International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2022)
Background: Central cervical cord injury presents with sensory deficits in the hand. Literature has shown that humans can detect the friction that occurs when manipulating objects, and can perform finger muscle activity in response to this friction. However, to date, there is no established approach that can improve dexterity in people with hand sensory-motor impairments after central cervical cord injury. Therefore, we conducted rehabilitation using a tactile-discriminating, sensory-feedback compensation system device and investigated the efficacy of this intervention. Methods and findings: This case study had an interventional design. The patient complained of sensory-motor dysfunction of the hand after a central cervical cord injury. The study duration included 2 weeks of pre- and post-intervention evaluation and 6 weeks of rehabilitation performed at hospital B. Pegboard task, building block stacking task, and material identification task were performed every 10 minutes in each session. The left hand was evaluated for sensory and motor function and learnability. Additionally, electroencephalogram measurements showed that deep sensation, sense of agency, left hand numbness, and motor frequency improved post intervention. Furthermore, there was a reorganization of the sensory-motor domain. However, it was difficult to statistically determine the efficacy of the rehabilitation approach as our study was limited to a single patient. Prospective studies with a larger sample size are necessary to determine the efficacy of the rehabilitation approach statistically and definitively. Conclusion: This suggests that a rehabilitation approach using this device can be effective for patients with sensorymotor dysfunction of the hand following central cervical spinal cord injury.
Central cervical spinal cord injury; Sensory-motor impairment; EEG; Sensory feedback
ADL: Activities of Daily Living; AOU: Amount of Use; EEG: Electroencephalogram; FMA: Fugl- Meyer Assessment; MAL-14: Motor Activity Log-14; MCID: Minimal Clinically Important Difference; MMT: Manual Muscle Testing; NRS: Numerical Rating Scale; PCS: Pain Catastrophizing Scale; QOM: Quality of Movement; STEF: Simple Test for Evaluating hand Function
Central cervical spinal cord injury (hereafter referred to as cervical cord injury) is the most common type of incomplete cervical cord injury that presents with sensory deficits in the hands [1]. The sensory features of the hand, including fingers, are responsible for detecting sensory information within the hand that occurs during motor execution and for reflexively regulating motion [2]. However, if afferent pathways of the central nervous system are blocked or attenuated by feedback from the somatosensory system due to some effect, reflexive muscle coordination using somatosensory information cannot be performed. Thus, it results in more variation in force during motion when grasping the object with the hand and the inability to grasp the object sufficiently [3]. This is called sensory-motor dysfunction of the hand, and this disorder can occur regardless of the pathway from the dorsal root of the spinal cord to the cerebral cortex, the afferent pathway of the central nervous system [4,5]. Therefore, sensory-motor dysfunction of the hand is more prone to occur in central nervous system diseases, such as stroke [4], in which cerebral lesions present disorders of the sensory-motor domain, and in orthopedic diseases, such as cervical cord injury [6], in which compression of the spinal cord causes neurological deterioration of the afferent pathways, including the posterior cord and dorsal horn.
In the past, approaches combining real-time feedback, such as visual, electrical, and auditory feedback, have been used for the rehabilitation of individuals with impaired hand dexterity after central neural damage, with reports of functional reorganization of the sensorimotor cortex in the brain and improvement of gross motor function [7,8]. One possible reason for the effectiveness of these methods is the possibility that the information matching between motor intention and sensory feedback of the treated limb could be synchronously processed in the brain. Synchronous information processing implies that motor intention and sensory feedback are processed in the brain within 250 milliseconds (0.25 s) without any discrepancy, generating a “sense of agency” that the participant is the one performing the movement [9]. This sense of agency [9], has been reported to increase activity in the premotor cortex and corticospinal tracts and establish motor learning, thereby improving upper limb performance [10].
However, when manipulating an object, humans need to visually confirm the coordinates of the object and perform hand muscle activities corresponding to dynamic friction by detecting friction that occurs on continuously touching the object with the hand (hereafter, dynamic friction) via sensory receptors in the fingertips [11]. Therefore, as feedback, approaches that use visual, electrical, or auditory stimuli for performing skillful movements may be insufficient, as they cannot detect the dynamic friction that occurs when touching an object.
