International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2024)Volume 12, Issue 1
Introduction: Lumbar Spinal Stenosis (LSS) and Lumbar Neuroforaminal Stenosis (LNS) are common diagnoses that plague patients with low back pain. Symptoms can also include neurogenic claudication. Costly Magnetic Resonance Imaging (MRI) and Energy Dispersive X-ray (EDX) or electrodiagnostic testing are used as adjuncts to validate diagnosis. However, there are only limited studies discussing the association of these diagnostic tools with radiculopathy. We investigate the association between EDX confirmed radiculopathy and the degree of LSS and LNS found on MRI.
Methods: Retrospective cohort study of patients presenting to an outpatient pain medicine clinic who had a documented EDX and lumbar MRI. The severity of radiographic LSS/LNS was compared to EDX data using a Pearson Chi Square test. The data was fit to a multivariable logistic regression model.
Results: There was not any statistical significance when comparing EDX evidence of radiculopathy and LSS (p=0.50), LSS severity (p=0.54), LNS (p=0.69) or LNS severity (p=0.11).
Conclusion: No significant associations were found between LSS/LNS severity and EDX findings. The presence and degree of severity of LSS/LNS on MRI was not a reliable predictor of EDX findings.
Lumbar spinal stenosis; Neuroforaminal stenosis; EMG; Radiculopathy; Neurogenic claudication; Healthcare costs associated with low back pain
Lumbar Spinal Stenosis (LSS) is a degenerative condition that increases with every decade of life, particularly over the age of 65 [1]. An estimated 85.9 billion dollars in healthcare costs have been associated with back pain annually [2]. The most common treatment modalities for this clinical syndrome include medications, physical therapy and lumbar epidural steroid injections. Failure of conservative treatment is routinely accompanied by further workup with advanced diagnostic modalities such as Magnetic Resonance Imaging (MRI) and Electrodiagnostic (EDX) studies. The future challenge, if costs are to be controlled, appears to lie squarely with prevention and optimum management [2].
Lumbar central canal stenosis is used to describe a clinical syndrome associated with back and leg pain. This pain is made worse with prolonged standing or ambulation. Variable degrees of LSS have been described by neuro radiologists as mild, moderate, and severe. Anatomical narrowing can compress the nerves in the spinal canal and can lead to cauda equina syndrome. Lumbar pain and neurogenic symptoms are frequently relieved with forward flexion [3-5].
The term “LSS” refers to a narrowing of the central spinal canal, whereas Lumbar Neuroforaminal Stenosis (LNS) refers to a narrowing of the neural foramen. Narrowing can be caused by degeneration of the ligamentum flavum, facet joints, or intervertebral discs; all of which can lead to an inflammatory response [5,6].
Imaging such as MRI and Computed Tomography (CT) are utilized as adjuncts for the purpose of visualizing anatomy and pathology in LSS/LNS. These radiographic studies can guide surgical intervention [7]. MRI is the method of choice for assessing the severity of spinal stenosis [7,8]. CT scans may also be helpful for examining bone abnormalities and the degree of stenosis, particularly in patients who cannot undergo MRI due to medical conditions such as having a pacemaker or metal implants in their bodies. Additionally, CT myelogram can be used as another way to assess the potential spinal canal compromise.
When clinical history, physical examination and radiographic findings are numerous, treatment can be challenging [7,8]. Thus, further EDX may be warranted. EDX have been shown to have high specificity for nerve pathology [9,10]. EDX add prognostic value which can in turn lead to better long-term treatment outcomes, especially for patients with lower extremity radicular pain in the presence of lumbar spinal stenosis [11].
The use of EDX for patients with suspected radiculopathy has been well established [12-15]. EDX are indicated in patients with sensorimotor signs and symptoms. These can include pain, paresthesia, weakness, sensory changes, reflex changes and/or atrophy. EDX have shown to be significantly altered in select patients with moderate to severe degrees of central spinal stenosis [14].
