Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2025)Volume 10, Issue 1
Purpose: The study aimed to investigate the effectiveness of Parent-Initiated Early Motor Enrichment (P-EME) on motor skill development in preterm low birth weight infants.
Design and methods: Sixteen parent-infant dyads were recruited for a pre-post experimental study, with the experimental group receiving six weeks of P-EME activities, such as visualizing/tracking toys, hand-to-hand and handto- foot play, assisted kicking, prone play, head control practice, and sitting with upper trunk support. The Peabody developmental motor scales-2 was used as an outcome measure.
Results: The results showed significant improvements in both Gross Motor Quotient (GMQ) and Fine Motor Quotient (FMQ) after treatment, particularly in very low birth weight infants who had poor fine motor development.
Conclusion: The study suggests that P-EME can facilitate motor development in preterm low birth weight infants and reinforces the importance of parental engagement in early intervention services. However, a robust clinical trial is necessary to establish the present findings.
Early intervention; Early movement experience; Preterm; Low birth weight
Preterm low birth weight is defined as a baby born alive before 37 weeks of pregnancy and with a birth weight of less than 2500 grams. According to World Health Organisation (WHO), globally, every year, 15 million babies are born preterm, and almost 15% of all births worldwide are low birth weight [1]. The prevalence of infants born preterm low birth weight in low and middle-income countries was second highest, accounting for 13.2%-18.2% [2].
Preterm low birth weight is an important determinant of child health as it is associated with greater risk of death, poor health, and disabilities in early life and at later ages are at higher risk of developmental delays in all the domains compared to infants born full term [3]. In low and middle-income countries, due to poor socioeconomic conditions and lack of awareness high-risk infants having neurodevelopmental disorders go undetected in the early years of life and thereby deprived of early identification and early intervention to prevent disabilities and facilitate optimum health conditions [4].
The way infants move and interact with objects during early development shapes their understanding of the world and there is increasing recognition that parents play a critical role in promoting health outcomes in this phase [5]. These types of positive interactions help to establish social competency and secure attachment, which are essential for later social, language, and cognitive development [6]. A variety of early intervention programs have been developed, which are delivered by professionals in Neonatal Intensive Care Units (NICUs) or pediatric rehabilitation hospitals [7]. While there is evidence demonstrating the effectiveness of these early interventions promoting children’s health and psychosocial development, they limit their capacity to provide a comprehensive representation of the effectiveness of early intervention programs as delivered by parents of preterm low birth weight infants [8]. Hence the present study is planned to determine the effectiveness of parent provided early movement experience for preterm low birth weight infants on motor skill development.
In this pre-post experimental study, data were collected from September to February 2022 at Tertiary Care Hospital, Belagavi. Preterm low birth weight infants at corrected age (is premature baby's chronological age minus the number of weeks or months she/he was born early) of 1-2 months with parents of more than 18 years of age with a minimum education of 12th standard and consent to participate and provide written consent to the research and publication of the results were included. The infants who were critically ill or diagnosed with genetic disorders, congenital anomalies, metabolic diseases, respiratory distress and existing neuromotor disabilities and history of surgery in the last 1 month were excluded. The sample size was calculated using the T statistic and non-centrality parameter, A value of N=16.1823 gives the following calculations: NCP=Non- Centrality Parameter=√N*E/SΔ=2.8159. DF=Degrees of Freedom=N-1=15.1823. tα=Inverse of the T distribution with the given probability of 1-(α/2) and DF of 15.1823=2.1292. Beta (tα, DF, NCP)=0.250006 and power of 1-α of 0.75. The N thus calculated is rounded up to the next highest integer to give the group size of N=17. To avoid selection bias, systematic sampling method was used for recruitment. CONSORT diagram showing the flow of participants through each stage of a trial is depicted in Figure 1. Early movement experience activities were demonstrated to the parent to be performed at home for six weeks, 2 to 4 minutes for each activity for a total of 20 minutes/ day, which can be done in one session or shorter session. The intervention included visualizing/tracking toys (squeeze-toy, rattle), hand-hand and hand-foot interaction, kicking-activities, prone play, head control practice, sitting with upper trunk support. The demonstration was performed till the parent understood and performed the activity completely and had the confidence to perform it in the absence of supervision. The parent was provided a pictorial description of the activity in the form of a daily activity logbook. Follow-up was done through a phone call to check adherence to the intervention at the 2nd and 4th weeks. After completion of 6 weeks of intervention, infants’ post-assessment was done using PDMS-2. Peabody developmental motor scale-2 assess fine (grasping and visual-motor integration) and gross motor (reflex, stationary, locomotion and object manipulation) development of children from birth to 5 years was used as an outcome measure. The manual reports a good index of internal consistency for each subtest α=0.89 to 0.95 and for each motor quotient 0.96 to 0.97 [9]. The administration of PDMS-2 was done by an experienced physiotherapist. The obtained raw scores for each subtest of the scale were converted Clin Pediatr, Vol.10 Iss.3 No:1000306 to age equivalent, percentile and standard scores. The sum of the standard scores were converted to Gross Motor Quotient (GMQ), Fine Motor Quotient (FMQ), and a Total Motor Quotient (TMQ). All the values were recorded on the summary score sheet and entered into the excel spreadsheet. Data cleaning was done before analyzing the data. Statistical analysis was done using R i386 3.6.3. Continuous variables are represented by mean ± standard deviation. Categorical variables are represented by frequency tables. Paired continuous data are compared using paired t-test and Welch test. P-value<0.05 was considered significant. Approval for the study was obtained from Institutional Ethical Committee (KIPT/Sl no-. 701/7/8/20) and registered with CTRI (CTRI/ 2021/01/030372).
