International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Original Research Article - (2022)Volume 10, Issue 4
Background: Traditional Mirror Therapy (TMT) uses a mirror to reflect the movements of healthy limbs to trick the brain through the visual illusion that the impaired limb is moving as a healthy limb. Virtual Reality (VR) systems present a computer-generated reality to simulate the physical world that a user can interact with via projected images or virtual reality goggles. Virtual Mirror Therapy (VMT), one such application of VR, presents the user with a visual of two limbs moving in a unified mirror motion when in the real world; only the healthy limb is mobile. The effects and impact of TMT and VR systems have been studied previously, but few systems have combined and tested the two methods together in a clinical environment.
Objective: This pilot study aims to evaluate the effectiveness of VMT in comparison with TMT for stroke and braininjured patients to improve impaired upper limb functionality, using clinical assessment tools Chedoke Arm and Hand Assessment Inventory (CAHAI) and Chedoke-McMaster Stroke Assessment (CMSA).
Methods: The design was a clinical pilot Randomized Control Trial (RCT) study with 7 patients (4 subjects TMT, 3 subjects VMT). Each participant received treatment over a 4 to 6-week period. Patients were randomly assigned to receive either TMT or VMT treatment. Clinical assessments were conducted by a blinded assessor at baseline and after 6 weeks of treatment.
Results: Data was compared to determine the effectiveness of VMT vs. TMT in improving upper extremity function in stroke and acquired brain injury patients
Conclusion: Results showed that upper extremity function improved in both VMT and TMT for stroke and acquired brain injury patients. Overall, the results of this pilot RCT showed that the effects of VMT are matched with those of TMT. To determine the full efficacy of virtual mirror therapy a larger scale RCT with more subjects should be conducted to achieve more conclusive results.
Virtual reality; Mirror therapy; Stroke; Acquired brain injury; Upper extremity; Rehabilitation
Unilateral motor impairment is a common sequel of Cerebral Vascular Accidents (CVA) and Acquired Brain Injuries (ABI). Severe motor impairment in these populations is a devastating medical condition with long-lasting effects. These effects include physical and cognitive deficiencies due to damage to the brain's neural systems, with about 55%-75% of individuals failing to regain functional use of their paretic arm and hand after a stroke [1-3] due to neural damage in the brain. In order to minimize the after-effects of stroke and ABI, physical and cognitive therapy is undertaken in both acute and chronic conditions. Physical rehabilitation engages the brain and allows it to reorganize motor neurons, through a process known as neuroplasticity to create new pathways that lead to increased mobility and function [4]. Mirror Therapy (MT) has been shown to reduce the effects of upper limb partial paralysis in patients with hemiplegia [5]. MT involves placing a mirror over the affected limb and angling it. MT uses the mirror to reflect the movement of healthy limbs onto impaired limbs to trick the brain, through visual distortion, into thinking that the impaired (affected) limb is moving like a healthy limb. This creates a visual illusion that moving the unaffected limb also results in movement in the affected limb. The literature indicates that MT is an effective method for improving upper limb function in clinical populations [6-8]. However, MT is not used widely in rehabilitation facilities for upper limb partial paralysis due to a number of limitations such as: (1) the MT activities performed lack functionality and activities of daily living (ADL) tasks (i.e. placing pennies in a jar), (2) the activities are non-immersive and have low patient engagement (3) it is restrictive and has tentative procedures. Murray stated that mirrors limit the workspace to a narrow spatial dimension and force the patient’s body to remain in a fixed position during therapy, with the head oriented towards the mirror during therapy, which can be an uncomfortable pose for ABI users [9].
A recent Cochrane systematic review concluded that further studies should compare mirror therapy with other conventionally applied or newly developed therapies [10,11]. One such newly developed treatment is using a virtual environment for the mirror effect. The potential advantage of Virtual Mirror Therapy (VMT) is that it uses the virtual representation of functional bilateral, symmetrical tasks.
In the last 10 years, Virtual Reality (VR) has become an emerging treatment option [12], and the literature reported efforts in testing the applicability of VR-based devices in neurorehabilitation. A recent review [10] assessed the effects of VR treatment on the recovery of motor, gait, balance, cognitive functions, and activity limitations. Previous VR-based devices have delivered therapy to an upper extremity through different virtual environments, including video game-based tasks, camera-based gesture recognition, and high 3D multimodal VR platforms [13-18]. The images can be delivered either by open (non-immersive) standard computer screens and television monitors or by closed (immersive) Head-Mounted Displays (HMD) and Computer-Assisted Virtual Environment (CAVE) systems. However, only a few of the VR studies have sought to combine VR and mirror therapy. These devices have been developed for pain treatment, with a special focus on treating chronic pain such as phantom limb pain in amputation patients [19-21]. VR system was used in two trials to evaluate the effect and mechanism of upper limb motor function recovery [21,22].
