Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2019)Volume 10, Issue 1
Melanoma a type of skin cancer derived from melanocytes which represents around 4% of all skin cancers recorded till date, but is responsible for 80% deaths due to skin tumors. The development of new targeted therapies directed specifically against malignant cells has brought hope to the treatment of melanoma patients. The first drugs developed against specific molecules were BRAF inhibitors, designed for the treatment of metastatic melanoma. These drugs have been demonstrated to improve both overall and disease-free survival in these patients. At the same time, a wide range of adverse events (AEs) have emerged from their use. Some of them are quite frequent and are observed regularly in everyday practice on the other hand, there are rare AEs that require an early diagnosis for adequate treatment so knowledge of their existence is crucial for timely recognition and patient management. We here have presented a case of erythema nodosum-like septal panniculitis in a patient receiving therapy with vemurafenib and cobimetinib.
Melanoma; BRAF inhibitors; Vemurafenib; Adverse events; Erythema nodosum; Panniculitis
Melanoma is a type of skin cancer derived from melanocytes, whose I ncidence has grown during the last decade. Even though it represents only 4% of all skin cancers, it is responsible for 80% of deaths from skin tumors and one of the most important in terms of years of potential life lost [1]. However, the development of new targeted therapies directed specifically against malignant cells has brought hope to the treatment of melanoma patients. The first drugs developed against specific molecules were BRAF inhibitors, designed for the treatment of metastatic melanoma with positivity for V600E BRAF mutation, which occurs in 40-60% of melanomas, especially in those arising in areas without chronic sun exposure [2]. These drugs have been demonstrated to improve both overall and disease-free survival in these patients [3]. At the same time, a wide range of adverse events (AEs) have emerged from their use. We must be familiar with these AEs since they can cause significant morbidity and even force discontinuation of therapy. Some of them are quite frequent and are observed regularly in everyday practice, such as maculopapular rash, photosensitivity, xerosis, keratosis pilaris or epithelial neoplasms [4]. On the other hand, there are rare AEs that require an early diagnosis for adequate treatment, so knowledge of their existence is crucial for timely recognition and patient management. Examples of these are neutrophilic dermatosis such as Sweet syndrome, eccrine neutrophilic hydradenitis and neutrophilic panniculitis [5]. We present a case of erythema nodosum-like septal panniculitis in a patient receiving therapy with vemurafenib and cobimetinib.
A 43-year-old male was diagnosed with melanoma of unkown primary after consulting for a painful right axillary lymphadenopathy. Fine needle aspiration biopsy of the lymphadenopathy demonstrated epithelioid melanoma metastatic cells. Complete study of the patient revealed no signs of primary melanoma but detected left inguinal adenopathies, two lung metastases and one splenic metastasis. The patient started on combined therapy with vemurafenib and cobimetinib.
One month later, the patient consulted in the Emergency Department for asthenia, malaise, high fever, and arthralgias that did not improve with non-steroidal antiinflammatory drugs (NSAIDs). Physical examination revealed infiltrated, erythematous, ill-defined and painful subcutaneous nodules on the proximal upper (Figure 1) and lower extremities. They were also present to a lesser extent in the abdomen. A punch biopsy was performed and the patient was treated with oral perdnisone 45 mg daily, with discontinuation of therapy for melanoma.
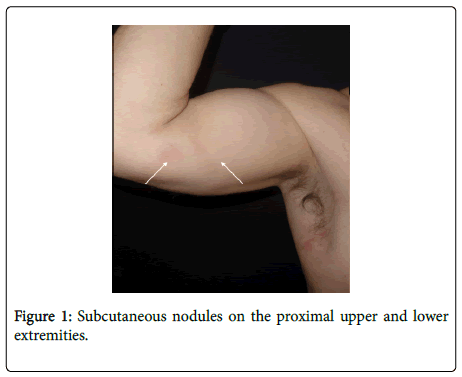
Figure 1: Subcutaneous nodules on the proximal upper and lower extremities.
Histological examination demonstrated a discrete superficial and deep perivascular inflammatory dermal infiltrate, associated with a dense neutrophilic infiltrate in the subcutaneous tissue septa, which in some areas extended partially into the lobules. There were multiple granulomatous-like structures composed by histiocytes encircling a clear central space and surrounded by a dense neutrophilic infiltrate, findings characteristic of Miescher's granulomas (Figure 2).
