Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2020)Volume 5, Issue 2
Objective: Introduction: the neonatal health of premature babies remains a major concern. Kangaroo Care is an effective method of taking care of premature babies and is a good alternative, to make up for the insufficient supply of conventional care. The objective of the study was to assess the implementation of a kangaroo care unit at the Ziguinchor Peace Hospital.
Materials and method: These were a descriptive study from May 1, 2018 to July 31, 2019, in the pediatrics department of the Ziguinchor Peace Hospital. Included were newborns weighing between 750 and 1810 grams on admission to the kangaroo care unit. Excluded were newborns whose length of stay in the kangaroo care unit was less than 72 hours. We have studied the socio-epidemiological data; obstetric and neonatal data and evolutionary data.
Results: During the study period, 81 newborns (49 boys and 32 girls) were collected, representing a prevalence of 25,9% of all deliveries. The average gestational age was 33 weeks of gestation (28-40,6) and the average admission weight was 1510 grams (750-1810). The main pathologies and neonatal complications, associated with prematurity before starting kangaroo care, were hypothermia in 39 cases (48,1%); respiratory distress in 34 cases (42%); hypoglycemia in 29 cases (35,8%); neonatal infection in 21 cases (25,9%). Kangaroo care was started on average 3 days after the date of hospitalization. The mean follow-up weight was 2025 grams (1510-2470). The mean temperature was stable at 36,6°C (35,9-39°C). Eleven (11) children had hypothermia. The average blood sugar was 0,99 g / l (0,81 to 1,10 g /l). No newborn had hypoglycemia during kangaroo care. The length of hospital stays varied between 5 and 29 days. We deplored 04 cases of death. The average weight gain was 11,1 g / kg / day.
Conclusion: The incidence of prematurity is high at the Ziguinchor Peace Hospital. Kangaroo care is an alternative to the insufficient supply of conventional care. We recommend training medical and paramedical staff and building a large room to formalize kangaroo care activities.
Pediatrics; Premature; Ziguinchor peace hospital; Kangaroo care
In developing countries, neonatal health is a real public health problem. In Senegal, neonatal mortality was estimated at 28% in 2017, thus representing half of infant and child mortality [1]. The leading causes of death for newborns worldwide are prematurity (36%), perinatal asphyxia (23%) and sepsis (15%). Premature babies and hypotrophs are very vulnerable and exposed to many complications such as sepsis, metabolic disorders and neurosensory disorders at a distance [2]. One of the objectives for sustainable development is to eliminate avoidable deaths of newborns and children under 5 by 2030. Indeed, all countries will have to seek to reduce neonatal mortality to 12% live births at most, and infant and child mortality at 25% live births at most. A reduction in neonatal mortality is necessary to achieve this goal, which implies an improvement in the survival of premature babies. Among the problems linked to this survival, hypothermia and diet are very important elements. Kangaroo Care (KC) is an effective method of taking care of premature babies and is a good alternative, in developing countries like Senegal, to make up for the insufficient supply of conventional care [3,4]. This is about promoting skinto- skin, mother-child contact, helping to avoid hypothermia, promoting breastfeeding and strengthening the mother-child bond.
The Ziguinchor Peace Hospital (HPZ) has a pediatric service which started operating in 2015. It is in this context that our work was carried out. The main objective of the study was to assess the implementation of a KC unit within the pediatric service of the HPZ. The specific objectives were to study the effectiveness of KC in terms of growth and thermoregulation, to evaluate eating habits, to describe complications.
Study site
Our study took place in the pediatric department of the HPZ. The hospital is a benchmark hospital-university structure in the Ziguinchor region and in the sub-region. It has a pediatric service with a capacity of 30 beds. The medical staff of the HPZ pediatrics service is made up of three pediatricians (a university assistant, two hospital practitioners). The paramedical staff is made up of a state nurse, service supervisor, six (06) state nurses, four (04) nursing assistants and one (01) surface technician. The pediatric service has four (04) units: outpatient; the center for rehabilitation and nutritional education; hospitalizations and neonatology. The neonatology unit consists of a large room containing eight (08) cradles, one (01) heating table and one (01) incubator. It also has an annex room with a capacity of 4 beds for mother and child hospitalization.
