Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research Article - (2023)Volume 13, Issue 4
Background: Listening therapy addresses auditory processing challenges and difficulties associated with Autism Spectrum Disorder (ASD) and aims to improve social function and behavioural problems by providing filtered sound in people with ASD. However, contradictory findings have been reported on its efficacy in children with ASD.
Methods: This pilot study assessed the 1-week and 3-month outcome of Safe and Sound Protocol (SSP) on core deficits of autism, including social communication and Restricted, Repetitive Behaviours (RRB) and interests; receptive language; and sensory processing in 24 children with ASD aged 44-119 months.
Results: A statistically significant reduction was observed in the total score of Social Responsiveness Scale-2 (SRS-2) with additional improvement in one of the subdomains (RRB and interests) and in one of the quadrants of Sensory Profile (SP) (low registration and sensory avoidance) and auditory category of SP at 1 week after the intervention compared to baseline. However, all of these gains were not maintained at 3 months after the intervention compared to the baseline. This indicates that the effect of the intervention diminished overtime. Additional analysis indicated that children aged<6 years with mild autistic symptoms and higher language development may respond favourably to this intervention.
Conclusion: Mixed results were obtained in this pilot study on SSP’s effects and feasibility in children with ASD. Further research of higher quality is needed to determine its efficacy and establish if SSP can be a potential treatment option for symptoms associated with autism.
Listening therapy; Autism Spectrum Disorder (ASD); Safe and Sound Protocol (SSP); Social Responsiveness Scale-second edition (SRS-2); Restricted, Repetitive Behaviours (RRB)
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder defined across two core symptoms including impairments in social interaction and communication and restricted interests and repetitive behaviours [1]. Although ASD is known for its complex and multifactorial etiology, at least in part, dysregulation of the Autonomic Nervous System (ANS) contributes to the core features of ASD [2]. Heart Rate Variability (HRV) is the most commonly used non-invasive method of analyzing the ANS. Respiratory Sinus Arrhythmia (RSA), defined as high-frequency HRV at the rate of respiration, indexes Parasympathetic Nervous System (PNS) influences. The empirical findings supported that higher amplitude baseline RSA was associated with higher cognitive abilities [3], appropriate emotion regulation [4], fewer externalizing [5], and internalizing problems; moreover, it was associated with its positive association with better social engagement [6]. Given that the majority of studies have demonstrated lower levels of RSA in children with ASD and its association with higher levels of autistic symptoms, an approach that appeals to ANS function might be required as a treatment option for children with ASD.
The auditory integration-based intervention that uses specially recorded music or environmental sounds, which systematically produce or enhance positive emotional and calming reactions when listened to, has been collectively referred to as sound therapy or listening therapy [7]. Listening therapy is one of the few therapeutic strategies that aim to improve autistic symptoms and other difficulties in children with ASD by approaching the ANS. Unclear evidence exists on its efficacy in children with ASD mainly due to the lack of studies targeting this population. In this study, we examine the potential efficacy and feasibility of Safe and Sound Protocol (SSP), one of the listening therapies, which is designed based on the polyvagal theory on core symptoms and difficulties in children with ASD. To begin with, we discuss the accumulated evidence of atypical ANS in children with ASD. Next, we introduce the theoretical background of listening therapy and its summary of evidence as treatments for children with ASD. Finally, the characteristics of the SSP as well as the aim of our study are described.
Research on autonomic function in children with ASD
A considerable number of studies investigated the atypical ANS in resting-state and ANS regulation in individuals with ASD [2,8,9]. The literature on ANS in individuals with ASD contains confounding results because of inconsistent measures and methodology across studies. Hence, efforts are necessary to synchronize these studies and to synthesize the existing findings. One systematic review comparing ANS of children with ASD and those with typical development revealed that while autonomic differences during resting parasympathetic activity have not been observed between the two groups, there were different patterns of responses to a variety of tasks in children with ASD [10]. Another review suggested that the evidence for autonomic dysfunction in autism is inconsistent with the between-group findings of hyper arousal, hypo arousal, or null effects across different age groups [11]. Based on this result, other authors proposed reduced parasympathetic activation as a trans-diagnostic factor that relates to socialization and communication skills in individuals in internalizing or externalizing disorders rather than specific index for autism [11]. These studies indicated the complex nature of autonomic response in ASD, presence of subgroups in autonomic responders, and deficits of ANS regulation to external stimuli in autism. In addition, they have provided essential lessons when conducting interventions on children with ASD, as these may result in a variety of responses, an implication that highlights the importance of exploring the factors that affect the responsivity. Furthermore, Arora, et al. [11] paid attention to the evidence of different trajectories of RSA in autism that suggests that early differences in the development of ANS in toddlerhood in interaction with the environment might lead to later differences in autonomic arousal and responsivity to the environment. Considering this preliminary result and the findings that children with ASD have a variety of psychiatric complications [12], the need for psychophysiology interventions that may improve the autonomic activity in children with ASD seems to be justified.