Previously, Kitai et al. [12] reported an approach using a system that provides real-time feedback of vibration information generated on touching an object with the hand, in addition to the synchronous matching of visual information with hand movements, to stroke patients that, along with cervical cord injury, are prone to exhibit sensory-motor dysfunction in the hand. The authors reported that the neural activity of the sensory processing function in both sensory-motor areas increased as well as the sense of agency during hand movements improved. Thus, compensatory and realtime feedback of visual and vibration information during hand movements can reorganize the sensory-motor cortex and facilitate motor learning for hand dexterity movements in a patient who’s sensory and motor areas were damaged by stroke.
On the other hand, cervical cord injury, although a central nervous system injury, is a condition in which sensory feedback stimuli associated with movement are likely to be input into the brain as noise due to damage to sensory relay points rather than to the sensory-motor function integration site in the cerebral cortex [5]. The input of sensory information into the brain that does not match the actual motion induces abnormal perception in the brain [13], and the mismatch between the motor intention and sensory feedback reduces the sense of agency. Therefore, it is difficult for motor learning to be established. Dahlgren et al. [14] reported that after the injury of the cervical cord, the sensory-motor dysfunction in the hand can affect Activities of Daily Living (ADL) even after years of its onset. Therefore, to improve the sensory-motor dysfunction of the hand after cervical cord injury, it is important not only to match the sensory feedback with the motor intention in the brain, but also to ensure that the sensory feedback input is appropriate. However, an effective approach for improving skillful movements of the hand, which satisfies these conditions, has not been designed. A universally-accepted, effective rehabilitation approach could potentially help patients suffering from cervical cord injury complications recover their ADL.
Therefore, we aimed to test and validate the effectiveness of the real-time and compensatory approaches for transmitting vibration information by touching the hands of a patient with sensory-motor dysfunction caused by damage to the sensory relay point after cervical cord injury.
The results of this study suggested that a sensory compensatory approach for patients with sensory-motor dysfunction in the hand after cervical cord injury may improve hand ADL function and dexterity movements by enabling appropriate sensory input. This study may represent a new contribution to the field of neurorehabilitation.
A 59-year-old left-handed man was involved in a rear-end collision by a car approximately 6 months ago; he was urgently transported to hospital A with a diagnosis of cervical cord injury (Figures 1A and 1B). Magnetic resonance imaging revealed that the anteroposterior diameter of the spinal canal was highly reduced at the C5/C6 and C6/C7 levels. Clinical findings were marked numbness in both C6 regions, muscle weakness below both wrist joints, and hypersensitivity to cold sensation. Therefore, he underwent C2 domeplasty and C3–7 vertebroplasty at hospital A. Approximately one month after the onset of cervical cord injury, he was transferred to the convalescent ward of hospital B for rehabilitation, where physical and occupational therapy was provided for approximately 2 hours a day, over 5-6 weeks. The approach during hospitalization included upper limb muscle strengthening training, joint range-of- motion training around the scapula, application of hot packs on the forearms and hands, and dominant hand exchange exercises. As a result, Manual Muscle Testing (MMT) of both hand joints in all directions was >4, and hand function improved sufficiently to allow the patient to return to work in the steel industry. However, the left-hand side still had extremely strong numbness on the Numerical Rating Scale (NRS) (0: not at all and 10: extremely strong) [12] at 8/10, and the hand dexterity remained impaired. In addition, the hypersensitivity to cold persisted on the left-hand side.
Figure 1: Cervical spine MRI shows left nerve root compression at levels A: C5/6 and B: C6/7.
Approximately 4 months after the cervical cord injury, the patient was discharged from the hospital, following which an occupational therapist performed the same approach as that performed during hospitalization, twice a week for 20 minutes each at hospital B's outpatient rehabilitation program. After approximately 6 months, the patient requested an approach to manage sensory-motor dysfunction of the hand; hence, when he visited our hospital for outpatient rehabilitation, a physical therapist at hospital B performed an exercise task using the Yubi-Recorder on the numb left hand twice a week for 30 minutes. Motor function was confirmed, and the patient could perform the research task prior to the measurement. We also confirmed that the patient did not have issues with respect to cognitive function, communication, or sudden seizures (poor general condition) such as epilepsy.
The study was conducted with approval from the Kyoto Tachibana ethics review committee (approval No: 20-33). The patient was provided with a written consent form explaining the purpose, content, and procedures of the study. After answering their questions and obtaining their consent, a copy of the form was handed to them.
