International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2021)Volume 9, Issue 1
Introduction: The ultimate goal of rehabilitation after a limb loss is to gain independence at the highest level with the most efficient gait possible with the use of prosthesis and to return to a high level of social integration. The loss of a lower limb has severe implications for a person’s mobility, and ability to perform activities of daily living. This negatively impacts on their participation and integration into society.
Objective: To investigate the functional and gait parameters improved through flared outsole provided to the trans-tibial prosthetic user.
Results: The mean value of locomotor capabilities index of Group A is 35.73 and in group B the mean of locomotor capabilities index is 42.26. The above result was analysed by using related t test was found to be significant p<0.001, as there is significant difference between the both Group.
Conclusions: Ultimately, though, there is no substitute for firsthand experience with flared outsole alternatives. The time spent in fitting trials and dynamic alignment should be sufficient to rule out particular type of flared outsole that are totally unacceptable to the amputee, and an alternative type of flared outsole can be chosen before delivering the prosthesis. But, it is only after wearing the prosthesis day after day during a full range of activities that the subtle differences become clear to the wearer. Each time the prosthesis is replaced; the amputee and prosthetist should once again discuss the perfectly suitable flared outsole option and jointly determine the best course of action based on real-world experience to date.
Unilateral trans–tibial amputees; Prosthesis; Walking; Stair climbing; Gait parameters; Energy expenditure; Physical effort; Rehabilitation
The ultimate goal of rehabilitation after a limb loss is to gain independence at the highest level with the most efficient gait possible with the use of prosthesis and to return to a high level of social integration [1]. The loss of a lower limb has severe implications for a person’s mobility, and ability to perform activities of daily living. This negatively impacts on their participation and integration into society [2].
Ample of studies have been found on the use of flared outsole in orthotic purposes to provide stability to an unstable foot or ankle [3] and to resist inversion or eversion. This design acts as an outrigger, adding to the medial-lateral stability of the shoe and the foot [4].
The modification consists of a strip of firm material added to the medial and lateral side of the shoe and provides a wider base of support for the foot [5]. The lateral flare might be added only to the heel area or it could include the entire side of the shoe, providing a greater surface area for ground contact and will help the foot to feel more stable [6]. The orthotic flare on the lateral aspect of the heel has been investigated during running conditions on controlling: maximum pronation and total rear foot movement [7].
Proprioceptive Neuromuscular Facilitation (PNF)
Proprioceptive Neuromuscular Facilitation (PNF) is a stretching technique utilized to improve muscle elasticity and has been shown to have a positive effect on active and passive range of motions [8]. Studies have shown that this kind of training based on PNF stretching has become more effective than the traditional pre-prosthetic training program in improving ambulatory function [9].
Single-limb balance over the prosthetic limb while advancing the sound limb should be practiced in a controlled manner so that when required to do so in a dynamic situation such as walking, this skill can be employed with relatively little difficulty [10].
The stool-stepping exercise is an excellent method by which this skill may be learned [11]. Have the amputee stand in the parallel bars with the sound limb in front of a 10- to 20-cm (4- to 8-in) stool (or block), its height depending on the patients level of ability. Then ask the amputee to step slowly onto the stool with the sound limb while using bilateral upper-limb support on the parallel bars. The orthotic purpose of the flare is used to provide stability to an unstable foot or ankle and to resist inversion or eversion. This design acts as an outrigger, adding to the medial-lateral stability of the shoe and the foot (Figure 1).

Figure 1: Shoes with flared outsole.
A crucial element of constructing a rehabilitation programme is sound gait analysis. This will largely be observational. Gait analysis consists of observation of the gait, which should occur from all angles. Knowledge of normal gait patterns for the prosthetic and non-prosthetic user is required to help analysis of movement. On observation of the gait the assessor compares the function of the amputee to expected patterns of gait and look for deviations [12]. Analysis of the gait pattern will help determine why these deviations are occurring. This will then help to formulate the rehabilitation programme, which includes correction of the deviations. Outcomes measures can be used to monitor progress [13,14].
Although many studies have been conducted specifically examining the efficacy of Proprioceptive neuromuscular facilitation techniques used in transtibial amputees for improving the functional and gait parameters, no study have been made on the use of flared outsole in transtibial prosthetic users to improve their static and dynamic stability.
However, based on the literature, if Single limb stance (SLS) can be improved in an amputee, then the static as well as dynamic stability will be improved automatically. As such, no standard modification has been suggested to widen the base of support that satisfies the need of static and dynamic stability of an amputee. This study will be designed to measure the effects on gait parameters and functional outcome of with or without flared outer sole provided in trans-tibial prosthesis.
Aim
To investigate the functional and gait parameters improved through flared outsole provided to the trans-tibial prosthetic user.