Research on listening therapy with ASD
Abnormal responses to sensory stimuli, such as covering the ears, are common characteristics encountered in children with ASD. The discovery of the association between an abnormal reaction to certain frequencies of sound and behaviour and learning problems enhanced the application of listening therapy in children with complex communication needs and behaviour problems [13]. Lucker and Doman [7] gave a clear explanation for the mechanism of auditory hypersensitivity, suggesting that it is largely an emotion-based (limbic system) response to sound, and not an auditory system response to sound. In this mechanism, a non-classical auditory pathway, which branches off from the classical pathway at the level of the lateral lemniscus and projects to emotional centres of the brain, including the amygdala, plays a major role. Thus, it may induce an excessive behavioural response to the sound. The focus of the treatment should be placed on theorized reprogramming of auditory pathways to associate the negative sounds with some behaviour that would lead to a more calming response. The most common form of listening therapy involves listening to electronically-modified music of various lengths and sound frequencies [14]. The aim is to reduce the child’s hypersensitivity, and thus, expect to desensitize the limbic system and retrain the auditory responding system [7].
To date, a selective review of listening therapy studies in patients with ASD have demonstrated no evidence on increasing social communication skills in people with autism or on language acquisition [14]. It is worth mentioning that no meta-analysis has been performed to synthesize the existing data due to the limitations incurred by the different outcome measures used by such studies. However, the authors of these contributions targeted people of different ages from preschool to adults, and it was pointed out that the results might be masked by fewer gains in a generally older sample [14]. As for listening therapy limited to children with ASD, only a few comprehensive investigations have been conducted [15]. Limited information is available on whether listening therapy is effective for children as well as on the characteristics of children who could benefit from this intervention.
Safe and sound protocol
Among the major listening therapies for ASD including auditory listening therapy, a SSP designed based on polyvagal therapy to improve sensorimotor functioning in ASD is gaining attention. It stands out in its enhancement on the sense of safety, security, and social engagement of the user. According to the polyvagal theory, circuits that include special visceral efferent pathways, originating in brainstem nuclei, and exiting five cranial nerves, regulate the striated muscles of the face and head [16] and form the neural substrate of the social engagement system in collaboration with the myelinated vagal efferent pathway to the sinoatrial node [17,18]. Although this social engagement system is blunted in autism, due to the integrated nature of the system, it is hypothesized that the entire integrated social engagement system can be “rehabilitated” via an intervention designed to exercise a specific portal based on this theory [19]. High-frequency sounds associated with the human voice attenuate low-frequency background sounds with phylogenetic transition from reptiles to mammals [20] through a neural system that regulates the middle ear muscles. The dysfunction of this system and difficulty in extracting human voice from background sounds have been observed in individuals with ASD [21]. SSP provides the range of the speed frequencies that corresponds to a calm human voice. As the middle ear muscles (i.e., stapidius, tensor tympani) are trained through this process, the ability of users to extract the human voice and remove low-frequency background sounds would have expected to be improved [19]. Resultantly, individuals are better able to reach a calmed emotional and physiological state and engage in social interaction. Porges, et al. [19] preliminarily assessed the effects in participants with ASD (n=33), following a predecessor of SSP named the Listening Project Protocol. They found that the intervention resulted in positive effects with improvements in both RSA and auditory processing performance, and normalized the RSA reactivity [19]. The results supported the speculation that, due to common brainstem regulatory mechanisms, exercising the middle ear muscles to change the transfer function of the middle ear would improve the vagal regulation of the heart as well as the auditory processing performance.
Two Randomized Controlled Trial (RCTs) that examined the use of SSP in children with ASD demonstrated substantial parent- rated improvement in auditory hypersensitivity, spontaneous speech, listening, and behavioural problems of children with ASD compared to control patients [22]. Although the results of the study revealed the promising effect of SSP on children with ASD, it is still unclear whether SSP can improve core deficits of ASD, including social interaction and RRB, sensory processing difficulty, and receptive language. Motivated by the limited evidence and knowledge about the efficacy of SSP, the major aim of this pilot study was to contribute to the study of SSP intervention in children with ASD.
The first goal of our study was to determine if SSP could provide a therapy option for children with ASD. In this scope, our working questions were as follows: 1) To assess improvement in social interaction; 2) to reduce restricted repetitive behaviours; 3) to assess if gains were made in receptive language; and 4) to assess if sensory processing impairment including auditory processing difficulty were observed. Our second aim was to identify possible predictors of response to SSP. We hypothesized that greater improvement would be expected in younger children (<6 years old) as developmental plasticity is widely considered to be more prominent in early life stages. On the contrary, the effects of interventions turned out to be modest in lower- functioning individuals with severe autistic symptoms who are supposed to have a larger region of abnormality in the limbic system [23]. Finally, greater improvement would be expected in children with severe auditory processing difficulty, according to the RCT trial conducted by Porges, et al. [22]. In accordance with the abovementioned hypotheses, our research questions were as follows: If there may be established different responses in relation to 1) age (less than or greater than 6-years-old); 2) language development (average receptive language or low receptive language); 3) severity of autism (diagnosis of ASD or diagnosis of autism); and 4) level of difficulty in auditory domain (typical, probable difference, definite difference). Moreover, it is expected that a variety of responses to SSP in children with ASD can serve as a clinical reference for improving core deficits and difficulties associated with ASD and provide an implication for understanding the pathophysiology underpinning ASD.
The study was conducted between April 2020 and August 2021 at the Division of Early Childhood Mental Health, National Centre for Child Health and Development in Tokyo, Japan. Ethical approval for this study was obtained from the Ethics Committee of the National Institute for Child and Health Development (No.2020-078). Prior to the study, the parents of the involved children were informed about the procedure and their written consents have been obtained in accordance with the Declaration of Helsinki.
