaArjo district of East Wollega Zone in which the communities are socially interlinked and where there was a previous reported suspected measles cases. Under Dalati PHCUs; the highly affected Kebele was HawiBekumsa and which is 10KM away from the health center. Then the suspected cases were increased at Adare PHCUs; especially at WamaAdare and WamaDoshe Kebeles starting from 13/11/2019. About ten suspected cases from Adare health center were referred to Arjo primary hospital on 19/12/2019. After the suspected cases referred to the hospital and measles suspected cases happened at different sites; the district health office collected the samples of four measles suspected cases and sent it to EPHI on 24/12/2019. All of the samples were collected from suspected cases at WamaDoshe Kebele of Adare PHCUs. The lab result written feedback was not given to the DHO and they were informed by telephone call notices from ZHO PHEM focal person that all of the samples were found to be IgM positive. Then the DHO rapid response team (RRT) come together and declared the occurrence of the measles outbreak on 19/12/2019.
The difference between date of illness onset and health care facilities visit was 8 days, 9 days, and 10 days with an average of 9 days (Table 6).
| Codes of index cases |
Sex | Age (in years) |
Address | Vaccination status |
Date of onset of disease |
Date seen at health facility |
Date health facility notified the district |
Date sent to lab |
IgM result |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 4 | Wama Doshe | Vaccinated | 13-12-2019 | 22-12-2019 | 22-12-2019 | 24-12-2019 | Positive |
| 2 | M | 4 | Wama Doshe | Vaccinated | 12-12-2019 | 22-12-2019 | 22-12-2019 | 24-12-2019 | Positive |
| 3 | M | 4 | Wama Doshe | Vaccinated | 13-12-2019 | 22-12-2019 | 22-12-2019 | 24-12-2019 | Positive |
| 4 | F | 6 | Wama Doshe | Vaccinated | 14-12-2019 | 22-12-2019 | 22-12-2019 | 24-12-2019 | Positive |
Table 6: The characteristics of index cases in NunuKumba district, East Wollega Zone, Western Ethiopia, June 2020.
According the data reported on the line list the first measles suspected case was reported from Nunu-01 Kebele and visited the health facilities on 30/09/2019. In the district the last measles suspected case was reported from AbdiUmata Kebele of Adare PHCUs on 02/04/2020. The total duration of the outbreak after being declared by the district RRT lasted for three solid months and thirteen days (19/12/2019 to 02/04/2020). Despite of having the line list data of cases; it was not analysed by place, person and time at both the district and PHCUs levels.
All outbreaks cannot be predicted or prevented. However, precautionary measures can be taken within the existing health infrastructure and service delivery to reduce risks of outbreaks and to minimize the scale of the outbreak, if it occurs [30]. Evaluation is an important tool for policy makers that help to improve the performance and productivity of health programs. The rationale of evaluating public health surveillance systems is to determine if the disease is being monitored efficiently and effectively [31]. In this outbreak survey the overall attack rate (AR) was 1.05%. This is higher than the study conducted in Kabridahar District, Ethiopia which revealed the overall AR of 0.4/1000 [32]. The possible explanation for these differences was early diagnosis and management of cases at Kabridahar district. The overall CFR of this outbreak was 0.41%. This is lower than the study conducted in both Artuma Fursi Woreda and Simada district of Amhara region, Ethiopia, Indonesia and Mozambique which revealed the CFR of 2.6%, 13.4%, 14.1% and 4.4% respectively [23-24,33-34]. Another study conducted in west Hararghie zone, Ethiopia, and Sudan revealed the measles CFR of 6.7 % and 0.9% respectively; which was higher than the current finding [35,36]. A similar, the study conducted in Kabridahar District, Ethiopia showed that the overall measles CFR of 0% which is lower than the current result [32]. These all differences might be due to immunization status and coverage differences, socio-cultural influences, early detection and response, malnutrition and overcrowding.