Objectives
To find out the efficacy of flared outsole in trans-tibial prosthetic users while improving stability i.e. Single limb stance, which ultimately improves the functional outcome as well as gait parameters.
Hypothesis
There is a relation between the use of flared outsole on gait parameters and functional outcome in Trans-tibial prosthesis users.
Null hypothesis
There is no relation between the use of flared outsole on gait parameters and functional outcome in Trans-tibial prosthesis users.
Significance of study
The study is going to present a better rationale for the prescription of appropriate shoe modification required to provide static and dynamic stability in trans-tibial amputees.
Study area: Department of Prosthetics and Orthotics, Pt. Deendayal Upadhyaya National Institute for the Persons with Physical Disabilities (Divyangjan), New Delhi.
Study duration: 1 year (May 2018–April 2019)
Sample size: 30 Subjects (23 Male and 7 Female)
Study design: Two group post-test experimental study design
Inclusion and exclusion criteria
Inclusion criteria:
• Both Male and Female
• Age range: 25-50 yrs.
• Only unilateral trans-tibial amputees are considered.
• Stump length: 1/3rd to 2/3rd of tibial length
• Full ROM of Hip and knee joints and strength not less than 4 in MMT.
• No contracture in the knee and hip joints.
• No sign of phantom pain and phantom sensation.
• Able to understand the command.
Exclusion criteria:
• Bilateral trans-tibial amputee
• No other associated Neurological or Orthopaedical condition.
• Complicated stump (pain, wound, neuroma etc)
• Patient with inadequate Range of motion
• Patient with inadequate muscle strength.
Outcome measures
Gait parameters: Stride length, Step length, and Cadence and Velocity Locomotor capabilities index.
Protocol of the study
A random sample of 30 subjects with unilateral transtibial amputees fulfilling inclusion criteria took part in this study. They were advised to walk in level ground surface. All efforts were made to maintain the environmental conditions same throughout the study. No data was taken in rainy or extreme hot and humid environmental conditions. The patients were normal psychologically with no anxiety, stress, fear etc. They were taught to walk with their own self-selected walking speed.
Study procedure
The individuals with unilateral transtibial amputee reporting to OPD were first screened through the inclusion and exclusion criteria. The individual fulfilling the criteria were included in the study. The individual were explained the study procedure. The informed consents were obtained from the individual or their parents prior to the study participation (Figure 2).
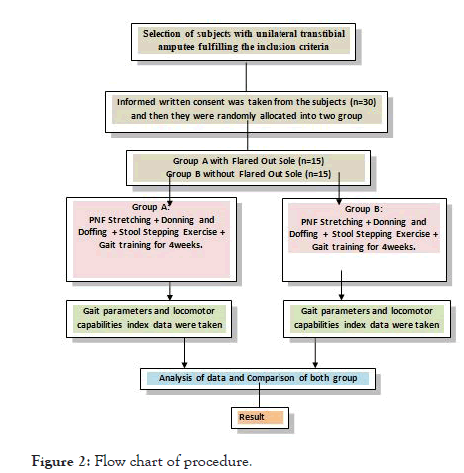
Figure 2: Flow chart of procedure
Firstly, the participants were assessed and evaluated. The demographic data like age, gender, body weight, height were taken. The patients were divided in group A included those fitted with trans-tibial prosthesis with flared outsole and group B included those fitted with trans-tibial prosthesis without flared outsole. Prosthesis were fabricated and fitted for all the amputees. After the fitment of prosthesis, PNF stretching, Stepping Stool exercise, donning and doffing of prosthesis and gait training were given for 4 weeks. After 4 weeks of all these training and exercises, gait parameters and locomotor capabilities index were recorded for both Group A and Group B amputees fitted with trans-tibial prosthesis with flared outsole and without flared outsole respectively. Finally, theses collected data were compared between two groups.
Before going for data collection procedure, all the participants have undergone through PNF stretching technique and Stepping stool exercises as described below:
Data collection procedure
After these exercises, every participant has undergone training for Donning and Doffing and then Gait training. This process was compulsory for all the participants for a period of 4 weeks.
Then every participant was taken for the study and made him/ her to walk on a level ground surface. Foot prints were taken using the method described by Wilkinson and Menz. Their shoes with or without flared outsole were dampened and coated with talcum powder or ink immediately before walking on a strip of brown paper.
The participants were instructed to walk along a smooth horizontal 10 m long walkway at a comfortable speed. Only the middle portion of the walk covered within 20 seconds was evaluated to avoid the variable steps associated with initiation and termination of gait. The same action was repeated for 10 times and the mean from this result was calculated for the distance covered within 20 second. The walking velocity (cm/s) was obtained after dividing the recorded distance by the ambulation time (20 secs).