Participants
The participants were recruited via the outpatient department of Division of Early Childhood Mental Health, National Centre for Child Health and Development. According to the purpose of research, we targeted children of a wide range of ages, from preschool to elementary school. To be included in the study, participants had to be between 3 and 12 years of age at the moment of selection and diagnosed with ASD based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria [1], corroborated with Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) form [24] and Autism Diagnostic Interview-Revised (ADI-R) form [25-27]. All diagnostic assessments were conducted or observed by trained, research-certified clinical psychiatrists. The following exclusion criteria were applied: (1) Neurodevelopmental disorder of known etiology (e.g., fragile X syndrome); (2) serious neurological or physical condition; (3) history of epilepsy; (4) significant sensory or motor impairment; and (5) major physical problems, such as a chronic serious health condition. Patients receiving medication were not excluded; however, we did exclude patients whose drug dosage and type were changed during the intervention. Background information and medical history were collected both via face-to-face interviews and from medical records to confirm that all the participants met the inclusion and exclusion criteria. The intervention was planned to be discontinued if significant self-harm or violence or a significant sleep disorder would be noted.
Data collection
Data were collected at the following three time-points which are before the intervention (T0), 1 week after the intervention (T1), and 3 months after the intervention (T2). The primary assessment concerns the changes between T0 and T2 scores. The score changes of T0-T1 and T1-T2 were also assessed as an adjunct assessment to see the temporal effects of the intervention. The primary outcome measure is the association between social impairment and ASD, as measured by the Social Responsiveness Scale™-Second Edition (SRS-2). The second outcome measure regards the receptive vocabulary understanding and sensory processing difficulty, as measured by the Picture Vocabulary Test- Revised (PVT-R) and Sensory Profile (SP), respectively. SRS-2 and SP were measured at T0, T1, and T2, and PVT-R was measured at T0 and T2. All of these scales were completed by the parents.
Primary outcome
The SRS-2 is a standardized measure used to identify social impairment associated with ASD that quantifies its severity across cultures [28,29]. It includes a parent-reported 65-item questionnaire using a 4-point Likert scale ranging from “almost never” to “almost always,” in which each item with a higher score indicated greater impairment. Moreover, it comprises five subdomains that correspond to the two-factor structure of diagnosis, based on DSM-5: Social communication and interaction (social awareness, social cognition, social communication, and social motivation subdomains) and Restricted, Repetitive Behaviours (RRB) and interests [30]. Our analysis included the raw scores of total scores and five subdomains.
The SRS-2 school-age form was used for 21 children aged above 4 years and the SRS-2 preschool-age form was used for 3 children aged 3 years. Japanese Version of the SRS-2 school-age form has been shown to have strong internal consistency (α =0.95) and concurrent validity with the ADI-R (0.66) in mixed clinical (ASD) and nonclinical samples [31]. The Japanese Version of the SRS-2 preschool-age form has been shown to have strong internal consistency (α=0.93) and concurrent validity with the ADI-R (0.74) in clinical (ASD) samples [31].
Secondary outcomes
Sensory profile: SP is a standardized parent-reported questionnaire that was developed as an instrument to assess behavioural responses to various sensory experiences in everyday life for children aged 3-10 years [32]. It contains 125 items using a 5-point Likert scale ranging from “almost never” to “almost always,” in which a higher score indicated greater impairment. The 125 questions were divided into 14 sections and separated into the following three major domains: Sensory processing, modulation, and behavioural and emotional responses. Sensory processing consists of six categories, namely auditory, visual, vestibular, touch, multisensory, and oral sensory. SP also defines the four response patterns (called quadrants) by the intersection of the neurological threshold and self-regulation as follows: Low registration, sensation seeking, sensory sensitivity, and sensation avoiding. The sections and the quadrants are also classified into three categories with referencing the mean score of the typical sample: Typical >1 SD), probable difference (>1 SD), and definite difference (>2 SD). In this study, we focused on the auditory of the sensory processing and the four quadrants scores. In the Japanese version of the SP form, mild internal consistency reliability in the auditory section (α=0.79-0.84) and moderate internal consistency reliability in the quadrants (α=0.78-0.92) were reported [33]. The criterion-related validity of the SP was supported by its moderate to strong correlations with the subscale of “hypersensitivity and difficulty” in the parent-interview ASD rating scale as well [33].
Picture Vocabulary Test-Revised (PVT-R)
PVT-R is the Japanese version of the Picture Vocabulary Test- Revised (PVT-R), which is used to evaluate the listening and understanding of single-word Japanese vocabulary for individuals aged 3 years to 12 years and 3 months [34]. The age-adjusted Scaled Score (SS) was used as a standardized index. High internal consistency reliability of the PVT-R has been reported (α=0.90-0.92), and concurrent validity with the Illinois test of psycholinguistic abilities has also been reported (0.73-0.92) [34].
Intervention program and instrument
The SSP program is designed to provide altered vocal music, the sound of which mimics the prosodic features of a mother’s calming voice, which is intended to induce the user’s bodily states of safety and improve their social engagement. The treatment period went on for 5 consecutive days with 1-hour session per day. The vocal music was stored on an iPod and was delivered via headphones. The MP3 ear-cup type headphones were equipped with a special filter, and the vocal music was computer processed based on a proprietary algorithm, so that the program provided only sounds with frequencies corresponding to 500-3000 Hz, the low and high frequencies being removed. Maximum loudness was calibrated at a peak of 75 dB.