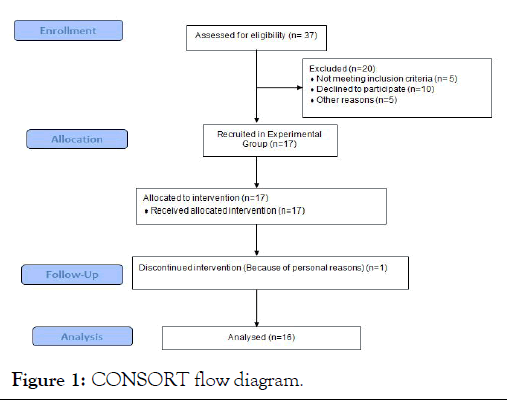
Figure 1: CONSORT flow diagram.
Baseline characteristics of the 16 mother-infant dyads in the study: It was observed that 9 of 16 participants in the sample were females. The mean corrected age of infants at baseline was 83.87 ± 14.13 days, with a mean birth weight of 1.58 ± 0.33 kg. The mean gestational age was 33.13 ± 2.5 weeks. Four participants were very low birth weight, and 12 were moderate low birth weight. The average stay in NICU is 8.06 ± 9.65 days. The mean age of the mother was 27.75 ± 3.34 years, and most of the mothers were educated to graduate level. Six parents were in lower middle income, and ten parents were in the upper middleincome category (Table 1).
| Characteristics | Sub-category | Value | Frequency (%) | Mean ± SD |
|---|---|---|---|---|
| Gender | Male | - | 7 (43.75%) | - |
| Female | - | 9 (56.25%) | - | |
| NICU stay (in days) | 0 days | - | 5 (31.25%) | 8.06 ± 9.65 |
| 1-10 | - | 7 (43.75%) | ||
| >10 | - | 4 (25%) | ||
| Gestational age (in weeks) | <32 | - | 6 (37.5%) | 33.13 ± 2.5 |
| 32-37 | - | 10 (62.5%) | ||
| Infant’s corrected age (in days) | - | 16 (100%) | 40.44 ± 11.05 | |
| Birth weight (in Kgs) | VLBW (<1.5) | 4 (25%) | 1.58 ± 0.33 | |
| MLBW (≥ 1.5) | 12 (75%) | |||
| Birth height(in Cms) | 16 (100%) | 42.5 ± 3.48 | ||
| Mothers age (in years) | 16 (100%) | 27.75 ± 3.34 | ||
| Socio-economic status | Lower middle | 6 (37.5%) | ||
| Upper middle | 10 (62.5%) | |||
| Mothers’ qualification | PUC | 4 (25%) | ||
| Graduation and above | 12 (75%) | |||
| Note: Kgs: Kilograms; VLBW: Very low birth weight; MLBW: Moderate low birth weight; Cms: Centimeter | ||||
Table 1: Baseline characteristics of the 16 mother-infant dyad in the study.
Pre and post intervention PDMS-2 standard score, quotient score and relative increase: Pre and post-intervention PDMS-2 standard score and quotient score of 16 infants in the study showed statistically significant results at p<0.001. Standard Scores of the gross, fine, and total motor were 5.56 ± 2.92, 4.69 ± 2.30, 10.13 ± 4.86 and for quotient score for gross, fine, and total motor scores were 9.31 ± 6.64, 8.06 ± 3.91, 10.38 ± 4.33 respectively. The average percentage of a relative increase in the standard score was 20.16%, 30.53%, 23.44%, and quotient scores were 10%, 10%, 11% for gross, fine and total motor scores, respectively. It is seen that the confidence interval in prepost overlap in all categories (Table 2).