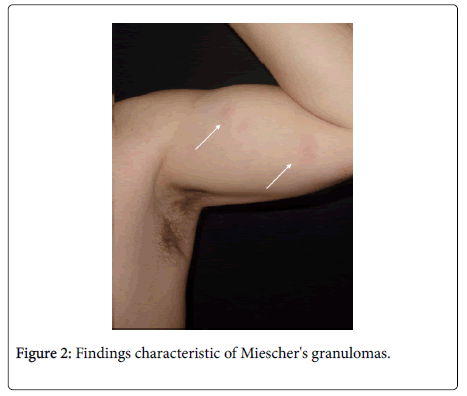
Figure 2: Findings characteristic of Miescher's granulomas.
The patient's symptoms and lesions resolved 2 weeks later, so steroid therapy was tapered down. One month later, both vemurafenib and cobimetinib were reintroduced, with subsequent reapparance of the same lesions. Adequate control was achieved with low-dose prednisone without requiring discontinuation of vemurafenib or cobimetinib.
Neutrophilic panniculitis is a rare AE of BRAF inhibitor therapy, drugs used to treat metastatic melanomas with BRAF gene mutation. This type of panniculitis has also been described in children and adolescents with central nervous system tumors treated with vemurafenib [6]. So far, there have been over 20 cases reported of panniculitis associated with the use of BRAF inhibitors in metastatic melanoma (Table 1). This AE is mostly reported with BRAF inhibitors as monotherapy, and among these, it is more frequent with vemurafenib than dabrafenib. It has not been described in patients receiving MEK inhibitors exclusively. A recent report described a case of panniculitis associated to combined therapy with vemurafenib and cobimetinib that resolved and relapsed with the latter's removal and reintroduction, respectively [7]. This might be the first case of panniculitis associated to MEK inhibitor therapy, though it may also be a coincidental observation, as the majority of case reports describe resolution of lesions, either spontaneously or with NSAIDs, withour discontinuation of BRAF inhibitor therapy.
| Authors | Gender, Age (years) | Melanoma type (location of metastases) | BRAFi ± other | Symptoms | Time of BRAFi therapy until onset | Systemic symptoms | Histology (type of panniculitis) | Treatment | BRAFi discontinuation | Course | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Maldonado-Seral et al. [14] | F, 42 | SSM (lung) | V | Nodules in legs | 2 weeks | No | Lobular, neutrophilic and histiocytic | None | No | Resolution in a few days | |
| Monfort et al. [15] | F, 70 | ALM (lung, mediastinum, abdomen, central nervous system, subcutaneous, lymph node) | V | Painful nodules in legs | 15 days | No | Neutrophilic | None | No | Resolution in 15 days | |
| Monfort et al. [15] | F, 38 | ¿? (subcutaneous, lymph node, parotid, lung) | V | Painful nodules in arm | 10 days | Arthralgias | Lobular neutrophilic panniculitis, deep neutrophilic dermatitis | No | Resolution in 5 days, some relapses | ||
| Zimmer et al. [11] | F, 44 | MUP (lymph node, lung, mesentery, bone) | V | Painful nodules in arms, legs and gluteus | 16 days | Generalized arthralgias | Lobular neutrophilic panniculitis, small vessel vasculitis | Prednisolone 1 mg/kg, indomethacin, dipyrone | Yes | Resolution in 11 days, reintroduction of V at 25% dose, relapse of arthralgias 5 days later, but no subcutaneous nodules | |
| Zimmer et al. [11] | F, 59 | ALM (lymph node, lung, liver, bone) | V | Painful nodules in arms and legs | 7 days | Mild arthralgias | Septolobular neutrophilic panniculitis | Etoricoxib | No | Resolution in 4 weeks | |
| Shina et al. [10] | F, 45 | ¿? | V | Painful nodules in arms and legs | 37 days | Rash (Grade 3), arthralgias, conjunctivitis, photoensitivity | Erythema nodosum-like panniculitis | Analgesics | Yes (3-4 days) | Spontaneous resolution, reintroduction of V at 35% dose | |
| Shina et al. [10] | M, 26 | ¿? | V | Painful nodules in arms and legs | 31 days | No | Erythema nodosum-like panniculitis | None | Yes (3-4 days) | Spontaneous resolution | |
| Kim et al. [16] | F, 52 | ¿? (lymph node) | V | Erythematoviolaceous plaques in legs | 2 weeks | Arthralgias | Lobular neutrophilic panniculitis | None | No | Spontaneous resolution in months | |
| Choy et al. (series of 9 patients, one initially D and later D + T) [8] | 4F, 5M, mean 39 (29-71) | ¿? | 4V 3D 3D+T |
Erythematous nodules in legs, arms and trunk | Mean 48 days (3-195 days) | Arthralgias (7 of 9 patients) | 8 biopsies of 7 patients: 5 lobular panniculitis (4 neutrophilic, 1 lymphocytic, 3 mixed). 3 mixed panniculitis (one with vasculitis) |
None or NSAIDs. Oral prednisone in 3 patients |
No | Complete resolution | |
| Ramani et al. [3] | F, 50 | ALM (lung, lymph node) | D | Nodules in legs and arms | 8 weeks | No | Lobular neutrophilic panniculitis , necrotizing granulomas | Doxycyclin 2 weeks | No | Resolution in 2 weeks, at 8 weeks disease progression (cerebral metastases) and exitus | |