Testing environment
The intervention program was based on the principles of the SSP. The first author completed an SSP training including 5 h of online video training and testing, obtained an SSP certification, and provided the necessary instructions to all parents. Before starting the program at their home, parents were taught how to operate the instruments and verified for proper use face-toface with the provider. The specific instructions provided to the parents are as follows: Create a comfortable and calm space to relax and keep video games and television away, where they feel safe to maximize the SSP effectiveness. Refrain from listening to music while children are sleeping, eating, or exercising. A 1-hour session consists of two 30-minute parts and you should make them finish listening to both parts on the same day. If children need to take a break, pause the music for some time, and then make them listen to the rest of the music. Music should be listened to in the order of the program. The sessions were conducted in the houses of each participant to see how this intervention is adapted in their daily life. Parents were asked to keep records of the daily time spent by their child in session.
Statistical analysis
To address the primary question, pairwise t-analysis tests were performed for each continuous variable of the primary and the second outcome at T0 and T2, T0 and T1, and T1 and T2 to examine the children’s changes after the intervention. As children aged 3 years and above 4 years were assessed with different versions of SRS-2, analyses were performed separately; data for the three children aged 3 years were considered as a supplemental analysis.
The second research question required different datasets. Twenty-one children were divided into two groups according to the diagnosis classified by ADOS-2-Autism, ASD, age: Older than 6 years (≥ 6), younger than 6 years (<6); receptive language estimated by receptive language with referencing PVT-R: Low (PVT-R SS <-1 SD); High (PVT-R SS ≥ -1 SD); the level of auditory processing difficulty measured by SP in auditory category: Typical (1 SD ≥); probable difference (1 SD<); and definite difference (2 SD<). Using this dataset, we conducted a pairwise t-analysis with the T0 and T2 scores, T0 and T1 scores, and T1 and T2 scores of the total score of SRS-2 within each group, independently. When the significant difference in the total score of SRS-2 in a specific group was detected, a pairwise t-analysis was added for five subdomains. We used the Easy R (EZR) program of software version 18.0 for analysis [35], and the statistically significant difference was set to <0.05.
Twenty-nine children with autism between the age of 44 and 119 months were enrolled in this study. The participants were all Japanese. Among the 29 children that met the eligibility criteria, 1 dropped out due to difficulty in wearing headphones and 4 due to medication modification during research periods. Altogether, 24 of the 29 children (91.04%) completed the SSP training. Of these 24 children, 3 were 3 years old and 21 were 4 years old or older. No serious adverse events were observed during or after the intervention.
Results of the 21 children above 4 years
The mean age of the children over 4 years was 83.80 months (SD=18.32) (range=58-119 months) and three (14.2%) of them were female. The mean total listening time of the 21 children was 237.08 minutes (SD=63.66).The mean Autism Diagnostic Observation Schedule-2 (ADOS-2) total and comparison scores were 18.28 (SD=8.16) and 7.47 (SD=2.61), respectively (Table 1). At T0, 13 children received a diagnosis of autism, while 8 were diagnosed with ASD by the ADOS-2 criteria (Table 1 and Figure 1).
| ADOS-2a | Overall (n=24) | Autism (n=21) | Autism spectrum (n=10) | |||
|---|---|---|---|---|---|---|
| Mean | SDb | Mean | SDb | Mean | SDb | |
| Total score | 17.79 | 8.05 | 24.28 | 2.96 | 9.35 | 0.81 |
| Comparison score | 7.25 | 2.58 | 8.7 | 1.26 | 4.3 | 0.45 |
| Note: aADOS-2: Autism Diagnostic Observation Schedule-Second Edition; bSD: Standard Deviation. | ||||||
Table 1: Accompanying models of support.
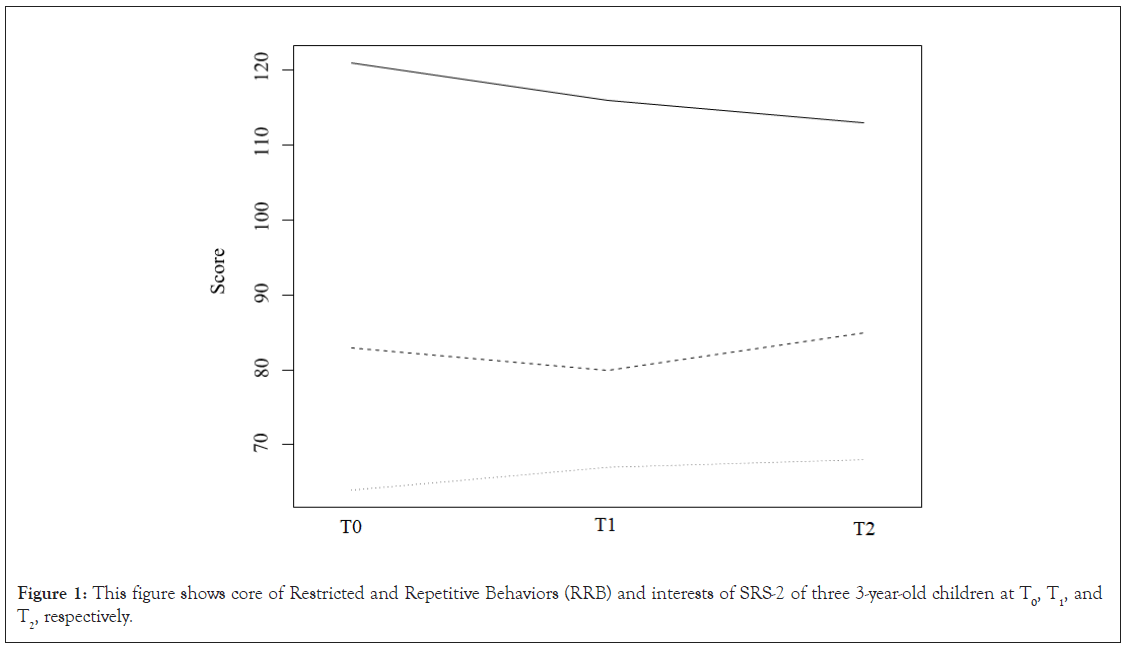
Figure 1: This figure shows core of Restricted and Repetitive Behaviors (RRB) and interests of SRS-2 of three 3-year-old children at T0, T1, and T2, respectively.