The median age of the cases in this survey was 5.9 years. This is lower than the study conducted in Artuma Fursi Woreda of Amhara region which showed the median age of the cases as 7.5 years [21]. This finding is higher than the study conducted in the metropolitan setting, Addis Ababa, Ethiopia and Brazil which revealed that the median age of the cases w 5 years and 11 years [37, 38]. This study also revealed the age of affected cases ranges from 1month to 38 years. This study is similar with the study conducted in Brazil [38] and higher than the study conducted at different area [33]. This outbreak assessment indicated that the majority of the cases were the age group ranging from 1 to 4 years (456,46.7%). This is consistent with the study conducted in Indonesia in which the highest AR (50.0%) occurred among 1-4 years age group [33,39]. A similar study conducted in Brazil indicated that 27.6% of measles cases occurred under 9 months of age and higher AR was between 9-23 months [34]. This finding indicated that the sex disaggregated distribution of AR was: male (492,50.40%) and female (484,49.60%). This means the ratio of male to female was almost one to one. This is almost consistent with the study conducted in Sudan which showed that 51% male and 49% female were affected by measles outbreak [36]. This assessment showed that the CFR was slightly higher among female (0.6%) than male (0.2%). The current result is also consistent with the study conducted in Simada district of Amhara region, Ethiopia which revealed that a majority of deaths occurred among females (9/13, 69.2%) [27]. In contrast to this finding the study conducted in Indonesia revealed that about 64.3% of measles cases were male [33]. The possible explanation for this finding was the female were more affected by malnutrition and there might be gender related socio-cultural influence.
It is revealed that more than one fourth of the cases (27%) were admitted. This result is lower than the study conducted in China which showed that about 61% of cases had been hospitalized [40]. This assessment showed that the mean date difference of cases to seek health care services was 3.1 days and the majority of them seek health care services within 3rd and 4th days. This result is consistent with the study conducted in in Zaka, Zimbabwe which revealed that the median duration for seeking treatment after onset of illness was 3 days [41]. This assessment revealed that there is epidemic preparedness plan of the year 2019/2020 at the district level; while there was no separated and written epidemic preparedness plan at health centres levels. This is similar with the study conducted in Zaka, Zimbabwe [41]. This is consistent with study conducted in Afar, Ethiopia which revealed that the performance of surveillance systems core activities like epidemic preparedness and response at district and health facility level were far from the 80% target [31]. The current finding showed that the PHEM focal persons at the district and health centers levels did not analyzed data and used it for decision making. This is similar with the study conducted in Zaka, Zimbabwe, Dawuro Zone and Afar, Ethiopia [31,41,42]. The possible explanation was lack of knowledge and skills to conduct outbreak report analysis. Besides, it showed poor surveillance system at district and primary health care unit levels.
This assessment revealed that the DHO delayed for about two weeks to respond and conducted the field investigations after the first index cases were reported from the health care facilities. This is similar with the study conducted in Zika, Zimbabwe [41]. Another similar study conducted in Mozambique revealed that about 73.2% of respondents said there was no adequate coordination and communication local, state and national levels [43]. The study conducted in Amhara region, Ethiopia showed that about threefourth (76%) of surveillance focal persons had a refresher training in the last two years [44]. In contrast to this; the current finding revealed that all surveillance focal persons (100%) were trained. This finding is also in contrast to the study conducted in Afar, Ethiopia in which training status at health facility levels was far from the 80% target [31]. World Health Organization (WHO) recommended all epidemic prone diseases like measles cases are to be reported on weekly basis including zero reporting [33]. It also stated that at least 80% of reporting completeness is considered as satisfactory [42]. In this assessment it was revealed that the reporting completeness of PHEM report at the health centre in the year 2018/2019 and the first eight months of 2019/2020 was 81% and 91% respectively. Likewise health posts level PHEM report completeness during the same period was 70% and 93% respectively. The current finding was higher than that of WHO regional office for Africa which was around 57%, and lowers than the completeness of data in Western African sub region which was 94% [42]. In this finding; the reporting completeness of health posts in the year 2018/2019 was lower than WHO recommended set of performance indicators or targets which was % of weekly report received should be ≥ 80% and the study conducted in Yemen [46,47]. World health organization recommended that the suspected measles cases should be investigated with house visits and notified to concerned bodies within ≤ 48 hours [46]. In contrast to this; there was no field investigation conducted to address contact tracing and link identified cases epidemiologically in the current measles outbreak. This assessment also found that; there was no written feedback from DHO to health centers; and health centers to catchment health posts on PHEM activities. This is similar with the study conducted in Dawuro Zone and Afar, Ethiopia [31,42]. A similar study conducted in Mozambique revealed that about 63.3% of respondents responded that they did not get prompt feedback when diseases were reported from national or state ministries. Besides, it showed that 49.7% of respondents responded that lack of feedback prevent the practice of disease reporting [43]. Qualitative result also supports this finding.