Type and duration of study
It is a descriptive and analytical study over a period of 14 months from May 1, 2018 to July 31, 2019.
Study population
Our study population consisted of infants weighing less than 2,000 grams.
Inclusion criteria: Included in the study newborns weighing between 750 and 1810 grams on admission to the KC unit of the Pediatric Department of the HPZ.
Exclusion criteria: newborns whose duration of stay in the KC unit was less than 72 hours were excluded from the study.
Operation of the kangaroo care unit
For the purposes of this study, a room with a capacity of 4 beds was fitted out for hospitalization. Newborns were admitted directly or after an incubation period. A pre-inclusion interview was done with the parents. The ventral portage was done by the mother with a light loincloth, for a variable duration from 6 to 8 hours per day. Feeding generally begins with a probe then, depending on the level of neurological maturation, it is administered by syringe, cup and finally by feedings or bottles. Breast milk was favored, with supplementation of artificial milk adapted to needs.
Mothers provided most of the care for their child (breastfeeding or other methods, babywearing, toilets, etc.). They were assisted by a nurse who provided daily weighing, temperature readings (every 3 hours) and the administration of medication. Capillary blood sugar is assessed based on clinical status and food self-sufficiency.
Continuous information, education and communication sessions were held in the unit during which mothers and care givers were made aware of the care of premature newborns, the importance of hygienic and infection prevention rules, strategies favoring breastfeeding and KC benefits.
KC continued at home with weekly follow-up when the child was independent and had a satisfactory weight gain (15g / kg / d for 3 days). The KC is usually stopped when the newborn reaches 2500 grams or when he no longer tolerates the kangaroo position.
Data collection and analysis
The data was collected from the hospital medical record and the KC inclusion and follow-up sheet. We studied the following parameters:
• Socio demographic and epidemiological data of the mother: age, address, marital status, professional activity, level of education.
• Obstetric data: number of antenatal consultations, obstetric pathologies, delivery, term of pregnancy, place and route of delivery, number of fetuses, antenatal corticosteroid therapy.
• Neonatal data: sex; weight; conventional care events with associated pathologies and neonatal complications; the type and mode of feeding the newborn.
• Evolutionary data: weight change (daily weight gain, weight on admission to and departure from the unit, weekly weight); monitoring of body temperature; complications; length of stay in KC unit.
• The criteria for judging the effectiveness of the method were: daily weight gain; the absence of hypothermia; the absence of hypoglycemia and the percentage of survival.
During the period of our study, we registered 313 newborns. Among these children, we listed 96 premature deliveries and/or hypotrophy, a prevalence of 30.7%. Newborns weighing less than 2,000 grams constituted 81 cases (49 boys and 32 girls). This makes a prevalence of 25.9% of all deliveries.
Sociodemographic and epidemiological data
Our parturients were between 14 and 46 years old. They came from the municipality of Ziguinchor in 46% of the cases, against 54% outside the municipality of Ziguinchor. Fifty-one-point eight percent (51,8%) of parturients were housewives. In the group of women without professional activity, there were 04 female students and 21 secondary school pupils. Almost 1/3 of the mothers were single. Table 1 summarizes the socio-demographic and epidemiological data.
| Sociodemographic and epidemiological data | Effective | Percentage (%) | |
|---|---|---|---|
| Mother's age (years) | 14 – 18 | 10 | 12,4 |
| 19 – 35 | 59 | 72,8 | |
| 36 – 46 | 12 | 14,8 | |
| Matrimonial property regime | Single | 22 | 27,2 |
| Married | 56 | 69,1 | |
| Widowed | 2 | 02,5 | |
| Divorcee | 1 | 01,2 | |
| Socio-economic level | Low | 49 | 60,5 |
| Way | 29 | 35,8 | |
| High | 3 | 03,7 | |
| Schooling of the mother | Yes | 62 | 76,5 |
| No | 19 | 23,5 | |
| Mother's profession | Housewife | 42 | 51,8 |
| Official | 3 | 03,8 | |
| Other function | 11 | 13,6 | |
| Student | 25 | 30,8 | |
Table 1: Distribution of the population according to socio-demographic and epidemiological data
Obstetric data
The number of antenatal consultations was greater than or equal to 4 in 26 patients (or 32,1%). The pregnancy was twin in around 1/3 of the cases (n = 26 or 32,1%). The most common obstetric pathologies were eclampsia and pre-eclampsia (32,1%), premature rupture of the membranes (19,7%) and anemia (18,5%). The term of pregnancy was less than 34 weeks of gestation in 36 parturients, 05 of whom had received antenatal corticosteroid therapy. The delivery took place at the maternity hospital of the HPZ in 83,9% of the cases. Table 2 summarizes the distribution of the population according to obstetric data.