Overall, literature studying the effects of VR based mirror therapy suggests that results of TMT and virtual applications are encouraging, but further research is needed with a specific focus on whether a virtually based mirror therapy device is effective at improving upper extremity function [23]. This paper presents a study of a system that combines immersive VR and mirror therapy to provide training to reduce the effects of upper limb partial paralysis in CVA and ABI patients and improve their functionality. The results and findings of a pilot randomized control clinical trial using the system are presented. This study utilizes the Chedoke Arm and Hand Assessment Inventory (CAHAI) and Chedoke- McMaster Stroke Assessment (CMSA) to evaluate the clinical outcome measures, both of which are standard practices in stroke rehabilitation.
Participants
Eight patients in total were admitted to the study. Subjects were randomly assigned to Traditional Mirror Therapy (TMT) or Virtual Mirror Therapy (VMT). One subject was withdrawn from the VMT study group due to behavioral difficulties, and thus their data was removed. Given the odd number of subjects, the groups are uneven, with one less subject in the VMT group. Subsequently, the results of 7 patients (4 traditional, 3 virtual) are presented. Both study groups received 5 sessions of therapy a week, for 30 minutes per session and for 6 weeks. Demographics for all study participants are shown in Tables 1 and 2. The participants included 2 females and 5 males; with the mean of age was 47 years.
| Patient number | Gender | Age | Weeks Post CVA | Impairment |
|---|---|---|---|---|
| 2 | M | 41 | 101 | 2 |
| 3 | M | 73 | 20 | 2 |
| 5 | M | 82 | 31 | 1 |
| 6 | F | 48 | 19 | 1 |
| Total | 4 | |||
| Max. | 82 | 101 | ||
| Min. | 41 | 19 | ||
| Avg. | 61 | 24.75 |
Note: Impairment: 1=Left body (Right brain); 2 = Right body (Left brain)
Table 1: Demographics of the conventional traditional mirror therapy (TMT) group.
| Patient number | Gender | Age | Weeks Post CVA | Impairment |
|---|---|---|---|---|
| 1 | M | 30 | 50 | 2 |
| 4 | M | 35 | 34 | 1 |
| 7 | F | 20 | 17 | 1 |
| Total | 3 | |||
| Max. | 35 | 50 | ||
| Min. | 20 | 17 | ||
| Avg. | 27.5 | 33.7 |
Note: Impairment: 1=Left body (Right brain); 2=Right body (Left brain)
Table 2: Demographics of the experimental virtual mirror therapy (VMT) group.
Participants were randomized into one of the two groups by the study coordinator using sequentially numbered opaque sealed envelopes pre-populated from a random number table. A research team member from the University of Guelph collected the demographic data from the patients' hospital records. An occupational therapist and physiotherapist blinded to the patient allocation administered the CAHAI-13 and the CMSA at admission and discharge. Patients and their families were provided with the Patient Reported Outcome Measures (PROMS) completed and returned at the first therapy session. The appropriate research ethics boards at the Hamilton Health Sciences, Hamilton, Ontario, Canada and the University of Guelph approved the research project methodology
Inclusion criteria
Individuals interested in participating in the study were admitted based on the following:
1. Radiological evidence of CVA or ABI between 2 weeks to 2 years post-injury.
2. Currently within the in-patient rehabilitation program at Hamilton Health Sciences.
3. No higher than a stage 4 CMSA affected side.
Exclusion criteria
Individuals were excluded from the study if they satisfied one or all the following:
1. Any behavioral impairments that would prevent safe participation are evident (i.e., aggressive behavior).
2. Severe visual impairment preventing the use of virtual reality devices (i.e. blindness, history of vertigo).
3. Severe cognitive deficit resulting in effects on the accuracy of the study.
Clinical outcome measures
Participants were assessed twice, the first upon admission to the study (prior to randomization) and the second after six weeks of intervention. A follow-up at six months' intervention is not feasible for this study because patients are often discharged to areas across the Ontario province. A total of 17 assessments were selected based on current clinical practice (CMSA and CAHAI) and established on the ‘Basic Common Data Elements for Rehabilitation Studies for Moderate-Severe TBI.