Further Step length, stride length, cadence were measured for quantitative gait analysis. The step length (cm) was measured from the geometrical heel center of the current footprint to the same of the previous footprint on the opposite foot and stride length (cm) from the line of progression between the heel points up to consecutive foot prints of the same foot. The cadence was calculated by asking the subject to walk for 1 minute through a straight pathway with self-selected speed, then calculating the number of steps taken during 1 minute. This distance was independent of 10 meter walkway. Each participant was given one prior walking before final assessment to become familiarized with walking condition. Footprint method was used for measuring the spatial gait parameters. Participants were asked to walk after applying blue ink on their outsole to get the footprint demonstrated in (Figure 3).
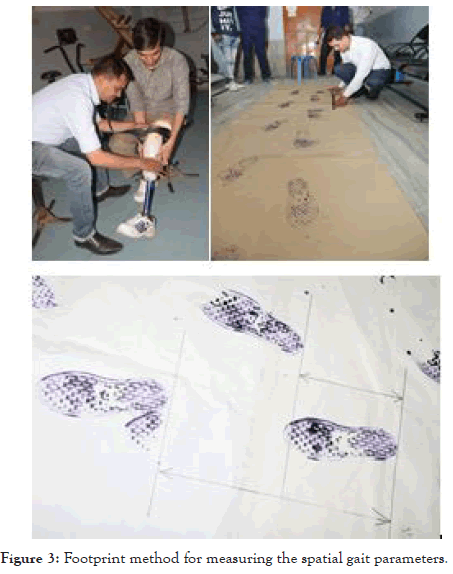
Figure 3: Footprint method for measuring the spatial gait parameters.
Statistical analysis
• Data was managed on an Excel spread sheet.
• SPSS statistical software version 16 was used for data analysis.
• Statistically the results were analysed using the t-test. Independent t-test was used to compare the gait parameters obtained from both the groups A with flared outsole and Group B without flared outsole.
• The significance level of p<0.05 was fixed
A total number of 30 participants (30 Transtibial amputee) were recruited for the study with age range from 25 to 50 years. There were 23 male and 7 female patients in the study. 15 participants with flared outsole were included in Group A whereas another 15 participants without flared outsole included in Group B. There was no drop out during the study. Data were collected after completion of post prosthetic gait training for 4 weeks.
The result of the study showed that there is an increase in velocity, step length, stride length and cadence with flared outsole group than without flared outsole group. When comparing velocity in both the groups 5.87% increment found in with flared outsole (3.07+0.19) than in without flared outsole (2.9+0.20). This improvement is statistically significant (p=0.025). In cadence the improvement in with flared outsole is 1.43% higher than without flared outsole. The percentage improvement is negligible but it shows statistically significant result (p=0.01). When step lengths of both the group are compared 10.5% improvement found in with flared outsole (0.62+0.015) than without flared outsole (0.561+0.017) having p=0.039. With flared outsole (1.24+0.030) and without flared outsole (1.12+0.034) when compared for stride length 10.7% improvement found in with flared outsole than without flared outsole (p=0.001). From the above data it reveals that the mean value of with flared outsole shows better result than the without flared outsole group (Tables 1-3).
| SL. NO. | Baseline characteristics | Group A | Group B |
|---|---|---|---|
| 1 | No of Subjects | 15 | 15 |
| 2 | Age range(years) | 25-50 | 25-50 |
| 3 | Mean age(SD) | 39.13(7.1) | 39.33(7.3) |
| 4 | Sex(Male/Female) | 11/4 | 10/5 |
Table 1: Pedigree on code 71 and code 93 C. arabica Ruiru 11.
| Velocity km/hr | Mean ± SD | t value | p value |
|---|---|---|---|
| Group A | 3.07 ± 0.19 | 2.13 | 0.025 |
| Group B | 2.91 ± 0.23 |
NOTE: The mean velocity of Group A is 3.07 and in Group B the mean velocity is 2.91. The result was analysed by using related t-test was found to be significant p<0.025, as there is significant difference between the both Group.
Table 2A: Comparison of velocity for both Group A and Group B.
| Cadence (Step/min) |
Mean ± SD | t value | p value |
|---|---|---|---|
| Group A | 82.26 ± 4.71 | 1.753 | 0.01 |
| Group B | 81.05 ± 4.17 |
NOTE: Table 2B shows the mean cadence of Group A is 82.2 and in group B the mean cadence is 81.05. The result was analysed by using related t-test was found to be significant p<0.01, as there is significant difference between the both Group.
Table 2B: Comparison of Cadence for both Group A and Group B.
| Step Length (m/sec) |
Mean ± SD | t value | p value |
|---|---|---|---|
| Group A | 0.62±0.015 | 2.62 | 0.027 |
| Group B | 0.56±0.017 |
NOTE: Table 2C shows the mean step length of Group A is 0.62 and in group B the mean step length is 0.56. The result was analysed by using related t-test was found to be significant p<0.027, as there is significant difference between the both Group.