Intervention and evaluation methods
The hand captures the dynamic friction generated during object manipulation with tactile receptors and performs fine control of muscles in response to dynamic friction. To address these issues, Tanaka et al. [15] developed the Yubi-Recorder, a system device that detects minute changes in the dynamic friction generated when the hand touches the object as vibration information and provides feedback as vibration information in real-time. It is capable of sensing unevenness, flatness, curvature, and roughness, and can capture tactile stimuli from any object shape, making it suitable for multi-directional motion. The sensor that detects vibration is attached to the distal interphalangeal joint of the index finger, and by modulating the information from the sensor to the frequency that humans perceive, tactile stimuli can be synchronously presented to their own body through the sensor as vibration stimuli.
The approach consisted of a 10 minute task in which the patient was asked to stack square blocks with his left hand with a base scale of 3 cm, as used in a building block stacking task; a 10-minute task in which the patient was asked to discriminate five sandpaper pieces using the ventral part of the left index finger (a material identification task); and a 10 minute task in which the patient was asked to insert a steel peg (25 mm long and 3 mm diameter) into a board (pegboard task) with two rows of 25 holes arranged vertically with the left hand (peg manipulation exercise). The site of transducer attachment used during the approach was the left acromion or left temporal bone, which is used in the vibratory perception test. For the vibrator attachment selection method, sandpaper was used, referring to the method of Kitai et al. [12]. In this study, five types of sandpaper with different coarseness were applied to the left acromion or left temporal bone, and the area where the coarseness of the sandpaper could be distinguished was defined as the area where the sensory compensation could be performed. The intervention period was 6 weeks, and the approach was performed five times each week.
To test the impact of the Yubi-Recorder approach, the left-hand side was compared before and after the intervention in terms of sensory and motor feature assessment, learnability, and Electroencephalogram (EEG) measurements (evaluation A). At the end of each week, peg tests were performed to assess the motor function of the left hand over time (evaluation B).
For the sensory function evaluation, two deep sensory tests of the hand were conducted: the position and motor sense tests. In the position sense test, the examiner moved the patient's healthy hand, and the patient was asked to mimic the action with the affected hand. In a motor sense test, with the patient’s eyes closed, the examiner moved the affected thumb in a motion, and the patient was asked to verbally answer the direction in which he moved it. Each test was performed five times and the number of correct answers was used to make a judgment. NRS [12] and PCS [16] were administered to evaluate numbness; for PCS, all responses with pain in the questionnaire were converted into numbness. The patient was asked to rate these states: numbness stuck in the head (rumination), feeling helpless to do anything about numbness (helplessness), and thinking that numbness was stronger than the actual numbness (magnification).
Motor function assessment of the upper extremities, including the hands, was performed by Fugl-Meyer Assessment (FMA) [17], a Simple Test for Evaluating hand Function (STEF) [18], and peg test [19]. In addition, grasp force measurement was performed using a GFD50-A grasp force meter (Tech Gihan Co., Ltd., Kyoto, Japan) to measure time and acceleration during hand dexterity movements. The FMA is a comprehensive test to evaluate upper limb motor functions such as single joints, compound joints, object grasping, and upper limb coordination and movement speed. STEF consists of 10 subtests, each involving grasping and moving objects of varying sizes and shapes, measuring the time required for a series of motions, and scoring 1-10 points depending on the time required to perform the task. The peg test is performed by inserting a 25 mm long, 3 mm diameter steel pin into the board with two vertical lines of 25 holes within 30 seconds. Grasping force measurement is an evaluation that uses a gripping force meter to measure the time and acceleration of the gripping force meter as it moves, which can be divided into three components of X, Y, and Z axes. To unify the moving distance of the grasping force meter, two pieces of paper of 53.7 cm width and 25.4 cm length were placed side by side, referring to the Box and Block test [20], a hand dexterity evaluation technique. Subsequently, a 15.2 cm high partition was placed between the two sheets of paper, where the midpoint of the left and right papers was marked, and the grasp force meter was set to move from the left to the right midpoint. The grasp force meter was set to be evaluated with weights of 5 g, 10 g, 17.8 g, 31.2 g, and 62.4 g. The patient performed each task three times on each side, and the time and acceleration were recorded. In the evaluation of time, the mean value and standard deviation were calculated for each task that was performed three times each, and the final values were then obtained from the sum of the two. For the evaluation of acceleration, the values were measured separately in the three axes of X, Y, and Z, and the mean and standard deviation of the combined values were obtained by multiplying the values by the coefficient transmitted to the hand for each frequency (hereafter, three-axis composite value). The obtained data were entered into the following formula.