The PHEM focal person at Birinkas health centre said that “monitoring and evaluation of EPI program is weak from DHO and ZHO” (Male participants 25years during in-depth interview, Birinkas HC). This is supported by the study done in Mozambique in which about 47.2% of respondents responded that poor staff motivation and weak supervision (46.5%) prevents the practice of disease reporting [43]. WHO recommendation on data analysis, presentation and reports set performance indicators or targets as: % of weekly report received ≥ 80%, % of cases notified ≤ 48 hours after rash onset (all cases that meet the clinical case definition), % of cases investigated with house visits ≤ 48 hours after notification ≥ 80%, % of cases with adequate specimen and laboratory results within 7 days ≥ 80%, and % of confirmed cases with source of infection identified ≥ 80% [46]. In contrast to this; the current finding indicated that an average day between the date of illness onset and health care facility visit was nine days which was higher than the study conducted in Zaka, Zimbabwe that showed the median duration for seeking treatment after onset of illness was 3 days [41]. The possible explanations were the differences in community awareness, health seeking behaviours, socio-cultural influences, early diagnosis and response.
The current finding indicated that the epidemic curve was sustained propagating in the community with no apparent periodicity and covered majority of the district Kebeles. This is similar with the study conducted in Kamwenge District, Western Uganda [48]. The study conducted in Amhara regional state of Ethiopia showed that the seasonal peak of measles cases noted in the hot-dry season of the year [49]. In consistent with this the outbreak in the current assessment reached climax at middle of January 2020 and declined by the middle of February 2020.
This finding revealed that; there was no PHEM related written guidelines at both the district and health centers level. In contrast to this; the study conducted in Amhara region, Ethiopia showed that 87% of visited health facilities had operational surveillance guidelines and 84% of them had national PHEM guidelines [44]. Another similar study conducted in Afar, Ethiopia revealed that the performance of surveillance system supportive functions like presence of PHEM guidelines at health facility levels were far from the 80% target [32]. The possible explanation for these differences might be high turnover of trained human power and preference of softcopy than hard copy.
In the current assessment we found that the standard case definitions on AFP, measles and NNT were available and posted in different units at both district and all health centers. This is consistent with the study conducted in Afar, Ethiopia [31]. This finding was higher than the finding from the study conducted in Amhara regional state of Ethiopia which revealed that 93% of visited health facilities had these standard case definitions [44].
Post-outbreak crisis
• Malnutrition and diarrhoea surge due to diversion of attention to the outbreak mitigation and response.
• Financial crisis because the entire district budget was shifted to the outbreak mitigation and response.
• Households and individuals were economically affected as a result of cases treatment and referral.
• Drugs used during the outbreak was not yet replaced at the health centers; especially Pediatrics drugs at <5year OPD
• Medical equipment and rooms were occupied by the cases(inpatient and SC rooms)
The lesson learnt
• Early PHEM preparedness plan and response was found to play a pivotal role in outbreak mitigation before it becomes public health crisis.
• Having PHEM dedicated budget at district level was found to be crucial in PHEM response.
• Strengthening PHEM data synthesis, analysis and use helps to early respond and shorten the life span of an outbreak.