| PDMS 2 | Factor | Time points | Mean ± SD | Change (Post-Pre) | Average % of the relative increase | P-value# |
|---|---|---|---|---|---|---|
| Standard score | Gross motor skills | Pre | 28.31 ± 2.15 | 5.56 ± 2.92 | 20.16% | <0.0001* |
| Post | 33.88 ± 2.45 | |||||
| Fine motor skills | Pre | 15.69 ± 1.62 | 4.69 ± 2.30 | 30.53% | <0.0001* | |
| Post | 20.38 ± 2.36 | |||||
| Total motor skills | Pre | 44.06 ± 3.45 | 10.13 ± 4.86 | 23.44% | <0.0001* | |
| Post | 54.19 ± 4.53 | |||||
| Quotient score | Gross motor skills | Pre | 96.5 ± 4.49 | 9.31 ± 6.64 | 9.74% | <0.0001* |
| Post | 105.81 ± 7.11 | |||||
| Fine motor skills | Pre | 85.94 ± 3.91 | 8.06 ± 3.91 | 9.57% | <0.0001* | |
| Post | 94 ± 2.19 | |||||
| Total motor skills | Pre | 91.13 ± 3.58 | 10.38 ± 4.33 | 11.44% | <0.0001* | |
| Post | 101.5 ± 5.01 | |||||
| Note: # One-tailed t-test *Level of significance (p<0.05) | ||||||
Table 2: Pre and post-intervention PDMS-2 standard score and quotient score of 16 infants in the study.
Comparison of PDMS-2 standard score and quotient score with baseline characteristics: Using one-tailed t-test, it’s been concluded that the mean gain in fine motor standard score after treatment is significantly less for very low birth weight infants (1.50 ± 0.58) when compared with moderate low birth weight infants (3.25 ± 0.97) with a p-value of 0.0009 and also for the participant with less than 32 weeks of gestation (1.67 ± 0.82) as compared to infants in the 32-37 weeks (3.50 ± 0.71) with a pvalue of 0.0016. While the Mean gain in Fine motor quotient score after treatment is significantly less for VLBW (4.50 ± 1.73) compared with moderate low birth weight infants (9.25 ± 3.72) with a p-value of 0.0025 (Table 3).
| PDMS 2 | Factor | Sub-category | Gross motor skills | Fine motor skills | Total motor skills | |||
|---|---|---|---|---|---|---|---|---|
| Gain | P-value | Gain | P-value | Gain | P-value# | |||
| Standard score | Gestational age | <32 weeks (n=6) | 5.5 ± 2.59 | 0.9498 | 1.67 ± 0.82 | 0.0016 WT | 7.17 ± 2.71 | 0.215 |
| 32-37 weeks (n=10) | 5.6 ± 3.24 | 3.50 ± 0.71 | 9.40 ± 3.63 | |||||
| Birth weight | VLBW (<1.5 kg) (n=4) | 7 ± 1.41 | 0.2699 | 1.50 ± 0.58 | 0.0009 | 8.50 ± 1.91 | 0.9679 | |
| MLBW (≥ 1.5 kg) (n=12) | 5.0 ± 3.18 | 3.25 ± 0.97 | 8.58 ± 3.85 | |||||
| Quotient | Birth weight | VLBW (<1.5 kg) (n=4) | 10.5 ± 5.80 | 0.6943 | 4.50 ± 1.73 | 0.0025 | 9.25 ± 3.77 | 0.5671 |
| MLBW (≥ 1.5 kg) (n=12) | 8.92 ± 7.09 | 9.25 ± 3.72 | 10.75 ± 4.59 | |||||
Table 3: Comparison of PDMS-2 standard score and quotient score with baseline characteristics of 16 infants in the study.
This study was designed to determine the effectiveness of the intervention on motor skill development in PLBW infants. The results showed improvement in the motor component in all the subsets of gross and fine motor skills. This is because parentinfant interaction leads to better experience, which facilitates motor development through the emergence of self-directed movements. In one study, it was examined the effect of experiencing locomotion for development in perception under a challenging environment controlled by incentives from society. When they were encouraged, crawlers tried for safe sloping within their capacity, but walkers explored risky one. When they were discouraged, they withdrew from all the activities which they had attempted. It was told that both components like motor experience and social incentives were impactful in improving postural control, responsible for balance and locomotion [10].
Another study aimed at various early experiences for the advancement of the development of future related skills maintenance by position and proper handling. Multiple advance activity was taught to caregiver and long-term changes were seen in preterm infants. The activities were enriched perceptual experiences which promote abilities including strength, postural control, and midline hand activity. These activities facilitated mother infant bonding. The observed changes in infants’ abilities most likely resulted from an interaction between infants’ abilities and in caregivers-infant interactions. Due to early movement experience neuromuscular systems prepared better for action. For execution of those movements required antigravity muscle action. Handling and positioning enhance proper neuronal connection and improve perceptual motor ability. Parent delivered early movement experience accelerated all these processes and helped in advancement of activity [11].