| Obstetric data | Variable | Effective | Percentage (%) |
|---|---|---|---|
| Number of prenatal consultations | < 4 | 55 | 67,9 |
| ≥ 4 | 26 | 32,1 | |
| Number of fetus | Single pregnancy | 54 | 66,7 |
| Twin pregnancy | 26 | 32,1 | |
| Trimellar pregnancy | 1 | 01,2 | |
| Obstetric pathology | Eclampsia and pre-eclampsia | 26 | 32,1 |
| Premature rupture of members | 16 | 19,7 | |
| Anemia | 15 | 18,5 | |
| Urogenital infection | 3 | 03,7 | |
| Retroplacental hematoma | 2 | 02,5 | |
| Delivery route | Cesarean section | 39 | 48,1 |
| Low Birth | 42 | 51,9 | |
| Place of birth | Health post | 2 | 02,5 |
| Health center | 8 | 09,9 | |
| Home | 3 | 03,7 | |
| Hospital | 68 | 83,9 | |
| Ante corticosteroid therapy | Not specified | 31 | 38,3 |
| Not indicated | 45 | 55,6 | |
| Done | 5 | 06,1 |
Table 2: Distribution of the population according to obstetric data
Neonatal data
The 81 newborns were received immediately at the unit, at an average of 16 minutes with extremes ranging from 3 to 240 minutes after birth, accompanied by a mother-child liaison form.
Gestational age was determined in 38,3% (31 newborns) of cases by the date of their last period; in 54.3% (44 newborns) of the cases by an early ultrasound and in 07,4% (6 newborns) of the cases by a score of maturation on the clinical examination of the child at birth. The average gestational age was 33 weeks of gestation (28– 40,6). There were 19 neonates (23.4%) of very premature babies born between 28 and 32 weeks of gestation. Moderate premature babies born between 32 and 36.6 weeks of gestation were 41 newborns (50,6%). The remaining 21 (25,9%) newborns were term hypotrophs, between 37 and 40 weeks of gestation.
The average weight at inclusion was 1510 grams (750 to 1810). The number of newborns weighing between 750 and 1500 grams was 28, or 34,6%; and those weighing between 1500 and 1810 grams were 53 in number, or 65,4%.
The main neonatal pathologies and complications, associated with prematurity before the onset of KC, were hypothermia in 39 cases (48,1%); respiratory distress in 34 cases (42%); hypoglycemia in 29 cases (35,8%); neonatal infection in 21 cases (25,9%). Table 3 gives the distribution of newborns according to neonatal pathologies and complications.
| Clinical picture | Effective | Percentage (%) |
|---|---|---|
| Hypothermia | 39 | 48,1 |
| Respiratory distress | 34 | 42,0 |
| Hypoglycémia | 29 | 35,8 |
| Neonatal infection | 21 | 25,9 |
| Neurological distress | 15 | 18,5 |
| Jaundice | 13 | 16,0 |
| Food difficulty | 13 | 16,0 |
| Hyperglycémia | 8 | 09,9 |
| Hyaline membrane disease | 8 | 09,9 |
| Shock | 6 | 07,4 |
| Apnea of prematurity | 4 | 04,9 |
| Perinatal asphyxia | 3 | 03,7 |
| Abdominal bloating | 3 | 03,7 |
| Ulcerative necrotizing enterocolitis | 1 | 01,2 |
| Pallor | 1 | 01,2 |
Table 3: Distribution of newborns according to clinical presentation and complications
Therapeutic and evolutionary data
Newborns admitted were hospitalized directly in the KC unit in 64,2% of cases (n = 5-2 newborns) or after a brief stay in neonatology, in an open incubator (hot table) in 35,8% cases (n = 29 newborns).