MRI and EDX can often be over utilized in the setting of lumbar radicular pain syndromes [16-18]. Previous studies have shown discrepancies between electrodiagnostic testing and MRI results. Notably, differences can exist between structural levels seen on MRI and neurological levels diagnosed on EMG [19]. Ultimately, neurogenic sciatica is a clinical diagnosis.
The aim of this study was to identify if an association exists between EDX and the degree of LSS/LNS on MRI. To our knowledge the degree of neuroforaminal narrowing has not been evaluated with reference to EDX findings.
Patient selection
This retrospective cohort study was granted IRB approval through Wayne State University. 855 potential patients were identified by retrospective chart review. The inclusion criteria began with all patients who had been seen in our outpatient pain medicine practice. We later identified the patients whom had EDX and MRI available for review. Of these, 101 were duplicate patients. Of the remaining 754 unique patients, 126 individuals only had upper extremity EMG/NCS testing results and 455 individuals did not have a lower extremity EMG/NCS available for review. 64 individuals had lower extremity NCS/EMG performed, however, did not have any MRI studies available. The study pool was narrowed down to 109 total patients who had readily available lumbar MRI and complimentary EDX for review. Of the 109 research subjects, only 10 were identified to have EDX evidence of radiculopathy as show in Figure 1. All patients selected were coded de-identified prior to statistical analysis. The EDX was performed within our neurology department and all MRI’s were read by neuro-radiologists at our medical center (Figure 1). 855 total patients were identified based on chart review. 101 of these patients were identified to be duplicate records and were removed from the study, leaving 754 unique patients that were further reviewed. Of the 754 patients, 581 patients did undergo LE EMG at the time of the study, 126 did undergo UE EMG. 173 patients did undergo LE EMG, however, 64 of the 173 patients did not have coinciding Lumbar MRI. This left 109 total subjects that had both MRI of the L-spine and LE EMG. 10 of these patients did have evidence of radiculopathy on EMG testing.
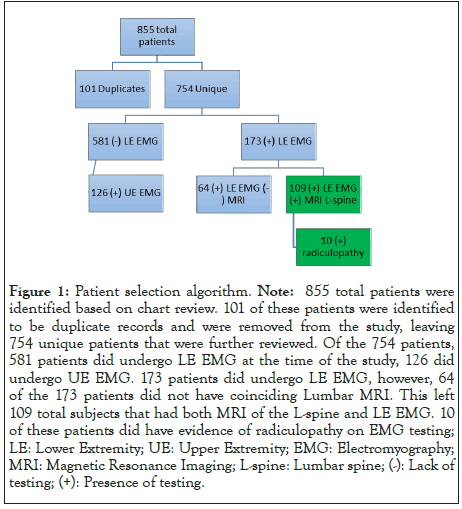
Figure 1: Patient selection algorithm. Note: 855 total patients were identified based on chart review. 101 of these patients were identified to be duplicate records and were removed from the study, leaving 754 unique patients that were further reviewed. Of the 754 patients, 581 patients did undergo LE EMG at the time of the study, 126 did undergo UE EMG. 173 patients did undergo LE EMG, however, 64 of the 173 patients did not have coinciding Lumbar MRI. This left 109 total subjects that had both MRI of the L-spine and LE EMG. 10 of these patients did have evidence of radiculopathy on EMG testing; LE: Lower Extremity; UE: Upper Extremity; EMG: Electromyography; MRI: Magnetic Resonance Imaging; L-spine: Lumbar spine; (-): Lack of testing; (+): Presence of testing.
Data gathering
Two independent PM and R physicians were assigned to gather data in regards to EDX and lumbar MRI results in the 109 research subjects. For the EDX testing, EMG results for the 109 patients were coded as having confirmed radiculopathy or absence of, and then assigned binary values. Routinely in the normal course of practice, images were independently reviewed by a board certified neuro-radiologist to determine presence of and severity of both LSS and LNS. Data was then separated into presence or absence of LSS and presence or absence of LNS based upon the radiologist interpretation. Then these subjects were further stratified into specific groups representing stenosis severity (none=0, mild=1, mild/moderate=2, moderate=3, moderate/severe=4, severe=5). The researcher assigned to the EDX results were blinded to the MRI results and vice versa.
