Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2020)
Introduction: Diabetes Mellitus (DM) is known to be a chronic multisystem disorder. Since the cutaneous manifestation can be the presenting sign of diabetes mellitus. These are well known and considered common. This work is an attempt to analyze the pattern of various cutaneous manifestations seen in DM in the present lifestyle scenario. In view of increasing prevalence of diabetes mellitus a study of cutaneous manifestation cannot be over emphasized.
Aim: To analyze and study the pattern of cutaneous manifestations in diabetic patients.
Material and methods: An observational single centered study of 18 months was conducted in department of Dermatology and Medicine at tertiary care teaching hospital.
Results: A total of 100 (males were constituted 55% and females were constituted 45%) diagnosed patients of Diabetes Mellitus and were examined. Cutaneous infections were the most common(71%) such as skin tags (33%), cherry angioma (21%), xerosis of skin (19%), acanthosis nigricans (18%), generalized pruritus (12%), xanthelasma palpebraum (8%), diabetic dermopathy (7%), yellow discolouration of hand (5%), diabetic thick skin (2%), rubeosis faciei (2%), and granuloma annulare (1%).
Conclusion: It is important to educate patient for proper self-examination, diet control, exercise, change in lifestyle, regular treatment along with monitoring of blood sugar (HbA1c) at regular intervals to detect infections and other manifestations of DM.
Diabetes mellitus; Cutaneous manifestations; Xanthelasma palpebraum; Diabetic dermopathy; Acanthosis nigricans
Diabetes Mellitus (DM) is known to be a chronic multisystem disorder. As the Health Organisation (WHO) describes it, diabetes mellitus is a metsabolic disorder of various aetiologies characterized by chronic hyperglycemia with disturbances of fat, protein, carbohydrate metabolism which occur as a result of disturbance in insulin action, insulin secretion or both [1,2]. The common clinical symptoms seen ion DM are blurring of vision, weight loss and polyuria. In its severe form; stupor, coma and death are seen due to non ketotic hyperosmolar state in absence of effective treatment. The skin is referred to as window or mirror to the body in health as well as illness. Acute disturbances in the metabolism as well as chronic degenerative complications of diabetes mellitus affect the skin [3]. Even though the mechanism behind these cutaneous remains unknown, certain cutaneous manifestations associated with diabetes mellitus have been pretty well recognized with an incidence rate ranging from 11.3% to 70.6%. Since the cutaneous manifestations can be the first presenting sign of diabetes mellitus [4,5]. These are well known and considered common. This work is an attempt to analyze the pattern of various cutaneous manifestations seen in DM in the present lifestyle scenario [6]. In view of increasing prevalence of diabetes mellitus a study of cutaneous manifestation cannot be over emphasized [7,8].
To analyze and study the pattern of cutaneous manifestations in diabetic patient.
An observational single centered study of 18 months was conducted in department of dermatology and medicine at a tertiary care teaching hospital.
Inclusion criteria
• Patients willing to participate in the study.
• Newly diagnosed cases of Diabetes mellitus.
• Known cases of Diabetes mellitus.
Exclusion criteria
• Patients with Gestational Diabetes mellitus.
• Patients on immunosuppressive drugs.
• Unwilling patients.
A complete general physical, systemic and dermatological examination was carried out each patient to detect the type and extent of cutaneous and systemic ailments present if any. Following routine investigations like hemoglobin, Total leukocyte count, Differential cell count and complete urine examination were done in each patient. Assessment of glycemic control was done in each patient.
The present study was conducted in the department of dermatology of tertiary care teaching hospital. 100 consecutive patients of Diabetes Mellitus with cutaneous manifestations formed the study group.
Table 1 shows patient’s age and sex distribution. Age group varied from 20-79 years with a mean of 52 years and SD of 10.52 years. Minimum age was 25 years and maximum 75 years. Maximum number of patients was in 50-59 years (32%) of age group, followed by age group 40-49 years (27%). Majority of the patients were male (55%) and females (45%) with male to female ration 12:1.
| S.No | Age (Years) | No. of patients (n=100) | Percentage (%) | ||
|---|---|---|---|---|---|
| Male | Female | Total | |||
| 1 | ≤ 29 | 0 | 2 | 2 | 2 |
| 2 | 30-39 | 5 | 3 | 8 | 8 |
| 3 | 40-49 | 14 | 13 | 27 | 27 |
| 4 | 50-59 | 17 | 15 | 32 | 32 |
| 5 | 60-69 | 13 | 12 | 25 | 25 |
| 6 | ≥ 70 | 6 | 0 | 6 | 6 |
Table 1: Age & sex distribution.