Table 2C: Comparison of step length for both Group A and Group B.
| Stride Length (m/sec) |
Mean ± SD | t value | p value |
|---|---|---|---|
| Group A | 1.24 ± 0.03 | 2.89 | 0.039 |
| Group B | 1.12 ± 0.034 | ||
NOTE: Table 2D shows the mean stride length of Group A is 1.24 and in group B the mean stride length is 1.12. The result was analysed by using related t-test was found to be significant p<0.039, as there is significant difference between the both Group.
Table 2D: Comparison of stride length for both Group A and Group B.
| LCI | Mean ± SD | t value | p value |
|---|---|---|---|
| Group A | 35.73 ± 4.1 | 4.08 | 0.001 |
| Group B | 42.26 ± 2.9 |
NOTE: Table 3A shows the mean value of locomotor capabilities index of Group A is 35.73 and in group B the mean of locomotor capabilities index is 42.26. The above result was analysed by using related t test was found to be significant p<0.001, as there is significant difference between the both Group.
Table 3: Comparison of Locomotor capabilities index for both Group A and Group B.
This might have happened due to the Enhanced base of support and cosmesis of the prostheses had a positive effect on prosthetic function and the participant’s satisfaction. Our study showed improved in velocity, cadence, and step length, stride length in with flared outsole than without flared outsole. This result is also supported from the study by Majumdar et al. who concluded that gait speed has a significant impact on the temporal and spatial gait parameters. The stride parameters changed in an increasing or decreasing order with the different walking velocity. The ground reaction forces in loading and push off is augmented from slower to higher walking speed. The minimum value of PCI indicated that better gait efficiency is achieved at higher walking speed during initial period of walking.
These results accords with those of literature led by Majumdar et al. He made a study on transtibial amputee on gait cycle and stated that the gait cycle duration decreased with speed increment. The ground reaction force patterns were moreover similar in different walking speeds however there was a significant difference in the force amplitude and rate of increment with slower to higher speed. Significant changes in gait parameters showed that amputee’s gait is not normalized in various walking speeds.
The locomotor capabilities of index of without flared outsole shows the greater value than that of with flared outsole group. The mean value of without flared outsole group in LCI is (42.26+2.96) and in with flared outsole group the mean value of LCI is (35.73+4.11). The without flared outsole group shows 18.27% more improvement than with flared outsole group. The above data reveals that the result of this study might be due to acceptance of broadened base of support system by the participants. This literature also supported by the literature of Baars et al. They emphasized on the enhanced base of support and cosmesis of the prostheses had a positive effect on prosthetic function and the participant’s satisfaction their study showed improved stance and dynamic stability with the use of flared outsole.
The result of the present study support the hypothesis and shows statistically significant difference between the Trans-tibial prosthesis with flared outsole and without flared outsole group. Thus, with flared outsole is better option for amputee patient than without flared outsole.
Patients will decide about flared outsole based on familiarity and loyalty to the first prosthesis fitted. Patients display a definite tendency to opt for with flared outsole. The choice will also depend upon whether the lifestyle is more active than sedentary and upon hearsay and myths which circulate in sporting groups. On the whole, most young people are best fitted with a prosthesis with flared outsole. It is easy to don and doff, and provides good stance and dynamic stability. It is almost impossible for someone to fall off the ground with the prosthesis used with flared outsole against the wishes of the wearer because of increased base of support.
The challenge for the prosthetist is to evaluate the relative advantages and limitations of various kinds of flared outsole and to recommend those that will prove most satisfactory for each individual in the long run. The more clearly the amputee’s personal goals and preferences are understood, the more likely it will be that the type of flared outsole selected will be successful.
Ultimately, though, there is no substitute for firsthand experience with flared outsole alternatives. The time spent in fitting trials and dynamic alignment should be sufficient to rule out particular type of flared outsole that are totally unacceptable to the amputee, and an alternative type of flared outsole can be chosen before delivering the prosthesis. But, it is only after wearing the prosthesis day after day during a full range of activities that the subtle differences become clear to the wearer. Each time the prosthesis is replaced; the amputee and prosthetist should once again discuss the perfectly suitable flared outsole option and jointly determine the best course of action based on real-world experience to date.
Citation: Sahoo MR, Behera TP, Suresh AMR, Jayavant S (2020) Efficacy of Flared out Sole in Functional and Gait Parameters in Trans-Tibial Prosthetic User. Int J Phys Med Rehabil. 9:585.
Received: 30-Nov-2020 Accepted: 15-Dec-2020 Published: 22-Dec-2020 , DOI: 10.35248/2329-9096.21.9.585
Copyright: ©2020 Sahoo MR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.