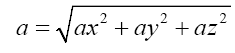
For each task that was executed thrice, the average time required for the grasping task and the average triaxial composite were computed. The mean and standard deviation were computed from the sum of the two. It requires that the grasp force meter be moved rapidly to reduce the execution time of the task. However, when the grasp force meter is moved rapidly, acceleration increases in the gripper force meter and hand, and the three-axis composite value becomes large. To perform the task immediately, it is necessary to control the increased acceleration within the finger abdomen so that the hand does not drop the grasp force meter. Hence, the shorter the average grasping force task time, the more smoothly the upper limb moves while controlling the acceleration generated by the grasp force meter and the hand within the finger abdomen.
We administered Motor Activity Log-14 (MAL-14) [21], which is useful to assess the ADL that require dexterity, and the quality of life assessment tool can determine the amount of hand use and the quality of movement. For each question item of MAL-14, we also assessed the relationship between behavior change and sense of agency by referring to the NRS motor initiative [12].
For neurophysiological evaluation, EEG measurements were performed using active electrodes (g.tec medical engineering GmbH, Austria) and a bio-signal measurement device, Livo (Tec Gihan, Co., Ltd., Kyoto, Japan). The patient first performed the peg task without the Yubi-Recorder attached to his left-hand side (no Yubi-Recorder condition). Subsequently, the patient performed the peg task with the Yubi-Recorder attached to his left hand (with Yubi-Recorder condition), and measurements were recorded during the performance of the task in each condition. We measured EEGs at 17 sites (Fpz, Fz, Cz, Pz, Oz, F3, F4, C3, C4, P3, P4, F7, F8, T7, T8, A1 and A2) using both earlobes as reference electrodes, which is based on an International 10-20 method. The bandpass filter was set at 0.5 Hz–60 Hz and sampling frequency at 1000 Hz. Data measured by EEG devices were spatially analyzed using exact Low Resolution Brain Electromagnetic Tomography (eLORETA) analysis, a three-dimensional imaging method for neural activity in the brain [22]. In this analysis, EEG data is computed as x-, y-, and z-directions in the brain region divided into 6239 voxels using a linear transformation, and then transformed into a threedimensional image using a non-linear transformation to correct for curved anatomy. Therefore, the neural activity region for each task state is computed as the cranial neural activity value (µA/mm2) at each voxel and can be expressed as the Brodmann area. In addition, the immediacy of Yubi-Recorder and comparisons between pre- and post-intervention conditions allowed identification of differences in the brain activity values obtained for each task condition using the statistics LORETA SnPM 26 (multiple paired t-test with nonparametric randomization) [23] in the same analysis program.
Study protocols included single-week pre-intervention evaluations (evaluation A), followed by 6-week interventions plus longitudinal evaluations (evaluation B). Subsequently, the study was completed with a single-week post-intervention evaluation (evaluation A).
A sensory feature evaluation showed an improvement in the left-hand position sense. Numbness of the left hand showed improvement, and PCS improved in terms of rumination, helplessness, and magnification (Table 1).
In the motor function, the FMA of the left upper extremity improved in relation to the reflex action of the shoulder/elbow/ forearm, wrist, and fingers, and the coordination/speed.
In STEF, the left hand improved to the same score as the initial evaluation of the right (Table 1). In the peg test, the left hand showed improvement (Figure 2). In the left-hand grasping force measurement, task performance time was reduced in the final task compared to the initial task; three-axis composite value did not change significantly between the initial and final evaluations, but the standard deviation was larger in the final evaluation (Figures 3A and 3B).