The analysis of SRS-2 total score is described in Table 2. A significant reduction on the total score of SRS-2 was observed in T1 compared to T0 (p=0.027); however, no significant reduction on the total score of the SRS-2 could be established at T2 (p=0.154), compared to T0 (Table 2). With respect to the analysis of the five subdomains, a significant improvement in one of Restricted, Repetitive Behaviours (RRB) and interests was observed at T1 (mean=18.95, SD=7.56, vs. mean=15.38, SD=7.18, p=0.007) compared to T0. However, no significant reduction was observed on Restricted, Repetitive Behaviours (RRB) and interests at T2 (mean=18.95, SD=7.56, vs. mean=16.52, SD=8.33, p=0.072) compared to T0. All other subdomains have shown no significant differences through T1 and T2 compared to T0. Concerning the analysis of SP, a significant reduction on low registration (p=0.026), sensory avoidance (p=0.004), and auditory category (p=0.023) was observed in T1 compared to T0; however, no significant reduction scales could be established at T2 compared to T0 on any of these (Table 3). No significant difference was found in any of the other quadrants of SP through T1 and T2 compared to T0 (Table 3). The standard deviation scores of PVT-R were not statistically significant through T1 and T2 compared to T0 (Table 4 and Figure 2).
Table 2: Social Responsiveness Scale-second edition (SRS-2).
| SPa | Mean value ± SDb | p-value | ||||
|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T0-T1 | T0-T2 | T1-T2 | |
| Low registration | 30.15 ± 8.53 | 26.90 ± 9.90 | 29.10 ± 9.92 | 0.091 | 0.297 | 0.207 |
| Sensory seeking | 52.5 ± 10.87 | 48.8 ± 17.70 | 53.3 ± 16.40 | 0.316 | 0.852 | 0.092 |
| Sensory sensitivity | 35.07 ± 8.79 | 34.50 ± 11.57 | 39.13 ± 13.77 | 0.84 | 0.181 | 0.032 |
| Sensory avoidance | 58.72 ± 14.20 | 52.40 ± 18.84 | 59.51 ± 18.22 | 0.051 | 0.816 | 0.062 |
| Auditory category | 19.70 ± 5.05 | 17.55 ± 5.42 | 20.05 ± 7.95 | 0.089 | 0.84 | 0.094 |
| Note: aSP: Sensory Profile; bSD: Standard Deviation. EZR software program (version 1.5) was used. | ||||||
Table 3: Sensory profile.
| PVT-Ra | Mean value ± SDb | p-value | |
|---|---|---|---|
| T0 | T2 | T0-T2 | |
| ssc | 6.24 ± 5.96 | 6.40 ± 6.04 | 0.664 |
| Note: aPVT-R: Picture Vocabulary Test-Revised, bSD: Standard Deviation, cSS: Standard Score. | |||
Table 4: Picture vocabulary test-revised.
Figure 2: This figure shows core of Restricted and Repetitive Behaviors (RRB) and interests of SRS-2 of three 3-year-old children at T0, T1, and T2, respectively.
Table 5 presents results of the analysis conducted within subgroups. Children aged less than 6 years (n=6) showed greater statistically significant improvement in SRS-2 total scores at T1 (mean=89.00, SD =24.55, vs. mean=68.83, SD=24.93, p=0.010) and T2 (mean=89.11, SD=24.23, vs. mean=74.16, SD=28.65, p=0.036) compared to T0. On the contrary, children aged >6 years (n=15) showed no significant improvement in SRS-2 total through T1 and T2 compared to T0. Children with higher receptive language (n=8) showed statistically significant improvement in SRS-2 total scores at T2 (p=0.037) compared to T0. On the contrary, children with lower receptive language (n=13) showed no significant improvement in SRS-2 total through T1 and T2 compared to T0. Children with a diagnosis of ASD (n=8) showed statistically significant improvements in the SRS-2 total scores at T2 (mean=69.25, SD=19.58, vs. mean=56.50, SD=18.37, p=0.027) compared to T0. On the contrary, children with severe levels of autism symptoms (n=13) showed no significant improvement in SRS-2 total through T0, T1, and T2. Children with a typical range of auditory category (n=4) showed statistically significant reduction in the SRS-2 total scores at T1 (mean=63.25 and SD=22.77 vs. mean=49.00 and SD=15.97, p=0.026), but not T2 (p=0.157) compared to T0. Furthermore, SRS-2 subdomain analysis revealed that children aged <6 (n=6) showed significant but modest improvement in the subdomain of social awareness (p=0.035) scores in T2 compared to T0. Children with higher receptive language (n=10) showed significant improvement in the social motivation in T2 compared to T0 (p=0.003) (Table 6).