SK was started on average 3 days after the date of hospitalization with extremes of 0 to 14 days. More than half (n = 47 or 58%) of the mothers started KC within 72 hours of birth.
The average weight at follow-up was 2025 grams (1510 – 2470). The mean temperature was stable at 36,6°C (35,9 - 39°C). Eleven (11) children had hypothermia with a temperature below 36°C. The average blood sugar was 0,99 g / l (0,81 to 1,10 g / l). No newborn had hypoglycemia during kangaroo care. Figure 1 summarizes the evolution of the weight; temperature and average blood sugar.
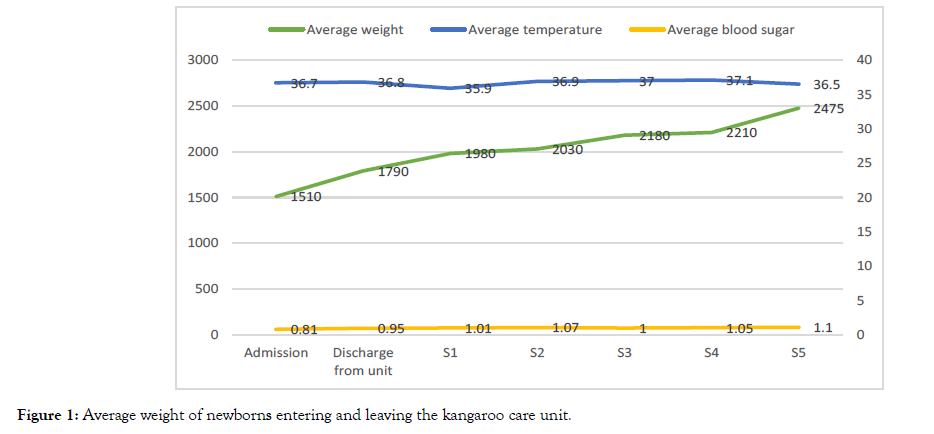
Figure 1: Average weight of newborns entering and leaving the kangaroo care unit.
Newborns received exclusive breastfeeding in 80,2% of the cases, mixed breastfeeding in 17,3% of the cases and artificial breastfeeding in 2,5% of the cases. In 05 cases the feeding of the newborn was passive with the use of a nasogastric tube.
The length of hospital stays in the KC unit ranged from 5 to 29 days with an average of 10 days.
We deplored 04 cases of death occurring on weekends. The mortality rate was 04,9% (04 deaths out of 81 newborns). A newborn had a swelling of the right hip after three days requiring a withdrawal from KC.
The average weight gain in hospital was 11,1 g / kg / day (3,4–27,2 g / kg). On an outpatient basis, the weight gain was greater by 12,7 g / kg / day (4,3–28,9 g / kg).
Thirty-six (37) newborns had a weight gain of less than 10 g / kg / day; 23 newborns had a weight gain between 10 and 15 g / kg / day and 21 newborns had a weight gain of more than 15 g / kg / day.
SKs are an effective method of managing premature babies. They are a good alternative, in certain health facilities in Senegal such as the HPZ, to make up for the insufficient supply of conventional care [3,4]. The pediatric department of the HPZ only has an incubator and a heating table. However, the neonatology of HPZ is a level II reference unit in the management of newborns and children under 2 months of age. It polarizes the whole region of Ziguinchor; the northern zone of the Kolda region and the sub-region (Gambia, Guinea Bissau). In fact, more than half of our parturients came from outside the municipality of Ziguinchor (54% compared to 46% from the municipality of Ziguinchor). The incidence rate of premature babies in our series was 25,9% (81 newborns), which is very high compared to the national average of 12% in 2017 [1].
World Health Organization (WHO) estimates that premature newborns represent 17% of all live births. This frequency varies from country to country, ranging from 6% in developed countries to 28% in developing countries [5,6].
This increase in prematurity is partly explained by the fact that HPZ is a benchmark structure in the management of newborns. Slightly lower rates (23,8% prematurity) were found in the same region in 2013 [7].
The high incidence rate of prematurity at HPZ justifies the urgency of setting up an SK unit in the hospital.