| Weng et al. [12] | F, 75 | MUP (lymph node, mediastinum, lung) | V | Painful erythematous nodules in legs, arms and abdomen | 1 week | No | Mixed neutrophilic panniculitis | Prednisone and celebrex | Dose reduction (halved) | Resolution in 5 weeks. After increasing dose, relapse of lesions, with subsequent dose reduction (halved) | |
| Ferreira J et al. [17] | F, 35 | Nevoid MM (lung, bone, liver, central nervous system) | V | Painful nodules in legs | 6 weeks | No | Lobular neutrophilic panniculitis | Oral and topical corticoids | No | Complete resolution, no relapses | |
| Ferreira J et al. [17] | F, 65 | SSM (lung, skin) | V | Painful nodules in arms and legs | 10 days | Fever, arthralgias, rash | Lobular neutrophilic panniculitis , foci of necrosis and apoptosis | None | Dose reduction | Complete resolution | |
| F: Female; M: Male; BRAFi: BRAF inhibitor; V: Vemurafenib; D: Dabrafenib; T: Trametinib; SSM: Superficial spreading melanoma; ALM: Acral lentiginous melanoma; MUP: Melanoma of unknown primary | |||||||||||
Table 1: Cases of panniculitis as associated to the use of BRAF inhibitors in patients with metastatic melanoma reported in the literature.
BRAF inhibitor-associated panniculitis is over two times more frequent in females than in males, and among patients treated with vemurafenib, it is more common in those with lung metastases. However, this last observation might be due to the high frequency of metastases in this location and have no pathogenic link to the development of panniculitis.
The majority of cases reported appeared early during therapy, between the 2nd and 3rd weeks of treatment. In the case series reported by Choy et al. lesions appeared later on (mean 48 days, range 3-195 days) [8]. Clinical presentation simulates erythema nodosum, with painful, erythematous nodules predominantly on the anterior aspect of the legs, although arm involvement is also frequent. They may be accompanied by systemic symptoms, usually with fever and arthralgias, in up to 60% of cases. Differential diagnosis should include subcutaneous metastasis of melanoma, so skin biopsy is required [8,9].
Histologic examination of reported cases reveal heterogeneous characteristics. These panniculitis are predominantly lobular and are composed of a neutrophilic infiltrate. Mixed septolobular panniculitis have been described in 4 patients, though the cases reported by Shina, et al. presented erythema nodosum-like panniculitis, similar to our case [10]. Pathology of our patient's lesions demonstrated a predominantly septal panniculitis, a dense neutrophilic infiltrate and multiple Miescher's radial granulomas. Though these are not pathognomonic, they are very typical of early erythema nodosum lesions. This is the first report of BRAF inhibitor-associated neutrophilic panniculitis with these histopathological findings.
These lesions usually resolve in a few days without requiring discontinuation of BRAF inhibitor therapy. However, as in our case, relapses after resuming therapy or increasing dose have been reported [11,12]. Treatment is symptomatic and usually analgesics and NSAIDs suffice, though some cases may require systemic corticosteroids, as did our patient. Some authors recommend using oral corticosteroids as initial treatment due to the intense pain these lesions can cause, which might even motivate discontinuation of therapy [13]. Each individual case must be carefully assessed before making the decision to interrupt BRAF inhibitor therapy [14].
In conclusion, we present a new case of BRAF inhibitor-associated erythema nodosum-like panniculitis presenting in a patient receiving combined therapy with vemurafenib and cobimetinib. Though the patient experienced a relapse after reintroducing therapy, avoiding a second discontinuation was possible due to adequate control with lowdose oral prednisone.
Citation: Tapial JM, Oñate CV, Martínez-Doménech Á, Ferrer DS, Pastor GP, et al. (2019) Erythema Nodosum-like Panniculitis Associated with the Use of Vemurafenib. J Clin Exp Dermatol Res 10:481.
Received: 03-Dec-2018 Accepted: 05-Jan-2019 Published: 01-Dec-2019
Copyright: © 2019 Tapial JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.