| SRS-2a total score | n | Mean value ± SDb | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T0-T1 | T0-T2 | T1-T2 | |||
| Age | <6 | 9 | 89.11 ± 24.23 | 75.11 ± 25.26 | 79.00 ± 26.35 | 0.015* | 0.045* | 0.229 |
| ≥ 6 | 15 | 88.06 ± 26.79 | 85.46 ± 25.53 | 85.33 ± 29.47 | 0.434 | 0.614 | 0.976 | |
| Receptive | ≤ -1 SDb SSc | 15 | 95.20 ± 25.15 | 88.93 ± 25.72 | 91.66 ± 27.64 | 0.127 | 0.531 | 0.493 |
| Language | >-1 SDb SSc | 9 | 77.22 ± 22.58 | 69.33 ± 20.63 | 68.44 ± 22.95 | 0.096 | 0.047* | 0.851 |
| Diagnosis | ASD | 10 | 75.80 ± 23.85 | 67.30 ± 24.15 | 65.00 ± 25.04 | 0.112 | 0.022* | 0.609 |
| Autism | 14 | 97.50 ± 23.01 | 91.78 ± 21.64 | 95.78 ± 22.82 | 0.13 | 0.763 | 0.329 | |
| Auditory category | Mild | 6 | 76.16 ± 29.26 | 65.33 ± 30.38 | 70.33 ± 26.77 | 0.017* | 0.101 | 0.031* |
| Moderate | 14 | 88.28 ± 19.57 | 86.50 ± 21.42 | 86.92 ± 29.61 | 0.637 | 0.807 | 0.926 | |
| Severe | 4 | 107.50 ± 32.33 | 88.75 ± 26.60 | 88.00 ± 23.69 | 0.078 | 0.104 | 0.934 | |
| Note: aSRS-2: Social Responsiveness Scale, second edition, bSD: Standard Deviation, cSS: Standard Score. EZR software program (version 1.5) was used.*p<0.05 denotes statistical significance according to t-analysis. | ||||||||
Table 5: Group analysis of Social Responsiveness Scale, second edition (SRS-2),total score.
| Age<6 (n=6) | Autism severity mild-moderate (n=10) |
Higher receptive language(n=9) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age <6 | Mean value ± SDa | p-value | Mean value ± SDa | p-value | Mean value ± SDa | p-value | |||
| T0 | T2 | T0–T2 | T0 | T2 | T0–T2 | T0 | T2 | T0–T2 | |
| Social awareness | 12.11 ± 2.08 | 9.33 ± 2.50 | 0.042* | 10.1 ± 3.90 | 8.3 ± 2.79 | 0.177 | 10.55 ± 2.78 | 10.00 ± 2.73 | 0.609 |
| Social cognition | 19.11 ± 5.84 | 17.88 ± 6.97 | 0.209 | 14.9 ± 6.40 | 13.0 ± 6.34 | 0.032* | 14.11 ± 5.51 | 13.77 ± 7.27 | 0.834 |
| Social communication | 28.44 ± 8.09 | 25.55 ± 9.13 | 0.189 | 23.6 ± 7.26 | 20.0 ± 8.55 | 0.065 | 24.66 ± 8.23 | 20.77 ± 7.87 | 0.084 |
| Social motivation | 11.55 ± 6.55 | 12.77 ± 6.07 | 0.421 | 12.4 ± 5.54 | 12.1 ± 5.19 | 0.809 | 12.66 ± 4.18 | 10.11 ± 3.01 | 0.045* |
| Restricted, repetitive behaviors and interests | 17.88 ± 6.29 | 13.44 ± 7.61 | 0.024* | 14.8 ± 7.16 | 11.6 ± 6.99 | 0.065 | 15.22 ± 7.85 | 13.77 ± 8.10 | 0.277 |
| Note: aSD: Standard Deviation. EZR software program (version 1.5) was used. *p<0.05 denotes statistical significance according to t-analysis. | |||||||||
Table 6: Subdomain analysis of Social Responsiveness Scale, second edition (SRS-2), in a group with significant difference detected in total score of SRS-2.
Results of three children aged 3 years
The three children aged 3 years (range=44-47 months) were all males. One child received a diagnosis of autism (ADOS-2 total score=23), while two were diagnosed with ASD by the ADOS-2 criteria (ADOS-2 total score=9 and 11). The mean total listening time of the three children was 217.00 min (SD=58.75). While the total score of SRS-2 had slightly improved for one child with a diagnosis of autism, it did not improve for the other two children with a diagnosis of ASD. Among the five subdomains of SRS-2, RRB and interests was the only one that improved for all three children. Mixed results were obtained for the other subdomains. There were no significant changes in PVT-R scores or in any of the four quadrants and auditory category of SP through T1 and T2 compared to T0 for other secondary endpoints.