Statistical analysis
We initially chose the chi-square test to examine the statistical association between radiculopathy and LSS, LSS severity, LNS, and LNS severity. Radiculopathy was coded as present or absent as was LSS and LNS. LSS severity and LNS severity was expressed as ordinal scale ranging from 0 to 5. When the chi-square analysis was conducted, we found that the expected frequencies for many of the cells were below 5. Therefore, we analyzed the data using Fisher’s exact test and the Fisher-Freeman-Halton test.
The proportion of patients who had actual presence of radiculopathy on EDX testing was low (10/109, 9.17%). Patients were further characterized and differentiated by degree of LSS or LNS seen on MRI. 42 (38.5%) patients were determined to have some degree of LSS on imaging, while 86 (78.9%) patients were determined to have some degree of LNS on imaging. Within the LSS population, 24 (22.0%) patients had mild (grade 1), 2 (1.8%) patients had mild-moderate (grade 2), 8 (7.3%) patients had moderate (grade 3), no patients had moderate-severe (grade 4), and 8 (7.3%) patients had severe (grade 5) degrees LSS. Within the LNS population, 33 (30.3%) patients had mild (grade 1), 4 (3.7%) patients had mild-moderate (grade 2), 24 (22.0%) patients had moderate (grade 3), 5 (4.6%) patients had moderate-severe (grade 4) and 20 (18.3%) patients had severe (grade 5) degrees of LNS. 67 (61.5%) patients did not have any evidence of LSS on neuroimaging and 23 (21.1%) of the patients did not have any evidence of LNS on neuroimaging (Table 1).
| Severity Grade | LSS | LSS% | LNS | LNS% |
|---|---|---|---|---|
| 0 | 67 | 61.5 | 23 | 21.1 |
| 1 | 24 | 22 | 33 | 30.3 |
| 2 | 2 | 1.8 | 4 | 3.7 |
| 3 | 8 | 7.3 | 24 | 22 |
| 4 | 0 | 0 | 5 | 4.6 |
| 5 | 8 | 7.3 | 20 | 18.3 |
| Total | 42 | 38.5 | 86 | 78.9 |
Note: The 109 selected patients were further characterized based on degree of LSS and LNS. 42 (38.5%) total patients had evidence of LSS on MRI. Of these, 8 patients were characterized as severe (7.3%), 0 patients were moderate/severe, 8 patients were moderate (7.3%), 2 patients were mild/moderate (1.8%), and 24 patients were mild (22.0%) in terms of LSS severity. 86 (78.9%) patients had evidence of LNS on MRI. Of these, 20 patients were characterized as severe (18.3%), 5 patients were moderate/severe (4.6%), 24 patients were moderate (22.0%), 4 patients were mild/moderate (3.7%), and 33 patients were mild (30.3%) in terms of LNS severity. 67 (61.5%) patients had no evidence of LSS on MRI and 23 (21.1%) patients had no evidence of LNS on MRI; Severity Grading 0=None, 1=Mild, 2=Mild/moderate, 3=Moderate, 4=Moderate/severe, 5=Severe. LSS=Lumbar Spinal Stenosis, LNS=Lumbar Neuroforaminal Stenosis.
Table 1: Characterization of Lumbar Stenosis.
