
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2021)Volume 12, Issue 10
Background: The aim is to compare the use of adenosine and verapamil for management of postoperative supraventricular tachycardia in terms of time of conversion of SVT to normal sinus rhythm, success rate, hospital stay length and adverse events
Methods: Patients (54–65 years old) received adenosine or verapamil groups. In the adenosine group, patients received IV adenosine 6 mg bolus then wait 2 minutes, if it failed another 12 mg IV of adenosine was administered. In the verapamil group, patients received IV verapamil 5 mg bolus slowly over 2 minutes followed by a second IV bolus of 10 mg, 30 minutes after the initial dose in persistent Supra Ventricular Tachycardia (SVT). If SVT persisted, the patient was shifted to adenosine.
Results: Patients were followed up regarding the efficacy of drug; blood pressure, mean time of conversion of SVT (time elapsed from effective dose of the study drug till conversion of SVT to sinus rhythm) and incidence of adverse events were recorded. The efficacy of adenosine was significantly higher than verapamil (P<0.001). The time of conversion of SVT to sinus rhythm was significantly shorter in adenosine group compared with verapamil group (P<0.001). The incidence of hypotension was comparable between the study groups. The mean arterial blood pressure and the incidence of complications were comparable.
Conclusion: Intravenous administration of adenosine effectively treat SVT in terms of higher efficacy and shorter time of conversion of SVT to normal sinus rhythm compared with verapamil without any significant difference regarding the incidence of side effects between the study groups.
Trial registration: This study was approved by Medical ethics committee of Ain Shams University approval number FMASU R 62/2019) and the protocol was prospectively registered at ClinicalTrials.gov: NCT 04203368 on December 16, 2019.
Adenosine; Verapamil; CABG; Adult; Postoperative
Arrhythmias commonly occur after cardiac surgery; supraventricular tachycardia occurs briefly after CABG [1]. They represent the main cause of morbidities such as thromboembolic complications, heart failure, increase hospital stay length and cost and may progress to ventricular arrhythmia despite improvements in anaesthetic and surgical techniques [1]. Post-Operative Arrhythmias (POAs) include Atrial Tachyarrhythmia (ATs) and to a lesser extent Ventricular Arrhythmias (VAs) [1].
Postoperative tachyarrhythmia is caused by Inflammation and hyper adrenergic state provoked by cardiac surgery in addition to atrial enlargement as well as trauma from cannulation [2]. Hypokalaemia and hypomagnesemia alter phase III of the membrane action potential, slowing the conduction speed and increasing the automaticity [2]. The extended use of Holter and growing age of the patient population and interruption of coronary blood flow lead to bigger incidence of SVT nowadays [2].
Cardiac surgery initiates a severe inflammatory response due to a variety of metabolic, immune changes and endocrine response known as the “stress response,” which has important clinical consequences [3]. Surgical trauma, blood transfusion, hypothermia, and cardiopulmonary bypass activate the inflammatory response especially surgical trauma [4,5]. These effects lead to a trial and ventricular arrhythmias in the early postoperative period.
The term paroxysmal tachyarrhythmia needs atrial or AV nodal tissue, or both, for their initiation and maintenance [6]. It is characterized by its sudden onset and includes AV re-entrant tachycardia AV nodal re-entrant tachycardia and atrial tachycardia. Tachyarrhythmias are more likely to be supraventricular than ventricular [7].
Patients with supraventricular suffering from hypotension, chest pain and severe anxiety, must be assessed if they are hemodynamically stable or not. Serious hemodynamic instability occurs in a minority of patients and immediate electrical cardioversion is required [8]. The criteria of instability include angina, systolic blood pressure less than 90 mmHg, signs of cardiac failure or confusion. Carotid sinus massage used as the first line of treatment and when fails, pharmacological therapy is required. The most commonly used drugs are verapamil and adenosine. They are both effective with different efficacy. Both have adverse events as hypotension, breathlessness and dizziness [9]. The aim of pharmacological treatment is to slow or block atrial-ventricular nodal conduction; however, there is still r some controversy regarding the effectiveness of verapamil and adenosine for the treatment of postoperative supraventricular tachycardia [10]. Adenosine is safe, promising and rapidly acting for management of supraventricular tachycardia through interruption of AV nodal re- entry pathway [11]. Verapamil reduces the frequency of sinus node firing and decreases AV node conduction and keeps the normal function of His-Purkinje fibres so it is used to terminate atrial arrhythmia [12].