The present pilot study aimed to evaluate the acceptability and potential efficacy of listening therapy based on polyvagal theory on children in preschool to preadolescence with ASD. The change of social impairment associated with ASD, receptive language acquisition, and sensory processing before and after the intervention was preliminarily evaluated. The analysis of datasets involving all participants detected statistically significant reduction in the total score of SRS-2 and one of subdomains of RRB and interests, quadrants of SP. There was low registration and sensory avoidance, as well as sensory processing difficulty in the auditory domain at 1 week after the intervention compared to before the intervention.
These results were suggested to be partly consistent with those of RCTs conducted by Porges, et al. [22], in that improvement in auditory hypersensitivity could be established at 1 week after the intervention. However, because of the difference in outcomes used in the study and great heterogeneity in our sample, the increase in sharing behaviour and spontaneous speech, and improvement in behavioural organization reported by Porges, et al. [22] using parental questionnaire and video assessment were not detected in our sample. As the total SRS-2 scores 1 week after the intervention were considerably reduced, it is possible that an increase in pro-social behaviour would have been observed if a different method had been used to evaluate the behaviour of the children. The significant differences found between baseline and 1 week after the intervention, as described above, were not observed between baseline and 3 months after the intervention. As this trend was observed with different outcomes assessed in the study, it is possible that the effects obtained from SSP diminished over time. Consequently, it is suggested that examining ways to help maintain and promote the efficacy of SSP would also be critical.
In one of the subdomains in SRS-2, restricted repetitive behaviours and interests, a significant difference was detected at 1 week, and a non-significant trend was detected at 3 months after the intervention. When the improvement of the SRS-2 total score is analysed only in the cases whose RRB and interests improved 3 months after the intervention (n=12), the SRS-2 total score has improved (mean=91.00, SD=26.17 vs. mean=76.41, SD=24.82, p=0.009). In this group, no improvement was observed in a specific subdomain of SRS-2; however, all subdomains of the social communication and interaction subdomain showed slight improvement within the range of insignificant difference. Several questions arose from our results. First, the factors that contribute to the improvement of RRB and interests remain unknown. Regarding the improvement of RRB and interests among the characteristics of the children influencing the effect of SSP we focused on, a non-significant trend was observed in children aged <6 years. Considering the results that the score of RRB and interests had improved in all three 3-year-old children, children aged <6 years might be associated with the favourable response with respect to the improvement of RRB and interests. There may have been other factors that are associated with this improvement, such as anxiety [36] and stress [37]. As these conditions have been suggested to affect the ANS, these factors should be assessed in the future. Second, how the improvement of RRB and interests observed in this study is mediated through changes in autonomic function remains unknown. In one of the few Restricted, Repetitive Behaviours (RRBs) studies, Condy, et al. [38] explored the RRBs’ severity in relation to basement RSA activity and RSA reactivity, suggesting that RSA activity and RSA reactivity predicted the RRB severity using Repetitive Behaviour Scale-Revised (RBS-R). Two studies explored the effects of trans cranial magnetic stimulation sessions in individuals with ASD on bilateral DLPFC to improve autonomic inhibition (quantified as an increased RSA) in individuals with ASD [39,40]. In both studies, an increase in baseline RSA and decreased RRB symptoms were observed [39,40]. Based on these reports, the reduction of the RRBs and interests score after the intervention indicated that the cardiac vagal control might have improved after the intervention. This supports Porges’ hypothesis that increased vagal influence (via pathways originating in the nucleus ambiguous) on the heart as reflected by RSA through exercising auditory portal. Moreover, our results are consistent with the model proposed by Condy, et al. [41], which states that biological inflexibility within the central nervous system measured through RSA leads to cognitive-behavioural flexibility reflected in less impulsivity and RRBs. Furthermore, cognitive-behavioural flexibility leads to social skills. According to this preliminary finding, it could be interpreted that in our sample, children whose RRBs and interests had improved, acquired higher cognitive flexibility, resulting in more frequent engagement in social interaction after the intervention, as reflected in total SRS-2 score. Further research would be necessary for quantifying the change of cardiac vagal control using the intervention in children with ASD. Moreover, generally, the decline in social skills has tended to be the focus of attention and has been the main target for evaluation and treatment. However, we might suggest that improving RRBs could be a crucial for improving other core autism symptoms. A future task should be addressing the correlation between the improvement of RRBs and social interaction, and the intervention and cardiac vagal control (i.e., basal RSA and RSA reactivity).