The primary outcome measures are CMSA and CAHAI. The CMSA was used to determine the stage of motor recovery and eligibility to participate in the study. The CMSA is a valid and reliable assessment of motor impairment in people with CVA. The CAHAI was used as the primary outcome measure. The reliability and validity of the CAHAI to measure upper extremity function in people with CVA and ABI had been previously established [24-26].
Virtual mirror therapy
A novel virtual mirror therapy system was designed to combine virtual reality and mirror therapy. Physiotherapists, occupational therapists, and neurologists were consulted throughout to help with the overall design and development of the device. The system has three main components: Personal Computer (Intel Core i7- 8700K 6-Core 3.7 GHz), head-mounted display (HMD) (Oculus Rift CV1 (Consumer Version 1) Headset), and two motion capture systems (Microsoft Kinect (for Windows V2), and Leap Motion). The Oculus Rift is an HMD that can present the user with a virtual world while tracking the motion and position of the user’s head. The Microsoft Kinect has a camera and a depth sensor long with built-in software that can track people’s motion and map it to a skeleton on a computer. The Leap Motion consists of two cameras and three infrared LEDs that work in harmony to track a person’s hand and finger movements. Leap Motion Controller was mounted onto the front of the Oculus Rift to track hand motion throughout activities.
Five virtual tasks were designed and developed using Unity Pro to create a 'home environment' where the user can perform a series of everyday activities. The list of developed tasks includes Barbell, Hanging Clothes, Stacking Plates, Rolling Dough, and Clapping Hands. Each activity was designed to mimic activities performed in the real world. Together the five activities (exercise) provide a range of movements seen in everyday life (adduction, abduction, flexion, and extension). Collaboration between the engineering design team and therapists allowed for efficient and meaningful task development and design. To ensure that the tasks incorporated a wide range of motions that would be seen in a typical therapy session. Therapists and physicians were involved in the validation process and approved the final design of each activity. These activities were also designed to best match those in the Traditional Mirror Therapy protocol.
There are three different virtual environments in the VMT system. Activities take place in a gym, kitchen, and backyard setting. The three activities that take place in a kitchen environment are Stacking Plates, Rolling Dough, and Clapping hands. Stacking plates have the participant in a seated position with a stack of red plates in their lap. The participant picks up and places the plates on the shelving unit in front of them. When seated at the kitchen table, participants have a rolling pin in hand and a wad of dough placed on a cutting board. The Clapping Hands exercise presents the patient with a red ball target in front of them in which they reach out and clap either side of the ball. Within the gym environment, participants perform bicep curl exercises with a weighted barbell. Lastly, in the backyard, a stack of clothing appears in the participant's lap, and they place each article of clothing on a clothing line.
Traditional mirror therapy
Traditional Mirror Therapy has been shown as an effective form of therapy for improving upper extremity function. However, TMT is not widely used due to a lack of engagement and practicality. A group of researchers in Germany developed a practice-based protocol for mirror therapy because there was too much variability and inconsistency in how mirror therapy is administered. The protocol provides a framework of activities with room for customization to the patient's specific needs. Additionally, it outlines the required materials, setup, and activities for mirror therapy. The TMT tasks were selected from five main categories of activities: Range of Motion, Strength, Fine Motor, Gross Motor and Coordination.
Experimental procedures
Eight patients were recruited to the study to understand the effects of VMT versus TMT as measured by pre and post-assessment scores over six-weeks. One subject was withdrawn from the VMT study group. Of the seven participants, four received traditional mirror therapy and three received virtual mirror therapy.
Standard rehabilitation practice is to use clinical outcome measures to determine a patient's progress throughout therapy. As mentioned, two clinical outcome measures that are common practice are CMSA and CAHAI.
The VMT system tracked multiple parameters during the therapy sessions (session time, number of pauses, number of breaks and repetitions). However, the highest priority was tracking the number of repetitions completed in each activity. The data was tracked in real-time, and repetition was described as one complete movement of the task. Repetitions were recorded by the VMT system and automatically stored in a database. With TMT, the reps were counted by hand with a manual number clicker and transcribed into a patient's file.
Experimental (virtual mirror therapy) group: Individuals randomized to the experimental group received 30 minutes of supervised therapy five times a week using the VMT system for a total of 6 weeks. This therapy treatment was administered solely by the research student investigator. Patients within this treatment group received usual care from the rehab program. Participants were seated in their wheelchair facing and three meters away from the Kinect. The trunk was not restrained; however, rehabilitation therapists ensured that patients were in a comfortable upright position with no tilt to the wheelchair. The affected arm was positioned in a rest position either on the arm of the wheelchair or propped up with a pillow. The researcher assisted the patient with putting on Oculus goggles, and each patient had their own assigned slipcover for the goggles for sanitation purposes.