The aim of this prospective randomized study to compare the use of adenosine and verapamil for management of postoperative supraventricular tachycardia in terms of time of conversion of SVT into normal sinus rhythm, efficacy and adverse events in elderly patients undergoing Coronary Artery Bypass Grafting (CABG).
Methodology
The institutional ethics committee approved the study (approval number FMASU R 62/2019). Clinical trial.gov. Number NCT04203368; Written informed consent was obtained from every patient for performing surgery. This prospective randomized parallel-group clinical trial was conducted in 268 adult patients aged 54–65 years with American Society of Anesthesiologists (ASA) physical status II and III, scheduled for elective isolated CABG from February 2020 till November 2020 who experienced SVT after CABG. The following inclusion criteria happened on the first postoperative day: (1) sinus rhythm more than 150 beats/min (2) systolic blood pressure >110 mmHg without inotropic support except dopamine less than 3 micrograms/kg/min (3) normal electrolytes level and volume status at the time of the attempts (4) patients received beta-blockers pre-postoperatively. Patient with impaired cerebral Perfusion, wide QRS complexes, ejection fraction less than 4%, allergy to adenosine or verapamil and patients with Wolff Parkinson White syndrome, preoperative atrial fibrillations or flutter, patients on antiarrhythmic drugs or digoxin and renal failure or patients diagnosed with hypo/hyper thyroidism were excluded. A detailed medical history, including medications used and full investigations including thyroid function test, electrolytes, coronary angiography and arterial blood gases were assessed on the night of the surgical procedure.
Anesthesia management was standardized to minimize any effect of anesthetic type on hemodynamics. Premedication with midazolam was limited to a maximum of 0.05 mg/kg. Anesthesia was induced with intravenous fentanyl, propofol, and rocuronium for muscle relaxation followed by endotracheal intubation and was maintained with 1%–2.0% isoflurane. Heart rate and blood pressure were maintained within 20% of the baseline values. After separation from CPB, heparin was neutralized with protamine sulfate and 1 mg/100 U heparin to reach an activated clotting time within 10% of baseline. All patients were transferred to the ICU after surgery.
Upon arrival at the ICU, a standardized protocol for postoperative care was implemented for all patients by welltrained nurses supervised 1:1 and by the ICU consultants and patients were continuously monitored with 12-lead Electrocardiogram in addition to invasive blood pressure and pulse oximetry.
Treatment regimen
Patients suffering from postoperative SVT (narrow QRS and regular rhythm) who were diagnosed by consultant of ICU then confirmed by cardiologist randomly allocated into 2 study groups, adenosine group and verapamil group. The patients were randomized using a computer-generated random number in various block sizes in 1:1 ratio. Randomization was done using the SAS statistical package version 9.3 (SAS institute, Cary, NC, USA) by a statistician who was not involved in the study.
In the adenosine group, patients received IV adenosine 6 mg bolus over 1-3 seconds followed by rapid saline flush then wait 2 minutes, if it failed to return to sinus rhythm then another 12 mg IV bolus of adenosine was administered and it can be repeated once more 5 minutes after the first dose. Patients were converted to verapamil 5 mg or 10 mg in case of recurrence of SVT. In verapamil group, patients received IV verapamil 5 mg bolus slowly over 2 minutes followed by a second IV bolus dose of 10 mg in case of persistence of Supra Ventricular Tachycardia (SVT) 5 minutes after first bolus dose. Patients were shifted to adenosine 6 mg or 12 mg in case of failure of verapamil to control SVT. The patients’ systolic blood pressure, heart rate and oxygen saturation were closely monitored during ICU stay. In case of hemodynamic instability, patients were treated by synchronized electrical cardioversion. If the rhythm did not convert to sinus rhythm after maximum dose of adenosine or verapamil, as in cases of atrial flutter or junctional tachycardia, it can be treated by cardiologists with intravenous beta-blockers or diltiazem.