Table 2 shows 99% of the patients belong to type II diabetes while only 1% was that of type 1 diabetes mellitus.
| S. No | Type of diabetes mellitus | No. of patients (n=100) | Percentage (%) | ||
|---|---|---|---|---|---|
| Male | Female | Total | |||
| 1 | Type 1/IDDM | 0 | 1 | 1 | 1 |
| 2 | Type II/NIDDM | 55 | 44 | 99 | 99 |
Table 2: Type of diabetes.
Table 3 shows pattern of cutaneous manifestation among diabetic patients. Cutaneous infections were the commonest manifestations present in 71% of patients, followed by the conditions associated with DM, which were present in 67% of patients, miscellaneous cutaneous findings were present in 45% of patients and none of patient had complications due to treatment of diabetes.
| S. No | Cutaneous manifestation | No. of patients (n=100) | Percentage (%) | ||
|---|---|---|---|---|---|
| Male | Female | Total | |||
| 1 | Cutaneous Manifestation | 0 | 1 | 1 | 1 |
| 2 | Cutaneous Condition associated with DM | 55 | 44 | 99 | 99 |
| 3 | Cutaneous Condition associated with treatment of DM | 0 | 100 | 100 | 0 |
| 4 | Miscellaneous cutaneous findings | 45 | 55 | 100 | 45 |
Table 3: Pattern of cutaneous manifestations.
Table 4 shows cutaneous infection/infestations were present in 71 of total patient (100). Most of the patients in infection group had more than one manifestation. Out of 100 patients 50 had fungal infection, 19 had bacterial infections and 6 had viral infection. None of the patient had parasitic infestation.
| No. of patients (n=71) | Percentage (%) | |||
|---|---|---|---|---|
| Male | Female | Total | ||
| Fungal | 29 | 21 | 50 | 50 |
| Dermatophytosis | 23 | 13 | 36 | 36 |
| T. Corporis | 10 | 7 | 17 | 17 |
| T. Cruris | 9 | 5 | 14 | 14 |
| Onychomycosis | 9 | 5 | 14 | 14 |
| T. Pedis | 3 | 1 | 4 | 4 |
| T. Unguium | 2 | 1 | 3 | 3 |
| Candidiasis | 11 | 9 | 20 | 20 |
| Candidal balanoposthitis | 6 | 0 | 6 | 6 |
| Vaginal candidiasis | 4 | 2 | 6 | 6 |
| Cutaneous candidiasis | 0 | 5 | 5 | 5 |
| Candidal paronychia | 1 | 2 | 3 | 3 |
| Bacterial | 8 | 11 | 19 | 19 |
| Folliculitis | 4 | 4 | 8 | 8 |
| Furunculosis | 3 | 5 | 8 | 8 |
| Carbuncle | 1 | 1 | 2 | 2 |
| Cellulitis | 0 | 1 | 1 | 1 |
| Viral | 2 | 4 | 6 | 6 |
| Herpes simplex | 0 | 3 | 3 | 3 |
| Herpes zoster | 2 | 1 | 3 | 3 |
Note: Out of 71 patients 5 patients had single infection and 66 patients had more than one infection.
Table 4: Miscellaneous cutaneous findings.
Table 5 shows the cutaneous conditions associated with DM which were present in 67% of patients. Among the cutaneous conditions skin tag was the most common and was present in 33%, followed by cherry angioma in 21%, xerosis in 19%, acanthosis nigricans in 18%, generalized pruritus 12%, xanthelasma palpebrarum in 8%, diabetic dermopathy in 7% yellow discoloration of skin in 5%, diabetic thick skin in 2%, rubeosis faciei in 2% and granuloma annulare in 1%. Many of these patients had more than one cutaneous condition associated with diabetes mellitus.
| No. of patients | Total | (%) | ||
|---|---|---|---|---|
| Male | Female | |||
| Discoloration of nails | 11 | 0 | 11 | 11 |
| Decrease hair on lower leg | 7 | 3 | 10 | 10 |
| Eczenias | 6 | 4 | 10 | 10 |
| Psoriasis | 3 | 2 | 5 | 5 |
| Pigmented purpuric dermatoses | 3 | 2 | 5 | 5 |
| Lichen planus | 1 | 3 | 4 | 4 |
| Schorrheic keratosis | 2 | 2 | 4 | 4 |
| Alopecia | 2 | 1 | 3 | 3 |
| Nevus | 1 | 2 | 3 | 3 |
| Macular amyloidosis | 0 | 2 | 2 | 2 |
| Vitiligo | 1 | 1 | 2 | 2 |
| Prurigo nodularis | 0 | 2 | 2 | 2 |
| Perforating dermatosis | 0 | 1 | 1 | 1 |
| Syringoma | 0 | 1 | 1 | 1 |
| Urticaria | 1 | 0 | 1 | 1 |
| Acne keloidalis nuchae | 1 | 0 | 1 | 1 |
Table 5: Cutaneous conditions associated with diabetes mellitus.