During 30 minutes of therapy, patients completed five exercises in the virtual environment. Exercises were queued in random order at the beginning of each session. Therapy sessions consisted of two fifteen-minute sessions back to back where each of the five exercises is completed for three minutes in duration for a total of fifteen minutes for all five exercises. In between sessions, patients were given a break, and the VR headset was removed. Patients were actively encouraged to engage the affected side during tasks and to attempt all tasks twice. This protocol was designed to ensure patients would be actively engaged and allowed for a rest period in between sessions.
Conventional (traditional mirror therapy) group: Similar to the Virtual Mirror Therapy group, individuals who were randomized to the experimental group received 30 minutes of Traditional Mirror Therapy of supervised therapy five times a week. This therapy was administered solely by the rehabilitation occupational therapy assistant. Patients within this treatment group received usual care from the rehab program. Participants were seated in their wheelchairs and wheeled up to an adjustable height table. A large mirror specially built for this project was placed midsagittal in front of the patient with the mirror slightly tilted to block the affected side from view. Before beginning the activity, patients were shown a two rep demonstration of the task. Patients were actively encouraged to watch their performance by looking in the mirror and to engage/stimulate the affected limb during tasks.
Statistical analysis
An independent t-test was conducted on the CMSA and CAHAI outputs from 7 patients. To test the normal distribution of the data, a Shapiro-Wilks test was done. P-values for all VMT treatment groups were p<0.05 and TMT treatment groups were p<0.05 in all assessments except for the CMSA Arm.
Shapiro-Wilks, along with boxplots, show that the data sets have opposite skews and are not normally distributed; therefore, transforming the data is not an option. The homogeneity of variances is met by all data sets for CMSA and the CAHAI. There was homogeneity of variances for assessment scores for VMT and TMT treatment groups, as assessed by Levene's Test for Equality of Variances.
A Wilcoxon statistical analysis was conducted to determine the distribution of the scores for the difference between the two treatment groups and median scores for both groups. The results of this test for the CAHAI, all three CMSA (shoulder, arm and hand) are shown in the Results section.
Statistical analysis-clinical primary outcome measures CMSA and CAHAI
Data of the primary outcome measure of clinical assessments of the upper extremity (CMSA and CAHAI) was compared to determine the effectiveness of the VMT system vs TMT. An independent t-test was used to determine if a statistically significant difference was seen between the change scores for experimental versus conventional treatment. The change score represents the difference between pre and post scores for each clinical outcome measure. For example, Patient 7 was in the VMT group and had a CAHAI pre score of 21 and a post score of 28, therefore the over CAHAI change score was +7. Change scores were calculated for all participants and run through an independent t-test using SPSS Statistics. The output is shown in Table 3 and is the group statistics.
| Treatment | N | Mean | Std. Deviation | Std. error mean | |
|---|---|---|---|---|---|
| CAHAI_Change | TMT | 4 | 7.75 | 10.37224 | 5.18612 |
| VMT | 3 | 4.6667 | 4.04145 | 2.33333 | |
| CMSA_Shld_Change | TMT | 4 | -0.75 | 2.21736 | 1.10868 |
| VMT | 3 | 0.6667 | 0.57735 | 0.33333 | |
| CMSA_Hand_Change | TMT | 4 | 0 | 0.8165 | 0.40825 |
| VMT | 3 | 0.6667 | 0.57735 | 0.33333 | |
| CMSA_ARM_Change | TMT | 4 | -0.25 | 0.5 | 0.25 |
| VMT | 3 | 0 | 0 | 0 | |
Table 3: Statistical output for mean values of each pre and post assessments.
Output for the group statistics, for primary outcome measures CMSA and CAHAI, are listed in Table 3, as shown in CMSA Shld (Sholder) (0.66), CMSA Hand (0.66) and CMSA Arm (0.0) compared to the traditional group (TMT). With the CAHAI change scores, the traditional group (TMT) had a higher mean score (7.75). Also, important to note was that the standard deviation was higher in all four assessments for the traditional group with values of 10.37 (CAHAI), 2.21 (CMSA Shld), 0.81 (CMSA Hand) and 0.5 (CMSA Arm), respectively. Comparatively, virtual standard deviation values were 4.04 (CAHAI), 0.57 (CMSA Shld), 0. 57 (CMSA Hand) and 0.00 (CMSA Arm).