| Initial evaluation | Final evaluation | |
|---|---|---|
| Position sense (times) | 1/5 | 5/5 |
| Motor sense (times) | 5/5 | 5/5 |
| Numbness (NRS) | 8/10 | 8/10 |
| PCS (Point) | Total: 43/52 | Total: 40/52 |
| Rumination: 20/20 | Rumination: 19/20 | |
| Helplessness: 16/20 | Helplessness: 15/20 | |
| Magnification: 7/12 | Magnification: 6/12 | |
| FMA (Point) | Total: 54/66 | Total: 61/66 |
| Shoulder/elbow/forearm: 31/36 | Shoulder/elbow/forearm: 35/36 | |
| Wrist: 9/10 | Wrist: 9/10 | |
| Fingers: 10/14 | Fingers: 11/14 | |
| Coordination/speed: 4/6ã?? | Coordination/speed: 6/6ã?? | |
| STEF (Point) | Right: 84/100 | Right: 90/100ã?? |
| MAL-14 | Left: 70/100 | Left: 84/100 |
| AOU (Point) | 45/56 | 50/56 |
| QOM (Point) | 44/56 | 42/56 |
| Sence of Agency(NRS) | 80/140 | 101/140 |
Note: NRS: Numerical Rating Scale; PCS: Pain Catastrophizing Scale; FMA: Fugl-Meyer Assessment; STEF: Simple Test for Evaluating hand Function; MAL-14: Motor Activity Log-14; AOU: Amount of Use; QOM: Quality of Movement.
Table 1: Physical therapy assessment.
Figure 2: Peg test.
Figure 3: Grasping force measurement. A: Time required for grasp force task; B: three-axis composite value. Note:  Unit: m/s2.
Unit: m/s2.
MAL-14 had an improvement in the Amount of Use (AOU) and Quality of Movement (QOM); the MAL-14 sense of agency NRS improved in the learnability assessment.
On EEG, in the no Yubi-Recorder condition, there was increased neural activity in the right primary and secondary visual cortices. In contrast, in the Yubi-Recorder condition, neural activity was enhanced in the right primary somatosensory cortex, both superior and inferior parietal lobes, and the right primary motor cortex (Figure 4 and Table 2).
| Task Conditions | Brodmann Area | Neural activity values | |||||
|---|---|---|---|---|---|---|---|
| x | y | z | Brain lobe | (μA/mm2) | |||
| Peg manipulation practice (left hand) | |||||||
| Condition without Yubi-Recorder (red) vs. Condition with Yubi-Recorder (blue) | |||||||
| Red | 30 | -95 | 0 | Right posterior cephalic lobe | Secondary visual cortex | 18 | 2.46 |
| Blue | 25 | -55 | 70 | Right superior parietal lobe | Somatosensory association cortex | 7 | 2.03 |
| Pre-intervention (red)<Post-intervention (blue) | |||||||
| Blue | 25 | -55 | 70 | Right superior parietal lobe | Somatosensory association cortex | 7 | 2.4 |
Table 2: Most neural active sites and Montreal Neurological Institute (MNI) coordinates for each condition.
Figure 4: Neurally active regions with enhanced activity. Gray: condition without Yubi-Recorder and Black: with Yubi-Recorder.
To investigate the pre- and post-intervention effects, cranial neural activity during peg test performance with the left-hand side was assessed at the initial and final evaluations, and identification was performed based on differences in neural activity values. Results showed that compared to the initial assessment, the final assessment increased neural activity in the right primary somatosensory cortex, both superior and inferior parietal lobes, and the right primary motor cortex (Figure 5 and Table 2).
Figure 5: Neurally active regions with enhanced activity. Gray: Pre-intervention and Black: Post-intervention.
The patient suffered from a cervical cord injury approximately 6 months ago due to a traffic accident and underwent C3-7 vertebroplasty. However, numbness on the left-hand side persisted, which caused a suspicious motor dysfunction. Therefore, to improve the sensory-motor dysfunction of the left hand, the Yubi-Recorder approach was used. The Yubi-Recorder is a system device that provides feedback vibration information in real-time, in addition to synchronously matching visual information. The effects of this approach were evaluated in terms of brain function, sensory function, upper limb motor function, and learning ability.