Table 6 shows miscellaneous cutaneous findings which were present in 45% of total cases. Dicolouration of nails was the commonest, followed by decrease hair over lower legs in 10%, ezemas in 10%, psoriasis in 5%. Apart from these pigmented purpuric dermatoses 5%, lichen planus 4%, schorrheic keratosis 4%, alopecia 3%, nervus 3%, macular amyloidosis 2%, vitiligo 2%, prurigo nodularis 2%, perforating dermatosis 1%, syringoma 1%, urticaria % and acne keloidalis nuchae 1% were also present in decreasing order of frequency.
| No. of patients | Percentage (%) | |||
|---|---|---|---|---|
| Male | Female | Total | ||
| Skin tag | 15 | 18 | 33 | 33 |
| Cherry angioma | 13 | 8 | 21 | 21 |
| Xerosis | 8 | 11 | 19 | 19 |
| Acanthosis nigricans | 7 | 11 | 18 | 18 |
| Gen pruritus | 7 | 5 | 12 | 12 |
| Xanthelasma palpebrarum | 5 | 3 | 8 | 8 |
| Diabetic dermopathy | 5 | 2 | 7 | 7 |
| Yellow discoloration of skin | 3 | 2 | 5 | 5 |
| Diabetic thick skin | 3 | 0 | 2 | 2 |
| Rubeosis faciei | 1 | 1 | 2 | 2 |
| Granuloma annulare | 0 | 1 | 1 | 1 |
Table 6: Miscellaneous Cutaneous.
Table 7 shows number of cutaneous manifestations among diabetic patients. Majority of patients had 3(26%), 4 (25%) and 2 (21%) cutaneous manifestation followed by one (12%), five (9%) and 6 or more than 6 (7%) cutaneous manifestations per patients.
| No. of cutaneous manifestations | No. of patients(n=100) | Percentage (%) | ||
|---|---|---|---|---|
| Male | Female | Total | ||
| 1 | 4 | 8 | 12 | 12 |
| 2 | 14 | 7 | 21 | 21 |
| 3 | 13 | 13 | 26 | 26 |
| 4 | 16 | 9 | 25 | 25 |
| 5 | 6 | 3 | 9 | 9 |
| ≥ 6 | 2 | 5 | 7 | 7 |
Table 7: No. of cutaneous manifestations per patients.
Diabetes Mellitus is the most common endocrine disorder which involves the skin. Many cutaneous disorders are associated with diabetes mellitus.
In the present prospective study, 100 patients were enrolled of age ranging from 25-75 years with mean age 52 years. Majority of the patients were in the age group of 50-60 years 32% followed by 40-50 years 27%. The cutaneous manifestations increase with age duration of diabetes mellitus as well as severity of the disease. Various studies by Mahajan et al. [2], Nigam et al. [3] reported that mostly of these patients were in 51-60 years of age. The relative increase in the incidence of cutaneous involvement with age, duration and severity in diabetic patients may be attributed to the decreased resistance of body as well as long duration of diabetes and poor control of glycemic state. Males (55%) outnumbered females (45%) in our study which is an agreement with previous studies by Sawhey, et al. [4]. The reason for lesser number of females in our study could mainly be because of sheer negligence, lack of awareness and illiteracy on the part of female patients as well as socioeconomic background.
In our study 99% patients had type-II DM, while 1% had type-I DM. In a study by Ragunatha, et al. [5] 98.8% of patients were of type II and 1.2% to type I DM. It possibly reflects the general distribution pattern of type-I DM and type-II DM in the general population.
The increased rate of infections in early part of diabetes onset may be due to decrease in the host defense mechanism and decreased phagocytic activity, which is noticed immediately in uncontrolled diabetes.