Our study was conducted with a heterogeneous group of participants with a wide range of ages and language development. To overcome this problem, we grouped the patients using various clinical characteristics and used a method to detect significant differences before and after the intervention in each group. As hypothesized, in children diagnosed with ASD, who were <6-years old, and who had higher receptive language, the effects of SSP were more apparent. Further analysis of the subdomains of the SRS-2 in the groups, in which the total SRS-2 score was significantly different before and after the intervention, showed improvements in social motivation in children with average receptive language, in social awareness in children aged <6 years at 1 week and 3 months after the intervention, compared to the baseline. Though limited evidence of language development and severity of autism effects on autonomic function due to the lack of studies exists, higher symptom severity of autism [42,43] and worse language and communication skills [42,43] are reportedly associated with reduced parasympathetic activation. According to the results of these studies, it could be interpreted that children with average receptive language and mild autistic symptoms were more likely to benefit from the intervention because they originally had a higher RSA than the other group. Similarly, studies measuring the effect of age on autonomic function are very scarce; however, one study investigated the trajectory of RSA development. In their observation, while the typical group represented an increased RSA from 5 to 48 months of age, “atypical” group represented an increased RSA from 5 to 24 months, and thereafter a plateau until 48 months of age [44]. In addition, it showed difficulties with social responsiveness at 48 months of age. One might also speculate that the RSA is less likely to change with intervention depending on the length of time that the RSA has reached a plateau.
In the current study, participants varied greatly in their response to the intervention. The difference between the measured values before and 3 months after the intervention was used as standard error (standard error: 5.76); the cases where the improvement exceeded the standard error were classified as “improvement,” and the cases where the decrease exceeded the standard error were classified as “deterioration;” 42.85% participants (n=9) were classified as improvement, 38.10% participants (n=8) were classified as unchanged, and 19.05% participants (n=4) were classified as deterioration. As it remains unknown whether this was partly a worsening effect or due to other external environmental factors, more detailed outcomes and longer-term observations may be necessary for providing valid answers to this question.
Although there are several questions concerning the efficacy and feasibility of the considered intervention, which we need to explore to bring the proposed approach closer to clinical application, our findings suggest that the SSP could provide treatment options in children with ASD and foothold for guiding the further development of a large scale clinical trial in the same direction. Furthermore, our findings provide insights into the psychopathology of ASD, suggesting the importance of highlighting the balancing of the ANS clinically in reducing emotional and behavioural difficulties displayed by children.
The overall results were quite mixed in this pilot study assessing the feasibility and potential efficacy of SSP in children with ASD. Our findings suggest that this approach might be effective in improving the repetitive behaviour in children with ASD. This trial study has also implied that SSP may be especially effective for children with higher language development, who are aged <6 and have a mild severity of autistic symptoms. However, additional research is needed to determine if SSP can be a potential treatment option for symptoms associated with autism.
This study has several methodological and contractual limitations. First, our results should be interpreted with caution because of the small number of patients involved and lack of a control group. A Randomized Controlled Trial (RCT) with a substantially increased sample size should be conducted in the future. Second, this study was conducted over a 3-month period, which was not long enough to detect reliable effects, especially in terms of the evaluation of language acquisition and sensory processing. Third, the considered outcome measures were limited, all of them being based on parent reports with no semi structured or structured observational assessment. We did not assess the children’s behavioural problems at home and at school or any group setting. Moreover, physiological evaluations, such as HRV or skin conductance observations, were not conducted in this study. Future studies may expand the evaluation of behavioural and communication measures, including observational assessment and physiological tests. Fourth, there may be bias in conducting the intervention, as the implementation of the sessions relied on parental records. Fifth, concerning subgroup analysis, the results might only reflect the characteristics of the few children who responded extremely well to the intervention. There is a need to analyze the correlation between the degree of improvement and the characteristics of the children with a sufficient sample size. Finally, though none of the children presented defined symptoms of discontinuance criteria, there might be adverse effects that have not been captured during the study period. The daily symptoms, including aggressive and repetitive behaviour of children with ASD, make it difficult to interpret whether they were ASD symptoms or adverse events. Although we recognize that this intervention has been well tolerated by children with ASD, more precise evaluations regarding adverse events or worsening effects are necessary before clinical practice.
Based on our pilot study on detecting the effectiveness of SSP in children with ASD, this innovative approach seems worthy of further development and investigation. Exploratory studies are still required to establish the reliability of the measures and to define feasibility, duration of intervention, and follow-up periods. Apparently, there seemed to be a difference in response and effectiveness of the intervention, depending on the characteristics of each involved child. Successful effects were not captured for children presenting lower language development, who aged >6 years, and presented severe levels of autism symptoms. The parents of children from these groups reported a few behavioural changes in their children, such as pointing with index finger, requesting to tell the names of objects, and referencing, after the intervention. Even if such changes were subtle and did not reflect on the measures, there is a possibility that a single behavioural change can be a catalyst for further development. Accordingly, it is necessary to observe the impact of interventions in the children and their families over a long term from both quantitative and qualitative perspectives. Moreover, as mentioned above, further research is necessary to explore changes in their biological system with respect to the intervention. Consequently, future research in this direction should be directed at physiological evaluation and observation of changes in autistic symptoms after the intervention in children with ASD.
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
Citation: Kishimoto M, Sekido Y, Kawai H, Takaki M (2023) Effects of Safe and Sound Protocol System on Psychological and Physiological Functions of Children with Autism Spectrum Disorders: Preliminary Findings. J Psychol Psychother.13:455.
Received: 18-Jun-2023, Manuscript No. JPPT-23-25192; Editor assigned: 21-Jun-2023, Pre QC No. JPPT-23-25192 (PQ); Reviewed: 05-Jul-2023, QC No. JPPT-23-25192; Revised: 12-Jul-2023, Manuscript No. JPPT-23-25192 (R); Published: 19-Jul-2023 , DOI: 10.35248/2161-0487.23.13.455
Copyright: © 2023 Kishimoto M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.