All patients were routinely extubated when deemed clinically appropriate according to the local ICU protocol, by ICU staff, when the patient was able to maintain spontaneous breathing for 48 h, according to normal weaning parameters, after which they were encouraged to sit on a chair and mobilize with the assistance of health care providers in the ICU then the physiotherapist became responsible for improving mobility and rehabilitation of the patients till discharge from the hospital. On the ward, patients received 12-lead ECG recording every other day and were followed up by an expert cardiologist till discharge from hospital. After home discharge, patients experiencing postoperative SVT should receive follow up with a cardiologist for electrophysiological test and to treat the recurrence of SVT which is usually treated by oral verapamil 80-120 mg TID.
Primary outcomes
The primary outcome of the study was the efficacy of the study drug which included the conversion to normal sinus rhythm.
Secondary outcomes
The secondary outcomes included, mean arterial blood pressure, mean time of conversion of SVT to sinus rhythm (time elapsed from effective dose of the study drug till termination of SVT), rate of recurrence of SVT within 2 hours of treatment drug administration and the incidence of adverse events including hypotension, flushing, dyspnea, dizziness, premature ventricular complexes and bradycardia. The end-point is drug withdrawal as a result of serious drug toxicity or need for surgical re-exploration.
Sample size
Using Power Calculations and Sample Size software (PASS; NCSS, LLC, East Kaysville, UT, USA) revealed that 268 patients, 134 per arm, was required after considering a 5% drop out (power of 80%; alpha error at 5%). These calculations were based on a previous study that showed that the efficacy was 91% in verapamil group and 79% in adenosine group [11].
Statistical analysis
Data were analyzed using SPSS Statistics version 23 (IBM© Corp., Armonk, NY, USA). Normally distributed numerical data were presented as mean and SD, and skewed data were presented as median and interquartile range. Qualitative data were presented as number and percentage or ratio. Normally distributed numerical data were compared using the unpaired ttest. Skewed numerical data were compared using the Mann– Whitney test and categorical data were compared using Fisher’s exact test. P-value <0.05 were considered statistically significant.
This study was performed at Ain Shams University hospital (Cardiothoracic Academy) from February until November 2020. A total of 268 patients were enrolled in the study with no single case of protocol violation as shown in CONSORT flow diagram (Figure 1).
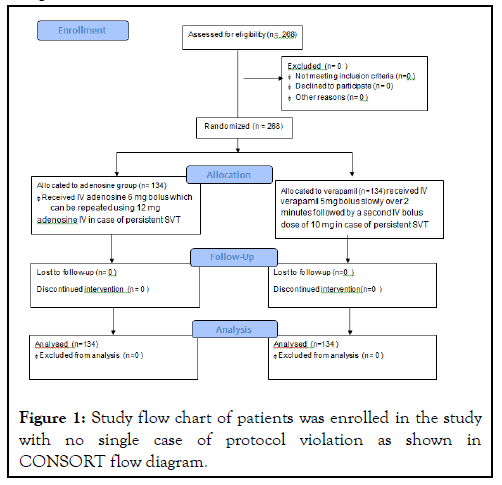
Figure 1: Study flow chart of patients was enrolled in the study with no single case of protocol violation as shown in CONSORT flow diagram.
The demographic and surgical data in addition to comorbidities were comparable between the study groups (Table 1).
| Adenosine group N=134 |
Verapamil group N=134 |
P value | |
|---|---|---|---|
| Age | 60.14 ± 3.01 | 59.6 ± 2.89 | 0.156 |
| Sex | |||
| Male | 98(73.13%) | 95(70.90%) | 0.683 |
| Female | 36(26.87%) | 39(29.10) | |
| ASA | |||
| ASA II | 74(55.22%) | 76(56.72%) | 0.806 |
| ASA III | 60(44.78%) | 58(43.28%) | |
| Cross clamp time | 67.06 ± 11.44 | 65.54 ± 12.63 | 0.304 |
| Bypass time | 150.11 ± 1.38 | 147.29 ± 1.34 | <0.001 |
| COPD | 29(21.64%) | 32(23.88%) | 0.799 |
| Hypertension | 47(35.07%) | 49(36.57%) | |
| Diabetes mellitus | 27(20.15%) | 25(18.66%) | 0.757 |
| Number of grafts | |||
| 2 grafts | 24(17.91%) | 25(18.66%) | 0.966 |
| 3 grafts | 60(44.78%) | 61(45.52%) | |
| 4 grafts | 50(37.31%) | 48(35.82%) | |
| LV EF% | 51.94±0.70 | 52.08 ± 1.26 | 0.255 |
Table 1: Demographic and surgical data, LV EF: Left Ventricular Ejection Fraction, COPD: Chronic Obstructive Lung Disease. All data were presented as percentage except age, bypass time, LV EF% and cross clamp time were presented as Mean ± SD.