Fungal infections (50%) were the commonest infections followed by bacterial (19%) and viral (6%). This is an accordance with other such studies by Mahajan et al. (54.68%) [2]. However similar studies by Yosipovith et al. [9] reported incidence of fungal infection 32%. This may be due to geographical area hot and humid climate as ewll as poor personal hygiene of patients. This may be because of most of the patients in our study were from lower socioeconomic group from rural areas where hot and humid climate conditions with poor hygiene, overcrowding and negligence.
Among the 19 patients having bacterial infections, folliculitis and frunculosis were present in 8 patients each carbuncle in 2 while cellulitis was present in 1 patient. This may again be due to geographical area, climatic condition and personal hygiene of patients (Figures 1 and 2).
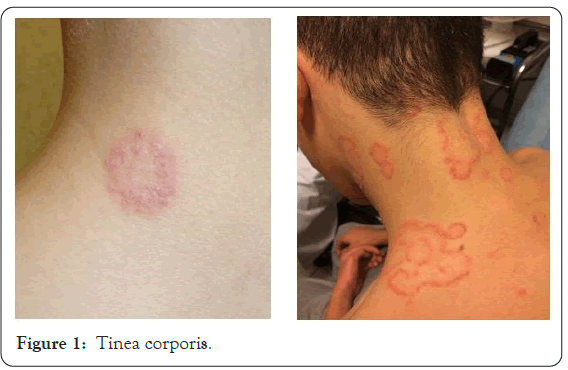
Figure 1: Tinea corporis.

Figure 2: Folliculitis.
Among the viral infections herpes simplex and herpes zoster were present in 3 patients each. Similar results were seen by Bhat et al. [6].
Among the cutaneous conditions associated with diabetes mellitus, Skin tags were the commonest and were present in 33% of patients in our study. Various studies by Kahana et al. [7] and Thappa et al. [8] observed that skin tags were present in 26.3% and 62.85% of the cases respectively (Figure 3).
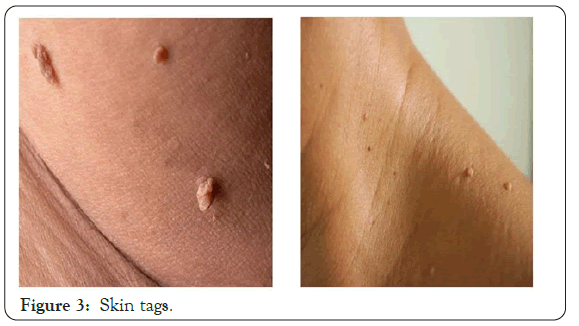
Figure 3: Skin tags.
In the present study, cherry angiomas were present in 21% patients while in a similar study by Arora et al. [10] observed cherry angioma in 44.8% of diabetic patient.
Acanthosis nigricans was present in 18% of the patients in our study, whereas Mahajan et al. [2], Bhat et al. [6] reported a slight lower incidence of acanthosis nigricans in their study 3% and 5.3% (Figure 4).

Figure 4: Acanthosis nigricans.
Apart from infectious and cutaneous conditions associated with diabetes, there are several other miscellanous cutaneous findings like discoloration of nail, decrease hair density over lower legs, eczemas, psoriasis, lichen planus and alopecia, amyloidosis, urticaria, perforating disorder of skin. In the present study discoloration), lichen planus of nail (11%), decrease hair over lower legs (10%), psoriasis (5%), pigmented purpuric dermatosis (5%), lichen planus (4%), seborrheic keratosis (4%), alopecia (3%), nevus (3%), macular amyloidosis (2%) and urticarial (1%). Out of these some of the conditions like vitiligo, alopecia, lichen planus is known to be present in diabetic mellitus cases as a part of autoimmune syndrome and poly endocrinopathy.
Number of cutaneous manifestations in our study were comparatively higher because a large percentage (64%) of our patients had uncontrolled diabetes. Poor hygiene, climatic conditions, illiteracy, diet, food habits and lower socioeconomic and rural background may be the additional factors.
Diabetes Mellitus is a systemic disease involving various organs. Skin is one of the important organs to reflect various changes of diabetes mellitus. Manifestations like cutaneous infections appear in early part of the disease. In many patients diabetes may remain undetected and the patients are not tuned to regular checkup of their blood sugar. Hence it is very important to educate patient.
Citation: Garg P, Chandra M, Rajauria G (2020) Evaluation of Cutaneous Manifestation of Diabetes Mellitus. J Clin Exp Dermatol Res. 11:542.
Received: 13-Nov-2020 Accepted: 27-Nov-2020 Published: 04-Dec-2020
Copyright: © 2020 Garg P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.