Given such a small sample size, the goal of this experiment was a proof of concept and to show that VMT results and TMT results were no different for CMSA and CAHAI change scores. Based on the literature, it is known that TMT is proven as an effective therapy tool, and we can assume that if no adverse effect and no difference exists between TMT and VMT, then it is possible that Virtual Mirror Therapy is equally as effective as Traditional Mirror Therapy or maybe greater and further investigation is warranted.
Results of the t-test showed that there was no statistically significant difference (p>0.05) in mean CMSA scores and mean CAHAI score between TMT and VMT (CAHAI p=0.652, CMSA Shld p=0.339, CMSA Hand p=0.286, CMSA Arm p=0.437), as in Table 4. P values are displayed in Table 4 in the Sig. (2-tailed) column. In the traditional group, the mean CAHAI change score was 3.08 (95% CI-13.5 to 19.6) higher than VMT mean CAHAI score. Whereas VMT mean CMSA Shld score was 1.41(95%, −4.0 to 2.0), mean CMSA Hand score -0.6 (95%, -2.1 to 0.8), and CMSA Arm score -0.25 (95%, 0.51 to 0.54) were higher than TMT mean CAHAI score. Although the results are encouraging, due to the small sample size, the statistical power of these results is low.
| Treatment | T-test for equality of means | |||
|---|---|---|---|---|
| df | Sig. (2-tailed) | Mean difference | ||
| CAHAI_Change | Equal variances assumed | 5 | 0.652 | 3.08333 |
| Equal variances not assumed | 4.086 | 0.616 | 3.08333 | |
| CMSA_Shld_Change | Equal variances assumed | 5 | 0.339 | -1.41667 |
| Equal variances not assumed | 3.524 | 0.297 | -1.41667 | |
| CMSA_Hand_Change | Equal variances assumed | 5 | 0.286 | -0.66667 |
| Equal variances not assumed | 5 | 0.262 | -0.66667 | |
| CMSA_ARM_Change | Equal variances assumed | 5 | 0.437 | -0.25 |
| Equal variances not assumed | 3 | 0.391 | -0.25 | |
Table 4: Statistical output for ind`ependent T-test for equality of the means.
To better summarize the findings, Table 5 provides an overview of the results. The table shows the mean change scores for each assessment in both treatment groups. The first value presented under each treatment group is the admission score, which reflects the mean admission (pre) score for each of the assessments. These are followed by the mean discharge (post) score. The mean change score is arrived at by subtracting the admission score from the discharge score.
| Patient number | CMSA Arm | CMSA hand | CMSA Shld | CAHAI |
|---|---|---|---|---|
| Traditional Therapy (n=4) | ||||
| Admission | 2.25 | 2.5 | 4 | 15 |
| (Pre) | ||||
| Discharge (Post) | 2 | 2.5 | 3.25 | 22.75 |
| Mean Change | -0.25 | 0 | -0.75 | 7.75 |
| P-Value | 1 | 1 | 0.655 | 0.109 |
| Virtual Reality Mirror Therapy (n=3) | ||||
| Admission | 2.333 | 2.333 | 4 | 2.725 |
| (Pre) | ||||
| Discharge | 2 | 3 | 4.333 | 2.89 |
| (Post) | ||||
| Mean Change | -0.333 | 0.667 | 0.333 | 0.165 |
| P-Value | 1 | -0.6 | -1.4 | 3 |
| Difference in Treatments | -0.3 | -0.6 | -1.41 | 3.08 |
| P-Value | 0.437 | 0.206 | 0.339 | 0.652 |
Note: *positive (+) difference values indicate TMT was greater, negative (-) value indicate VMT was greater.
Table 5: Summary table of Mean Change Scores in pre vs. post assessments for CMSA and CAHAI.
The change scores for each of the patients were analyzed statistically. P-values of 1.0 were found for CMSA Arm and Hand in the TMT group as well as CMSA Arm for the VMT group. A p-value of 1 indicates that the patients had the exact same change score (in this case improvement) in pre-versus post-assessment scores. In all assessment scores, there was no significant difference between the patient change scores (p>0.05). As mentioned previously, the ‘Difference in Treatments’ values indicates which mean change value was greater. In this case, the (-) value indicates that VMT experienced higher means and a (+) value indicates that TMT experienced higher means.
Statistical analysis-secondary outcome measures repetition data
Each patient's results from therapy activities were plotted on a graph of the Number of Repetitions vs. Session Number. A trend line and equation of the line were added to each plot to determine the slope. To further explain the results of the VMT rehabilitation activities, Figures 1 and 2 show the sample of the plots created for the VMT group activities. Due to the limited space, we cannot list all the plots for the 5 VMT different activities and their repetitions for all the 3 patients. Patient 7 was able to complete the Clapping Hand activity in all three levels of difficulty (Easy, Medium, and Hard) and is plotted in Figures 1 and 2 show the Patient 7 plot for the Stacking Plates activity.