With respect to sensory function, it improved in the left-hand position. On appropriately providing the motion-related sensory feedback, the sensorimotor cortex was reorganized and the depth senses were able to detect motion errors induced by motion prediction and post-movement feedback [24]. Therefore, this considered the use of the Yubi-Recorder to detect motor errors that occurred between motor prediction and actual motion and to reorganize the sensory-motor domain based on EEG results. The results of the EEG and position sense tests indicated that during depth sense testing, the patient was able to keep track of the hand movement information. In addition, numbness in the left hand improved. To perform movements efficiently, humans have the ability to block out unnecessary information once sensory information is provided as input [24]. Therefore, it was considered that the real-time input of dynamic frictional information necessary for movement suppressed the sensory input of numbness, which is unnecessary information for movement, and improved the NRS of numbness. PCS results showed improvement in catastrophic thinking. Numbness has been reported to be elicited by a temporal mismatch in information matching regarding motor intention and sensory feedback [25]. Before the intervention, the patient had a reduced sense of agency on the left-hand side, suggesting that sensory-motor discrepancy contributed to the numbness caused by organic changes in afferent conduction pathways due to stroke, owing to its chronic nature. EEG results showed that neural activity in the right primary somatosensory cortex was increased immediately after exercise and that the approach using the Yubi- Recorder temporally matched motor intent and tactile information, which generated a sense of agency and improved numbness due to the cognitive aspect of exercise.
For the motor function assessment, the Minimal Clinically Important Difference (MCID) in central nervous system disease for FMA was 4.75-7.25 [26], and exceeding MCID was considered to indicate that the treatment was effective. The case showed an improvement of 7, indicating that the intervention was effective. The case showed an improvement in arm/elbow/forearm and in coordination/speed which were close to the highest and best scores. The EEG results showed increased neural activity in both superior and inferior parietal lobes, and right primary motor cortex [27], which are important parts of motor image formation during left-hand dexterity movements and increased activity in the sensorimotor cortex, which was considered to have improved motor function at the upper extremity as a whole. However, although in this case FMA was improved, the reduction in the gripped item remained unchanged at 3 before and after the intervention. The reason why the scores for the grasping item did not change was that the Yubi-Recorder is a system device that provides real-time feedback of vibration information generated when touching an object with a hand [15]; but, it has been reported that this does not lead to improved muscle strength of the hand [12]. Therefore, the patient also required a separate intervention for the hand muscle strength to improve the grasping motion. In addition, in the left-hand side peg test, STEF improved, indicating improvement in left-hand side motor feature, object-carrying ability, and dexterity. The grasping force measurement showed improvement in task execution speed, which was attributed to an increase in acceleration and blurring range of the three-axis composite value. Deep sensing has the feature of capturing pressure changes associated with joint motion and fine motor control of the hand [28]; this could also improve depth sensation in the left hand, which enabled the control of dynamic friction generated in the finger pad and the ability to transport and manipulate the object rapidly.
MAL-14 showed an AOU improvement, an improvement over MCID in central nervous system disease of 0.5 [29], and an increased frequency of left-hand side use in the learnability evaluation. It is known that when abnormal perception occurs, learned non-use results from the unpleasant effect and interhemispheric inhibition from the healthy motor cortex [30]. The patient was also considered to have learned non-use due to abnormal perception caused by numbness. Since behavioral change is attributed to motor learning [31], it has been considered a necessity to improve the learned disuse. The sense of agency at the cognitive level, besides the sense of agency at the sensory level, in which motor prediction and sensory feedback coincide temporally, is also considered important [32]. Based on the evaluation of the sense of agency using MAL- 14, we consider that the patient’s sense of agency at the cognitive level, in addition to agency sense at the sense level, improved that resulted in a better behavioral index, AOU. On the other hand, MCID in central nervous system disease for QOM, which should be over 1.1 decreased [33]. The patient stated, "My fear of touching things has decreased, and I am able to perform a variety of tasks, but numbness intensifies when I touch cold objects, but I'm able to do so." Roughness perception and warm and cold perceptions are important in recognizing the material quality of an object with a hand [34], and we consider that the hypersensitivity to cold perception has been due to the lack of increased QOM scores.