• Neglecting community rumours on epidemic prone diseases leads to Public Health and economic crisis.
• Sector wide approach (SWAP) is back bone to tackle any public health crisis.
• Stockholders engagements play a vital role in containing public health crisis.
• This disease is preventable if there is strong linkage between health center and health posts and the immunization is given properly.
• Weak monitoring and evaluation system from top to bottom may end up with public health crisis.
• Updated training is needed for health care workers.
• Strong monitoring and evaluation system found to be crucial in early outbreak mitigation.
Strength of the study
This assessment used both primary and secondary data. It also used both qualitative and quantitative data collection methods.
Limitation of the study
There might be possibility of recall bias.
The measles outbreak was occurred in the majority of district Kebeles. The AR and CFR of this outbreak were higher than nationally expected target. Age group of 1-4years had higher attack rate. The AR for both sexes was almost similar whilst the CFR was slightly higher among female. The probable contributing factors for this outbreak were poor health seeking behaviour (poor community awareness and engagement), poor surveillance system, and poor PHEM report completeness, lack of operational surveillance guidelines and protocols, and dalliances of lab specimen result written feedback written recommended time period.
Based on the result of this survey, the following key recommendations are proposed to improve the surveillance system:
• All primary health care units in the district should be actively engaged in active case search and response activities.
• Strong collaboration should exist between PHEM and all programs in general; particularly MCH program.
• ZHD should conduct training gap inventory and train PHEM focal persons on updated guidelines and protocols.
• Community awareness creation and engagement activities on epidemic prone diseases should get due attention at PHCUs levels.
• Strengthening health centers and health posts linkage.
• Strengthening PHEM programs related supportive supervision.
• All epidemic prone diseases should get political attention and should earmark PHEM dedicated budget.
• The regional and national measles diagnosis centers should provide written lab result feedback within recommended time period.
Ethical approval and consent to participate
Ethics approval and consent to participate Ethical clearance was obtained from East Wollega Zonal Health Office, Nekemte, Ethiopia before the actual data collection process was started and brought to the administrative bodies of NunuKumba district health office to get permission for the survey. Brief explanation of the survey objective was given for participants and the process of data collection was started after the willingness of the participant was asked, and then verbal informed consent was obtained from the study participants. All the information obtained from the study participants were kept confidential throughout the process of study, and the name of the participant was replaced by code. Withdrawal from the study at any point if they wished was assured.
Availability of data and material
The finding of this survey is generated from the data collected and analysed based on stated methods and materials. The original data supporting this finding are available from the corresponding author on reasonable request.
Authors’ contributions
Zalalem Kaba Babure and Aklilu Fikadu Tufa conceptualized the study, and responsible for data acquisition. Zalalem Kaba Babure is served as the corresponding author of the manuscript. Zalalem Kaba Babure and Aklilu Fikadu Tufa were responsible for analysis and interpretation of the data. Aklilu Fikadu Tufa provided technical input and review. Zalalem Kaba Babure and Aklilu Fikadu Tufa collaboratively wrote the manuscript. All authors read and approved the final manuscript.
The authors wish to thank East Wollega Zonal Health Office and the staff of NunuKumba district health office for their contribution. This work would not be possible without the aid of the health workers from primary health care units of the district. The authors would specifically like to thank the study participants for their genuine response. Finally, we would also like to exte nd our heartfelt thanks to the data collectors for their invaluable contribution in this assessment.
Citation: Babure ZK, Tufa AF (2021) Bacterial Vaginosis: Evaluation of Measles Outbreak Response Activities and Surveillance System Performance in Nunukumba District, East Wollega Zone of Oromia Region, Ethiopia, June 2020. J Women's Health Care 10:516. doi:10.35248/2167-0420.21.10.516.
Received: 11-Jan-2021 Accepted: 10-Feb-2021 Published: 17-Feb-2021 , DOI: 10.35248/2167-0420.21.10.516
Copyright: © 2021 Babure ZK, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.