It was also noticed that improvement of the Fine Motor Quotient (FMQ) was more in MLBW infants. The standard score of the fine motor is also dependent on Gestational Age (GA) and Low Birth Weight (LBW). Standard score of the fine motor was less in VPLW. This is probably due to shorter gestational age or lower birth weight, and these factors have a negative impact on motor outcome.
A home-based parent-training early intervention was done to optimize development and child-parent interaction for preterm infants (GA<37 weeks, BW<2500 gm) born to teenage mother (<19 year) who completed 10th class. Outcome measures like the mother’s assessment of the behavior of her infant (MABI), the Maternal Developmental Expectation and Childrearing Attitude Survey (MDECAS), Carey Infant Temperament were taken. Developmental items from Bayley, Brazelton and Denver scales were taken as intervention. Different sets of sensorimotor exercise were given at 1 month, 2-4 month and 4-8 month. Growth and interaction were improved but minimum development was seen in motor skills [12].
Study was conducted on early movement training by parents on advanced feet reaching for the preterm infant at two months corrected age. In this 8-week protocol at the 2nd and 4th month of life assessment through video recording were done. After completion of this protocol toy-foot, contact time increased in the intervention group [13].
A study was done on PLBW infants (GA<37 weeks, BW<2000 grams) at corrected age of 4 months. Early Home Intervention was given to increase parents’ reaction and feelings to the infant’s requirement and behavior that would help in both environmental enrichment and development. Result demonstrates changes in behavior and improvement in cognitive development. No motor development was seen, which is in contrast to our study [14].
An early intervention was done for promoting child’ motor development and also to emphasize short-long-term parentchildren bonding by delivering guideline of physiotherapy to parents. Preterm infants (GA ≤ 32 weeks) were assessed with standardized tests like TIMPSI, PDMS-2, GMA, TIMP. Intervention for 10 minutes twice a day/3 week enhanced the infants’ motor outcome in 2nd year of CA. Unlike our protocol it showed long term effect of early intervention in motor development [15].
An early intervention, supporting play exploration and early development (SPEEDI) were applied for preterm infant (<30 week GA), 10 therapy session program were done. Higher score was shown in gross motor, receptive and expressive language at 4 month’s corrected age [16].
Same protocol as present study was done on two late preterm infants (34–36 weeks of gestation) who took treatment from 15 to 60 days of corrected age. Assessments of Gross and fine motor assessments were done by TIMP (Test of Infant Motor Performance) and Bayley. This protocol was well accepted by family and positive finding were seen in developmental outcome.
But in this present study where parent delivered early movement experience done on preterm and low birth weight infant at corrected age 1-2 month on motor skill development show effective result in PDMS-2 gross, fine and total motor development. Though the CI was overlapping in all the categories, this could be due to sampling error.
Various parent delivered early intervention like (MITP), (MMITP), and (IHDP) does not have direct effect on motor skill development. It was also proved that NIDCAP also not so effective on motor development [17].
It is highlighted in recent evidence that abnormalities or birth insult are not the only components for affected brain development in fact, modulation in environment and episode of positive input may change brain development and improve overall development in infants at risk for disorder. So the early intervention is essential or development [18-20].
In this present scenario were exposing the infants to receive different developmental therapies to avoid future delays could be risky at the same time, Parents' efficiently learning the intervention and delivering it to their infants might have a multidimensional effect on a child's development. Because the study design was experimental pre-post, we were not able to attribute the observed difference to the intervention alone. But the intervention is a home Program, cost effective and affordable that would improve motor development in preterm low birth weight infants and also have an effect on parent-child bonding which enhances self-derived movement.
The present study concludes that six weeks P-EME at home has a strong influence on motor skill development in preterm low birth weight infants. Preterm low birth weight infants were more likely to have poor fine motor development and signifies inculcation of interventions to enhance fine motor development. Also provides information to physical therapy professionals involved in the multidisciplinary care of high-risk infants in lower middle-income countries that involving parents in an early development program can aid in child development.
We acknowledge all the parents and their infants for participating in the study and KLE Dr. Prabhakar Kore hospital and Medical Research Centre for providing the infrastructure to conduct the study.
The authors report there are no competing interests to declare.
Outlined in authorship disclosure form.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Data will be provided on request to the corresponding author.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Deshpande V (2025) Effectiveness of Parent Delivered Early Movement Experience on Motor Skill Development in Preterm Low Birth Weight Infants: An Experimental Pre-Post Study. Clin Pediatr. 10:306.
Received: 25-Oct-2023, Manuscript No. CPOA-23-27781; Editor assigned: 27-Oct-2023, Pre QC No. CPOA-23-27781 (PQ); Reviewed: 10-Nov-2023, QC No. CPOA-23-27781; Revised: 06-Jun-2025, Manuscript No. CPOA-23-27781 (R); Published: 13-Jun-2025 , DOI: 10.35248/2572-0775.25.10.306
Copyright: © 2025 Deshpande V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.