Fischer’s exact test of the association between presence or absence of LSS and radiculopathy on EMG was not significant (p=0.50). Individuals were separated based on the severity of LSS (mild, moderate and severe). The Fisher-Freeman-Halton (FFH) test of the association between severity of LSS and radiculopathy on EMG was also not statistically significant (p=0.54). Similarly, there was no statistically significant association between neuroforaminal stenosis and presence or absence of radiculopathy (p=0.69). Individuals were then separated based on the severity of neuroforaminal narrowing to examine possible association with radiculopathy. The FFH test showed no statistically significant association between severity of neuroforaminal narrowing and presence of radiculopathy (p=0.11) (Table 2A).
| Fisher Correlations (P-values) | ||||
| EMG Result | LSS | LSS_sev | LNS | LNS_sev |
| Radiculopathy | 0.5 | 0.54 | 3.69 | 0.11 |
| Interrater Reliability (k-values) | ||||
| Radiculopathy | 0.052 | 0.028 | ||
Note: FFH (Fisher-Freeman-Halton) testing was performed. There were no statistically significant associations between evidence of radiculopathy on EMG and presence of LSS (p=0.50), LSS_sev (p=0.54), LNS (p=0.69) or LNS_sev (p=0.11). There were none to slight associations based on interrater reliability testing between evidence of radiculopathy on EMG and presence of LSS (k=0.052) and LNS (k=0.028); LSS: Lumbar Spinal Stenosis; LNS: Lumbar Neuroforaminal Stenosis; LSS_sev: Lumbar Spinal Stenosis Severity; LNS_sev: Lumbar Neuroforaminal Stenosis Severity.
Table 2A: Summary of correlations.
We examined interrater reliability between our variables. The association between LSS and presence of radiculopathy had zero to slight association (kappa=0.0518). The association between LNS and the presence of radiculopathy also had a zero to slight association as shown in Table 2A (kappa=0.0277).
We then fit a multivariable logistic regression model to examine the set of variables (presence of lumbar stenosis, stenosis severity, presence of neuroforaminal narrowing, and severity of neuro- foraminal narrowing) in predicting radiculopathy. There was no evidence of multicollinearity among the predictor variables: No VIFs exceeded 2.60.
Test indicated no strong indication of model misspecification. However, the overall model was not statistically significant (p=0.76) and none of the individual variables were significant predictors of radiculopathy. The c-statistic for this model was 0.61, which indicates poor model discrimination (Table 2B).
| Mulyivariable Logistic Regression Model | |
| p-value | c-statistic |
| 0.76 | 0.61 |
Note: Variables of LSS, LNS, LSS_sev, LNS_sev was fit to a multivariable logistic regression model to examine potential to predict evidence of radiculopathy on EMG. The model was not statistically significant (p=0.76) and had poor model discrimination (c-statistic=0.61).
Table 2B: Summary of correlations with mulyivariable logistic regression model.
To our knowledge the degree of LSS/LNS and associated findings on EDX has not been evaluated prior to this study. Specifically, no studies we are aware of have assessed neuroforaminal narrowing as we have in our study. The natural history of LSS with moderate symptom levels rarely shows symptom deterioration over a median of 3.3 years [20]. Moreover, it has been found that the probability of spontaneous activity on EDX is also not related to symptom duration [21]. This is unlike the known evolution of findings associated with acute nerve pathology, and emergence of neural changes apparent on EDX 3-6 weeks after insult.
Lumbar pain generalization can have several causes. Standard of care begins with conservative treatment options including nonsteroidal anti-inflammatories, physical therapy, chiropractic care, lifestyle modification and postural changes. Physical examination remains the best clinical indicator of geared diagnostic and treatment strategies.
Our data suggests that EDX may not be helpful in the setting of vague symptoms, especially without clear neurological findings on physical exam. MRI and EDX can place additional burdens on the healthcare system, costs on patients and ultimately may not have clinical significance. Clinically, most patients with LSS/ LNS will improve with conservative treatments including physical therapy, medications NSAIDs and minimally invasive spinal interventions.
There are several limitations to our study. This is real life data, and we believe the information obtained is clinically relevant. Comparisons and statistical analyses were made on qualitative measures that were quantified. Some limitations include that more than one radiologist was responsible for evaluation of the lumbar spine MRI. Associations were quantified based on these values and not more objective EDX parameters or previously established lumbar stenosis grading [12]. This could readily explain why we did not observe positive associations between MRI results and electrodiagnostic evidence for radiculopathy as previously reported [15]. Instead we quantified MRI and EDX in a retrospective fashion.