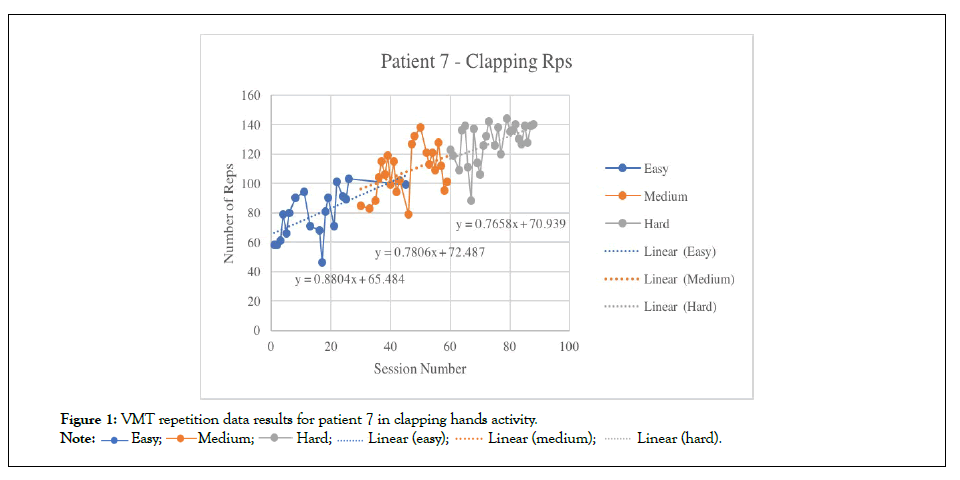
Figure 1: VMT repetition data results for patient 7 in clapping hands activity.

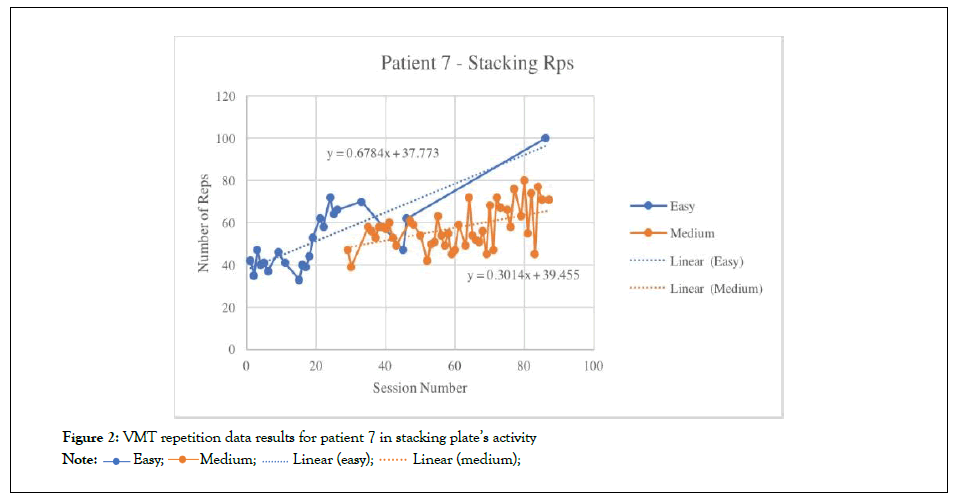
Figure 2: VMT repetition data results for patient 7 in stacking plate’s activity
The trend lines in Figures 1 and 2 shows that the number of repetitions increased as the number of sessions completed increased. Patient 7 started off on the Easy level of difficulty in all activates and was moved up to the level Medium in four activities (Rolling Dough, Stacking Plates, Hanging Clothes and Clapping Hands) and up to the hard level in one activity (Clapping Hands).
Slope values were used to determine the amount of improvement shown by average repetitions for each patient in all levels of activity Table 6, then group average improvements based on activity were determined (Table 7).
| VMT Average Rep Improvement | ||||
|---|---|---|---|---|
| Activity | Difficulty Level | Patient 1 | Patient 4 | Patient 7 |
| Barbell | Easy | 0.883 | 1.612 | 1.002 |
| Medium | 0 | 1.008 | 0.084 | |
| Rolling Dough | Easy | 2.002 | 1.91 | 1.273 |
| Medium | 0 | 2.209 | 0.799 | |
| Stacking Plates | Easy | 1.007 | 0.771 | 0.678 |
| Medium | 0 | -0.378 | 0.301 | |
| Hanging Cloths | Easy | 1.408 | 0.485 | 0.591 |
| Medium | 0 | 0.317 | 0.689 | |
| Clapping Hands | Easy | 0.328 | 2.817 | 0.88 |
| Medium | 0 | 1.321 | 0.781 | |
| Hard | 0 | 0 | 0.713 | |
| Total Average | 0.518 | 1.098 | 0.713 | |
Table 6: Average repetitions values are slope values from the equation of the line for each level of difficulty.