The analysis of the primary outcome revealed that the efficacy of adenosine (128 (95.5%)) was significantly higher than verapamil (109 (81%) (P<0.001) (Table 2).
| Drugs | Dose | Successful cardio version | Unsuccessful cardio version | 95% CI | efficacy | p-value |
|---|---|---|---|---|---|---|
| Adenosine | 6 mg | 111 (82.8%) | 23 (17%) | 0.606-4.787 | 128 (95.5%) | <0.001 |
| 18 mg | 17 (12.6%) | 6 (4.4%) | ||||
| verapamil | 5 mg | 82 (61.2%) | 52 (38.8%) | 0.766-2.784 | 109 (81%) |
|
| 10 mg | 27 (20.1%) | 25 (18.6%) |
Table 2: Efficacy of the study drugs (comparison between study groups).
Adenosine equal to 6 mg caused conversion in 111 patients while the remaining 23 patients, 17 patients required another dose of 12 mg adenosine to return to sinus rhythm. 4 patients converted with 10 mg verapamil while 2 patients required direct cardioversion (Table 2). Verapamil equal to 5 mg caused conversion in 82 patients while the remaining patients 52 patients, 27 patients required another dose of 10 mg verapamil to return to sinus rhythm. 15 patients converted with 6 mg adenosine while 7 patients required 12 mg adenosine and finally, 3 patients received direct current cardioversion (Table 2).
The incidence of hypotension was similar in verapamil group and adenosine group (P<0.082) (Table 3). There was no significant difference between the study groups as regard the incidence of bradycardia and dyspnea (P=0.652, P=1.00 respectively) (Table 3).
The mean time of conversion of SVT to sinus rhythm was significantly shorter in adenosine group compared with verapamil group (P<0.001). The mean arterial blood pressure was comparable in adenosine group compared with verapamil group (P=0.108). The incidence of facial flushing and vomiting were comparable between the study groups (P=0.156, P=0.562 respectively) (Table 3).
| Adenosine group N=134 |
Verapamil group N=134 |
95% CI | P-value | |
|---|---|---|---|---|
| Hypotension | 0(0.00%) | 3(2.24%) | 0.027-2.22 | 0.082 |
| Bradycardia | 2(1.49%) | 3(2.24%) | 0.108-4.024 | 0.652 |
| Dyspnea | 1(0.75%) | 1(0.75%) | 0.061-16.15 | 1.000 |
| Mean time of conversion to sinus rhythm from effective dose(minutes) | 8.51 ± 1.01 | 13.44 ± 1.54 | - 5.25/-4.62 | <0.001 |
| Dizziness | 1(0.7%) | 2(1.5%) | 0.044-5.539 | 0.562 |
| Mean arterial B.P (mmHg) | 84.38 ± 1.36 | 84.63 ± 1.13 | -2.11/ -1.65 | 0.108 |
| Facial flushing | 2(1.49%) | 0(0.00%) | 0.180-22.49 | 0.156 |
| vomiting | 1(0.75%) | 2(1.49%) | 0.248-9.194 | 0.562 |
Table 3: Secondary outcomes (comparison between study groups) B.P: Blood Pressure all data were presented as percentage except were presented as ventilation time, mean time of conversion to sinus rhythm from effective dose and mean arterial B.P presented as mean ± SD.
Verapamil and adenosine have been firmly used as a safe and effective treatment for supraventricular tachycardia which frequently occurs after CABG [10].
This prospective study was the first to discuss the efficacy and safety of adenosine and favored its use in termination of SVT in adults undergoing CABG surgery. It revealed that bolus intravenous adenosine use was associated with higher efficacy of conversion of SVT to normal sinus rhythm in terms of termination of SVT by the study drug. Mean time of termination of SVT was significantly shorter in adenosine group compared with verapamil group. The mean blood pressure and the incidence of adverse events were comparable between the study groups in patients undergoing CABG.
After review of literature, a previous study comparing bolus intravenous verapamil with bolus intravenous adenosine administration for management of SVT to normal sinus rhythm had confirmed similar efficacy of verapamil and adenosine with success rate 73% to 89% and 59% to 100% respectively [13]. This is different from the results of the current study.