The main neonatal pathologies and complications, associated with prematurity before the onset of SK, were hypothermia in 39 cases (48,1%); respiratory distress in 34 cases (42%); hypoglycemia in 29 cases (35,8%); neonatal infection in 21 cases (25,9%). These complications were found only in newborns admitted to neonatal resuscitation. They are classic prematurity and had been found by other authors [8-18].
At inclusion, the average weight of our cohort was 1510 grams, slightly higher than the Indian series of 1460 grams, but substantially equal to the Senegalese series of 1570 grams [19,20]. Unlike some series, the weight group 1500-1810 grams were the most represented, with 53 newborns, or 65,4%. In India, 76% of newborn babies weighed less than 1500 grams [19]. The predominance of children over 1500 grams in our cohort could explain our results.
In our cohort, 80,2% of children received exclusive breastfeeding, 17,3% mixed breastfeeding and 02,5% breastfeeding. The rate of exclusive breastfeeding in KC found in Dakar was 73,5% [20] lower than that found. This low rate of exclusive breastfeeding is a relative failure from the original KC goal. Teams should be more resistant to the introduction of formula milk. In principle, exclusive breastfeeding should be 100% encouraged and encouraged. We did not reach this goal due to the insufficient production of milk by the mother, unavailability of the mother.
Breastfeeding was the main food in our cohort. Indeed, it has been proven that in the same way as in skin-to-skin contact, breastfeeding contributes to the strengthening of the mother-child relationship and improves the neuro-developmental outcome of the newborn. The use of the probe (06,2% in our study) was essentially justified in the absence of an effective reflex of sucking and swallowing, the problem of the nipple and the absence of the mother.
The goal of KC nutrition is regular weight gain of 10-15 g / kg / day as in intrauterine life. In our cohort, the average weight gain was 11,1 g / kg / day in the unit and 12,7 g / kg / day in the outpatient setting, figures which approximate that of Dakar, the average of which was 16 g / kg / day [20].
The main objective of KC is to maintain the temperature. Obtaining good thermoregulation is the key to KC success. The results of our study show that this objective is achieved because we only noted 11 cases of hypothermia episodes. Several other studies have shown a significant reduction in hypothermia [19,20]. In the Dakar study, 3 cases of hypothermia out of 102 new patients followed in KC were reported [20]. In India no cases of hypothermia have been noted in newborns entering the program [19].
The average weight at the exit of the unit was 1790 grams, close to the 1933-gram series in Dakar [20] and other African series of 2000 grams [21,22]. This during the SK was continued at home for most of the patients.
As in our cohort there was no case of infection in KC. In Dakar, Faye et al., found a significant reduction of 20% in the risk of infection, especially nosocomial, of newborns followed in SK compared to newborns followed in conventional care. No newborns had been readmitted to conventional care. This confirms one of the main advantages of KC which is less invasive than conventional care [23].
Indeed, newborns followed in KC do not benefit from perfusion and are therefore less exposed to infections, especially nosocomial infections. However, the rules of hygiene and asepsis must be strictly observed.
The mortality rate observed in our study was 04%. All of the deaths occurred on weekends characterized by the absence of the KC unit nurse. This figure was close to the Dakar series, 3,7% and Adiss Ababa, 4% [20,22].
These results, although encouraging, clearly show the effort that must be made to reach the objective of zero deaths in KC units.
The incidence rate of prematurity is high at HPZ. KCs are an alternative to the insufficient supply of conventional care. We recommend training medical and paramedical staff and building a large room to formalize KC activities.
Citation: Thiam Lamine, Diouf F Niokor, Seck Ndiogou, Niang Babacar, Isabelle Jokébé, Fall Amadou Lamine et al. (2020) Establishment of a Kangaroo Care Unit at the Peace Hospital in Ziguinchor/Senegal: Preliminary Study. Clin Pedia OA 5:166 doi: 10.35248/2572-0775.20.5.166
Received: 05-Mar-2020 Accepted: 04-Jun-2020 Published: 11-Jun-2020 , DOI: 10.35248/2572-0775.20.5.166
Copyright: 2020 © Lamine T, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Competing interests: The authors have declared that no competing interests exist.