Table 6 shows the average repetition values taken as the slope from the equation of the line for each level. The cumulative average for the slope values is shown in Total Average Improvement values (Patient 1-0.518, Patient 4-1.098, and Patient 7-0.713). Patient 4 showed the greatest improvements (1.098 total average) and saw person highs in Rolling Dough-Easy (1.910) and Clapping Hands- Easy (2.817). Patient 7 saw an average improvement for 0.713 and had person best in Rolling Dough-Easy (1.273) and Barbell-Easy (1.002). Patient 7 increased very minimally (0.084) in Barbell- Medium due to only completing two sessions at this level. Patient 1 saw the lowest average score of improvement within the VMT group (0.518) yet saw the greatest improvement in a single activity with a value of 2.002 in Rolling Dough-Easy.
An analysis of the average activity improvement across the VMT group in Table 7 showed that there was variable improvement depending on the style of activity. Stacking plates produced the lowest value of 0.408 compared to all other activities. Hanging clothes, which has an almost identical movement pattern, produced the second lowest and a similar value of 0.582 for total average improvement. Both hanging clothes and stacking plates were two of four activities where the hard level was never reached. The greatest improvement was seen in the reaching centered activity of Rolling Dough (1.365), which was nearly twice as successful as Clapping Hands (0.766). The Barbell was similar to Clapping Hands, which requires tasks at mid-range with a value of 0.765.
| VMT Average Activity Improvement | ||||
|---|---|---|---|---|
| Activity | Avg. improvement | TOT Avg. Improvement | ||
| Barbell | Easy | Medium | Hard | |
| 1.166 | 0.364 | 0 | 0.765 | |
| Rolling Dough | 1.728 | 1 | 0 | 1.365 |
| Stacking Plates | 0.842 | -0.025 | 0 | 0.408 |
| Hanging Cloths | 0.828 | 0.335 | 0 | 0.582 |
| Clapping Hands | 1.342 | 0.701 | 2.553 | 0.766 |
Table 7: Average activity improvement for VMT group.
Results from TMT Average Rep Improvement are shown in Table 8. The analysis to determine the average repetitions improvement scores was the same as for the VMT group. Results were much lower than those shown in the VMT group, with some showing a decline in the average number of repetitions achieved (Patient 5). Patient 5 saw a decline in average repetitions in 3 activities, which included Strength (-0.006), Gross Motor (-0.010), and Coordination (-0.010). Only a minor increase in the other two activities was seen, Fine motor (0.026) and ROM (0.008). Patients 2 and Patient 6 both displayed increases in three activities ROM (0.570), Fine Motor (0.191) and Coordination (0.200). Patient 3 displayed the most improvement of the TMT group with a total average of (0.192) and personal highs in ROM (0.284) and Strength (0.242). Moderate improvement for Patient 3 was seen in Fine Motor (0.091) and Coordination (0.111) and moderate to high improvement in Gross Motor (0.233).
| TMT average rep improvement | ||||
|---|---|---|---|---|
| Activity | Patient 2 | Patient 3 | Patient 5 | Patient 6 |
| ROM | 0.57 | 0.284 | 0.008 | -0.009 |
| Strength | 0.015 | 0.242 | -0.006 | 0.012 |
| Fine Motor | 0.014 | 0.091 | 0.026 | 0.191 |
| Gross Motor | -0.115 | 0.233 | -0.01 | 0.2 |
| Coordination | -0.198 | 0.111 | -0.01 | 0.2 |
| Total Average | 0.057 | 0.192 | -0.076 | 0.065 |
Table 8: Average repetition improvement score for TMT group.
In contrast, looking at the average improvement within specific activities, Table 9 shows the results of each activity. Improvement gains were most strongly seen in ROM exercises with an average activity improvement of 0.213. A result that is still well below that of the lowest average activity improvement in the VMT group (0.408, Table 7). A negligible increase in Coordination (0.003) and a slight decrease in Gross Motor (-0.048) for the group.
| TMT Average Activity Improvement | |
|---|---|
| Activity | TOT Avg. Improvement |
| ROM | 0.213 |
| Strength | 0.051 |
| Fine Motor | 0.081 |
| Gross Motor | -0.048 |
| Coordination | 0.003 |
Table 9: Average activity improvement for TMT group.