The peg test was performed in EEG to evaluate the immediacy of using the Yubi-Recorder system on the left-hand side, and the identification was based on the difference in brain neural activity values during the task in both conditions. The results showed that the peg test without the Yubi-Recorder increased the neural activity in the right primary and secondary visual cortices. It has been reported that individuals with sensory-motor dysfunction in hand can perform movements as a means of visual compensation [35]. The primary visual cortex receives directional information directly from the lateral geniculate nucleus, which sends information to the visual association cortex [36]. A secondary visual cortex is an area associated with spatial attention, an action to direct attention to a specific location, and that information is sent to the superior parietal lobule and primary motor cortex [37]. The function of these visual areas enables humans to grasp the relationship between the hand and object in space and to move the hand in the direction of the object. The participant said, "I have difficulty manipulating objects because my hand is numb." It was considered that he was performing the motor task by understanding the positional relationship between his hand and the object by compensating for the right visual cortex because he had difficulty detecting the dynamic friction generated between the hand and the object due to abnormal sensation. However, besides visual information, recognizing touch sensation is important when manipulating an object with a hand, and the appropriate motor action is selected by continuing to recognize this sensation [38]. In other words, object manipulation, which relies on vision, lacks sensory information to track intra-body information. Therefore, it is impossible to detect dynamic friction that occurs between the hand and within the object, and the motor output of the hand is easily over-or underactuated. Therefore, it is considered that the patient also lacked the ability to monitor the information inside the body, despite the mild motor dysfunction of the hand, resulting in lower scores on the skillful movement task compared to those of the right.
In the condition with the Yubi-Recorder, neural activity in the right primary somatosensory cortex, both superior and inferior parietal lobes, and the right primary motor cortex increased. Sensory transmission from the primary somatosensory cortex to the parietal association cortex integrates multisensory information, including visual and somatosensory information, and clarifies perception [39,40]. The perceived information is then sent to the primary motor cortex to enable smooth hand movements [41]. Thus, at the end of the evaluation, the sensory processing pathways in both parietal lobes processed the information necessary to manipulate the object, and the right primary motor cortex could be used for motor control.
To investigate the effects of the intervention, cranial neural activity during peg test performance with the left-hand side was assessed at initial and final evaluations, and identification was based on differences in neural activity values. The results showed that the final assessment increased neural activity in the right primary somatosensory cortex, both superior and inferior parietal lobes, and the right primary motor cortex. Such findings suggest that the Yubi-Recorder approach can be applied to restructure the sensorymotor areas and improve the motor control function when the left hand performed a skillful motion.
This study had some limitations. Primarily, the study was conducted using FMA and MAL-14 MCID to separate the effects of tactile discrimination feedback with the Yubi-Recorder from those obtained with sustained movement. Results of the evaluation suggested improvements in the motor function and utilization of the left hand. Prospective studies, conducted in an A (baseline period)-B (treatment period)-A (baseline period) intervention design will be required to improve the accuracy of determining interventional effects using a Yubi-Recorder. This method would allow for an in-depth examination of the interventional effects and establish it as a novel rehabilitation technique. Additionally, the brain activation patterns recorded by EEG may not directly reflect the cognitive and motor stimulation associated with the intended intervention. To compensate for the limitations of this study, a stratified randomized trial with a large sample needs to be conducted to demonstrate and statistically determine the effects of the intervention. Positive outcomes of such prospective studies are expected to help improve the ADL and quality of life of patients with cervical cord injury. The findings of our study significantly contribute to the evolving evidence-based medicine for neurorehabilitation therapy worldwide.
This study suggests that an approach using the Yubi-Recorder, a system device that synchronously matches visual information and provides feedback vibration information to patients with sensorymotor dysfunction in the hand after cervical cord injury, improves deep sensations and the ability to control the dynamic friction produced by the left hand. Brain processing increased neural activity in both parietal sensory processing pathways and in the right primary motor cortex. The results also suggested that the left hand may improve sense of agency, catastrophic thinking, and extent of left-hand use.
We would like to express our sincere gratitude to our male participant who understood the purpose of this study and was willing to work together with us. Thank you very much.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Kitai K, Ueda T, Yamauchi R, Mizushima Y, Murata S, Nakano H, et al. (2022) Effectiveness of Sensory Compensation Approach for Hand Sensory-Motor Dysfunction Following Central Cervical Spinal Cord Injury. Int J Phys Med Rehabil.10:649.
Received: 15-Aug-2022, Manuscript No. JPMR-22-18852; Editor assigned: 18-Aug-2022, Pre QC No. JPMR-22-18852 (PQ); Reviewed: 07-Sep-2022, QC No. JPMR-22-18852; Revised: 14-Sep-2022, Manuscript No. JPMR-22-18852; Published: 23-Sep-2022 , DOI: 10.35248/2329-9096.22.10.649
Copyright: © 2022 Kitai K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.