Other limitations include the lack of inclusion of physical examination findings, duration of symptoms, treatment options completed, or lumbar spine x ray findings. This would be an interesting to perform in the future. One consideration, although controversial (and not offered at our medical center) is to perform more focused electrodiagnostic modalities such as lumbar paraspinal mapping.
Another limitation of the study was our sample size. Although we began with nearly 1000 patients, less than 10% were sampled whom had documented MRI and EDX studies. However this is important in that our practice utilizes diagnostic testing judiciously, and we believe this number (10% of patients sampled with a low back pain diagnosis) are reflective of an appropriate ordering frequency.
Survey data suggests that from 2017 to 2019, 10.8% of adults carried medical debt, including 10.5% of the privately insured, and 9.6% of residents of Medicaid-expansion states, significantly fewer than in non-expansion states [22]. We have noticed an increase in utilization review systems employed by insurance companies and hospital systems.
MRI and EDX are not tolerated by all parties. Between 1% and 15% of all patients who undergo an MR examination suffers from claustrophobia and cannot be imaged, or they require sedation to complete the scan [23]. In terms of patient-centered care, clinicians must also remember that EDX testing is invasive and the risks of adverse events, although relatively low, include pain/ discomfort, infections, bleeding, lymphedema, pneumothorax, and many more [24,25].
EDX studies are routinely performed when there are inconsistent findings on history, physical exam and other diagnostic workup.
However, EDX do not necessarily correlate with severity of LSS/ LNS on MRI of the lumbar spine. Consistent with our hypothesis, no statistically significant associations were found between the severity of LSS/LNS and electro diagnostically confirmed radiculopathy. Furthermore, no significant associations were seen after fitting the data to a multivariable logistic regression model. Finally, the kappa statistic, which examines the agreement between EMG findings and narrowing, was not significant.
Without neurologic symptoms (reflex changes, radicular sensations, weakness, or sensory loss on exam) it is believed MRI and EDX testing can and should be postponed.
No correlation was observed between the degree of LSS/LNS and EDX evidence of radiculopathy. Given the lack of correlation, EDX testing is not indicated prior to trial of more advanced interventions. However, for individuals with failure to improve with expectant management, EMG testing and more detailed anatomical imaging is indicated. Electrodiagnostic studies (evaluation of nerve function) are also used when there are symptoms radiating into the legs. Our study evaluates if there is an association between the degree on narrowing seen on MRI and its association with nerve function results on electrodiagnostic testing.
DHR is the principal investigator, reviewed the draft, provided edits and submitted the paper. AY obtained the references, assembled tables and figures and wrote the initial draft of the paper. DW performed the data mining and insertion/ composition into the excel spreadsheet. BB and AS were involved with revision of the document. M was the statistician involved with interpretation of the data. GKS was actively involved in data review, authorship and finalization of paper.
Data are available on request only due to ethical, legal or commercial reasons.
No funding was necessary for this study.
The authors of this manuscript disclose this was submitted for a poster presentation to AAP conference 2023. No copyrighted sources have been used for publication purposes. Permission is granted to use the figures in this document. No additional disclosures.
Citation: Rustom DH, Yan A, Shah A, Wilcox D, Bradt B, Millis S, et al. (2024) Electrodiagnostic Confirmation of Lumbar Radiculopathy and its Association with Lumbar Central Canal Stenosis and Neuroforaminal Stenosis. Int J Phys Med Rehabil. 12:715.
Received: 10-Jan-2024, Manuscript No. JPMR-24-29125; Editor assigned: 12-Jan-2024, Pre QC No. JPMR-24-29125(PQ); Reviewed: 30-Jan-2024, QC No. JPMR-24-29125; Revised: 07-Feb-2024, Manuscript No. JPMR-24-29125(R); Published: 15-Feb-2024 , DOI: 10.35248/2329-9096.24.12.715
Copyright: © 2024 Rustom DH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.