A virtual mirror therapy system for reducing the effects of hemiplegia in ABI patients was developed by integrating motion capture, virtual reality, and mirror phenomenon. In a pilot RCT of inpatient ABI patients, the system achieved full-body tracking and mirroring of the unaffected limb to present the user with a virtual, fully functional upper body. The performance was assessed by clinical outcome measures that are common practice within the inpatient unit. Advancements in the tracking of patient performances were made by the ability to accurately and simultaneously track therapy repetitions.
CMSA and CAHAI Discussion: The clinical assessments, CMSA and CAHAI, with TMT and VMT revealed no significant difference in the improvement of upper extremity functionality. With a sample size of this nature, it is common to experience such results. However, it is encouraging a significant difference did not exist in favour of TMT. VMT system was just as effective in rehabilitating motor function as TMT. These results do allow for short term validation of the study, and further research must be done.
Repetition Results Discussion: A benefit of analyzing repetition in this study is that it is the common therapy performance measure between treatments. VMT repetition data that was tracked in unity and stored in the system database was done so in real-time and TMT rep data was counted with a handheld counter by the OTA/ PTA and recorded on a spreadsheet. Results of the repetition analysis revealed that the TMT improvement scores were lower than those of the VMT group. Human error may be a significant factor in these lower values; however, this is an added benefit of the VMT capabilities and accuracy [27,28].
The repetitions data was analyzed to determine the mean improvement of patients within a treatment group. This method of analysis would allow for qualitative analysis of the growth an individual experienced throughout trials and show whether one group experienced more growth. Furthermore, it can then be extrapolated those patients who experienced improvements in repetitions scores were likely motivated and enjoyed the therapy. Levels of difficulty were not a part of the TMT protocol obtained for this study as the level of difficulty is not administered in a set fashion, for example, adding a heavier weight to an exercise at the discretion of the therapist. As well, there is no distinct increase in difficulty for all tasks in the TMT protocol, which can be attributed to the low average improvement scores.
Impact of the research
Improvement in upper limb impairment in the experimental group could result in a combination of outcomes: (1) improvement in motor function and ability to activate damaged portions of the brain; (2) ability to interact with surrounding; (3) increased tone and strength in the affected side of the body; (4) the challenge of a new form of therapy and increased motivation and participation in therapy tasks. A unique aspect of this study was that there were restrictions placed on admission criteria allowing only for participants with severe hemiplegia. Participants were not typical to those admitted to study of similar research as most rehabilitation centers will not rehab a severely lower stage arm.
This study was a pilot to examine the effectiveness of Virtual Mirror Therapy (VMT) in comparison with the conventional method of Traditional Mirror Therapy (TMT). Overall, the results of this pilot RCT showed that the effects of VMT are matched with those of TMT, which is a clinically proven intervention method for improving upper extremity function. Additionally, there were no negative effects on VMT. VMT showed a similar functional impact on the standard clinical outcome assessments. The VMT approach may be more engaging and follows current motor learning principles of using a high repetition of functional tasks to train recovery. There is a need for further research to consider the potential implications on other clinical populations and more comparative studies (i.e., age matching). To determine the true efficacy of VMT in a clinical setting, a full clinical randomized control trial with a greater number of patients is needed.
The authors would like to sincerely thank all the study participants. We also gratefully acknowledge the financial support from the Natural Sciences and Engineering Research Council of Canada (NSERC) through Discovery Grant No. 401378.
The appropriate research ethics boards at the Hamilton Health Sciences and the University of Guelph approved the research methodology.
The authors declare that they have no conflict of interest.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: MacNeil L, Johnson D, Seth N, Abdullah HA (2022) Efficacy of Virtual Mirror Therapy vs. Traditional Mirror Therapy in Stroke and Acquired Brain Injury Patients. Int J Phys Med Rehabil.10:634.
Received: 13-May-2022, Manuscript No. JPMR-22-17497; Editor assigned: 18-May-2022, Pre QC No. JPMR-22-17497(PQ); Reviewed: 07-Jun-2022, QC No. JPMR-22-17497; Revised: 10-Jun-2022, Manuscript No. JPMR-22-17497(R); Published: 21-Jun-2022 , DOI: 10.35248/2329-9096-22.10.634
Copyright: © 2022 MacNeil L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.