Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2020)
Epidermolysis Bullosa Acquisita (EBA) is a chronic autoimmune subepidermal blistering disease developed after damage to type VII collagen by autoantibodies. Type VII collagen is the major component of anchoring fibrils in the sub-lamina densa hemidesmosomes of the skin and squamous mucosas. The worldwide incidence is estimated between 0.2-0.5/million inhabitants per year. Two major clinical variants have been described: the mechanobullous, and the inflammatory EBA.
Epidermolysis bullosa; Autoimmune subepidermal; Hemidesmosomes
A 52-year-old female who presented with disseminated cutaneous plaques, focal presence of millium cysts, and hypopigmented atrophic scars on her trunk and extremities. In the inguinal region there were some tense blisters with erosive areas (Figure 1) [1,2]. Additionally, patient showed nail dystrophy, partial loss of toenails, moderate fibrosis of the fingers and multiple oral erosions (Figure 2) [3-5].
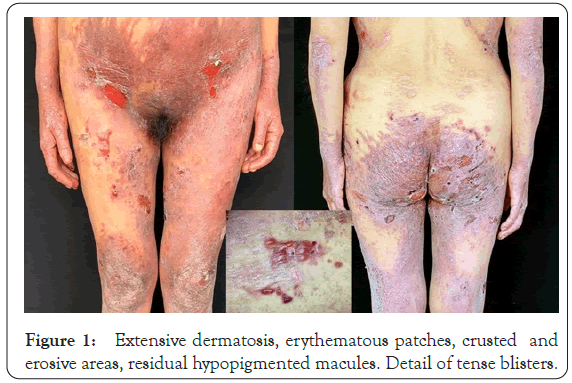
Figure 1: Extensive dermatosis, erythematous patches, crusted and erosive areas, residual hypopigmented macules. Detail of tense blisters.
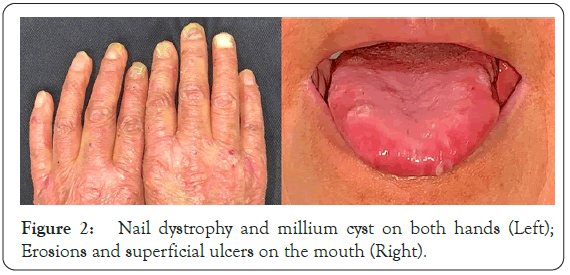
Figure 2: Nail dystrophy and millium cyst on both hands (Left); Erosions and superficial ulcers on the mouth (Right).
We performed a comprehensive metabolic panel that gives values within normal range. Protoporphyrins, antinuclear antibodies were negative and C3 and C4 were not significant. A thorough review of systems was entirely normal. She has negative family history.
A biopsy was taken from the blistering area. Histologically, a unique monocular subepidermal blister with slight content filled with serum and few inflammatory cells was noted. There were no acantholysis. The base of the blister showed the dermal papillae with prominent blood vessel proliferation, fibrosis and moderate lymphocytic inflammatory infiltrate (Figure 3).
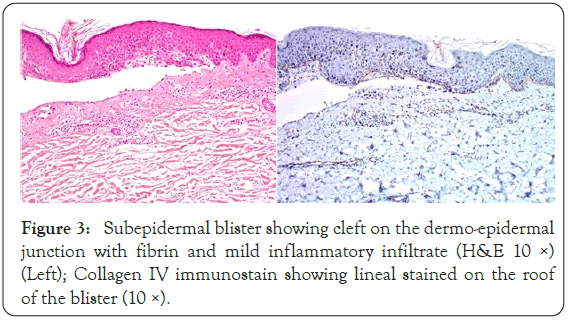
Figure 3: Subepidermal blister showing cleft on the dermo-epidermal junction with fibrin and mild inflammatory infiltrate (H&E 10 ×) (Left); Collagen IV immunostain showing lineal stained on the roof of the blister (10 ×).
We performed immunohistochemical stain for collagen IV which showed predominantly lineal stained on the roof of the blister. These findings supported the diagnosis of EBA (Figure 3).
EBA is a rare autoimmune mucocutaneous blistering disease; that occurs in all ethnic groups, in both genders, at any age with two onset age peaks (the second and seventh decades) [1,3-5]. EBA has been associated with other autoimmune diseases such as Crohn's disease, ulcerative colitis, thyroiditis, psoriasis, rheumatoid arthritis and other blistering diseases.(6) Furthermore, EBA is genetically associated with Human Leukocyte Antigen (HLA), especially HLA-DR2, DRB1*13 in Koreans and DRB1*15 in black patients [1].
Clinically, two major types have been described: the non-classical/ non-mechanobullous/inflammatory like the majority of EBA cases (55%) and the classical/mechanobullous form (38%). Also, the forms with characteristics of both have been reported in the 7% [6]. The mechanobullous type is characterized by subepidermal blisters or erosions on non-inflamed trauma-prone sites, scarring and milium formation, digital contractures and esophageal strictures. The inflammatory EBA includes: Bullous Pemphigoid (BP)-like EBA (tense bullae and erosions on inflamed erythematous or urticarial skin on trauma-prone and non-trauma-prone sites, with or without oral mucosal lesions), Mucous Membrane Pemphigoid (MMP)-like EBA (intact blisters or erosions on mucous membranes, blindness and cicatricial alopecia), Brusting-Perry pemphigoid-like EBA (subepidermal blisters on the head and neck with atrophic scars) and Linear-IgA dermatosis (LAD)-like EBA (erythematous cutaneous arciform lesions and blisters with linear IgA deposits) [1,6].
Histopathology itself doesn´t allow to distinguish EBA from other Subepidermal Autoimmune Blistering Diseases (SAIBDs); and the diagnosis must be established by: serration pattern analysis of linear immunoglobulin deposits in the perilesional biopsy, fluorescent overlay antigen mapping, immunoelectron microscopy and/or detection of circulating antibodies against COL7 [3]. However, these techniques require sophisticated and some have a higher cost laboratory processing and specific equipment [7].
Type IV collagen immunostaining is a simple technique that allow to differentiate EBA from other SAIBDs. The binding of autoantibodies to type VII collagen in EBA, results in the separation of dermal anchoring fibrils from the lamina densa, and type IV collagen is present above blister cavity [2,7-9].
In this case, the clinical diagnosis of inflammatory BP-like EBA, was established by the preponderance of inflammatory blisters eruptions on trauma-prone and non-trauma-prone sites with oral mucosal erosions. In addition, our patient fulfilled the following criteria for EBA diagnosis: (a) a bullous disorder within the defined clinical spectrum; and, (b) histology revealing a subepidermal blister. Finally, (c) the diagnosis was established by the finding of IV collagen immunostaining above blister cavity as a simple, fast, available, and inexpensive diagnostic technique.
All authors, staff and related parties declare that they have no conflict of interest or financing relationships for the preparation of this paper. The main objective of this document is to contribute to medical community sharing an interesting case of Epidermolysis bullosa acquisita presented with impressive clinical lesions.
We also have no financial interest.
Citation: Lafuente L, Urena V, Lascano N, Palacios S (2020) Epidermolysis Bullosa Acquisita: A Case Report. J Clin Exp Dermatol Res. 11:546.
Received: 04-Dec-2020 Accepted: 18-Dec-2020 Published: 25-Dec-2020 , DOI: 10.35248/2155-9554.11.s7.546
Copyright: © 2020 Lafuente L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.