A study by Cheng and his colleagues stated that the efficacy of intravenous boluses of verapamil and adenosine were similar where drug efficacies were 87% and 86% respectively. The findings of the current study showed that bolus intravenous adenosine use was associated with higher efficacy of conversion of SVT to normal sinus rhythm [14].
In contrast to the findings of the current study, a meta-analysis by Delaney et al. showed that Verapamil and adenosine efficacy were comparable in treating PSVT, but they still cause minor side effects such as higher incidence of hypotension for verapamil and higher incidence of minor adverse effects as dizziness and facial flushing for adenosine [10].
An earlier study by Rankin and his colleagues concluded that preliminary treatment of PSVT with adenosine was associated with efficacy 93.5%-100% while in verapamil, the success rate ranged from 81% to 95% [15]. Also, verapamil intravenous administration was associated with more significant side effects than adenosine [15]. These findings support the results of the present study.
A review by Smith comparing adenosine and verapamil administration for termination of SVT demonstrated that verapamil was more significantly effective for management of SVT than adenosine [16]. Although, verapamil administration was associated with higher incidence and duration of side effects [16].
A study by Shaker et al. comparing the use of adenosine with adenosine-verapamil for treatment of SVT stated that only 2 patients of adenosine group out of 92 randomized patients experienced facial flushing and one patient experienced decreased systolic blood pressure [12]. In this study, 2 patients of adenosine group experienced facial flushing but none of patients of adenosine group experienced hypotension.
A study by Ballo and his colleagues showed that intravenous administration of adenosine 6 mg effectively converted SVT to normal sinus rhythm within 1-2 minutes in 60% of the patients and in 92% of the patients after a bolus dose of 12 mg [17]. In this study, conversion of SVT to normal sinus rhythm after a bolus dose of 6 mg of adenosine in 83% of the patients and 12% of patients after another dose of 12 mg adenosine.
Adenosine is an endogenous purine nucleoside, its time of termination of supraventricular tacharrythmias is about 10-15 seconds. Its mechanism of action is mediated through interruption of the AV nodal re-entry pathway and is used as first-line medication in treatment of SVT [18].
An earlier study by Sethi et al. who compared the efficacy of adenosine versus verapamil for the control of paroxysmal supraventricular tachycardia and they found that the efficacy of adenosine (89%) was significantly better than verapamil (61%; p<0.05) [19]. The time of termination of SVT in Adenosine group was significantly shorter compared with verapamil group (24 seconds, 142 seconds respectively; p<0.01) [19]. These results agreed with the findings of the current study.
On the contrary of results of the current study as regard the efficacy, a previous study Lim et al. compared the efficacy of IV calcium channel blockers versus adenosine IV bolus [20]. They reported that a significantly higher efficacy in the calcium channel blocker group (98%) compared with the adenosine group (86.5%). However, patients receiving calcium channel blockers experienced greater incidence of hypotension (blood pressure decrease more than 20% of the baseline value) compared to the adenosine group where 1% of patients had hypotension [20].
This study was subjected to few limitations: The treatment drugs were not blinded which open a way for bias. Limited number of studies comparing the efficacy of both drugs in termination of SVT in adults undergoing cardiac surgery which makes it challenging to identify the preferred pharmacological therapy of this common arrhythmia occurring after cardiac surgery. Also, the sample size was modest, thus necessitating more clinical trials with a larger number of patients to confirm the results of the present study. Finally, other calcium channel blockers such as diltiazem were not studied to confirm their role in management of SVT.
Intravenous administration of adenosine effectively treated SVT in terms of higher efficacy and shorter time of termination of SVT compared with verapamil, and it was associated with minimal adverse effects similar to verapamil in adult patients undergoing CABG.
The data sets used during the current study are available from the corresponding author on reasonable request.
Citation: Shokri H, Ali I (2021) Efficacy of Adenosine vs. Verapamil For Management of Supraventricular Tachycardia Post-Coronary Artery Bypass Grafting: A Randomized Trial. J Anesth Clin Res. 12: 1036.
Received: 08-Nov-2021 Accepted: 23-Nov-2021 Published: 30-Nov-2021 , DOI: 10.35248/2155-6148.21.12.1036
Copyright: © 2021 Shokri H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.