
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2017) Volume 8, Issue 7
Background: Laryngeal carcinoma occupies the space of glottis. It may lead to difficult airway, and is prone to bleed if intubated with endotracheal tube (ETI). Intubation can also result in the possibility of tumor cultivation in the lung. Use of laryngeal mask airway (LMA) could avoid the disadvantages of endotracheal intubation, which would benefit patients undergoing partial laryngectomy.
Methods: This was a randomized controlled clinical trial. Thirty adult patients scheduled to receive partial laryngectomy were enrolled. All study subjects received an ASA rating of grade III. Subjects were randomly assigned to the LMA group or the ETI group. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse oxygen saturation (SpO2), tidal volume and end tidal CO2 were recorded at 6 to 8 time points throughout the procedure. Arterial blood gas was analyzed at the time of tracheotomy and the same time interval after tracheotomy. Comparison analysis was performed using the Student’s t-test for continuous variables.
Results: ETI and LMA both provided satisfactory ventilation, and there was no significant difference in time to tracheotomy time between the two groups. Arterial blood gas analysis showed no significant differences in pH, PCO2, PO2, SaO2, BE, or HCO3- between the two groups. Significant differences were observed regarding hemodynamics, however; immediately after intubation, HR, SBP and HBP were significantly lower in the LMA group than in the ETI group (74.47 ± 11.77 vs. 84.67 ± 14.23, 99.67 ± 9.21 vs. 137.53 ± 35.50, 61.20 ± 8.10 vs. 82.53 ± 22.48, respectively). Five minutes after intubation SBP was still significantly lower in the LMA group (94.00 ± 11.28 vs. 110.53 ± 24.61).
Conclusions: Ventilation with LMA in partial laryngectomy was as effective as ETI, and hemodynamics were more stable in the LMA group compared with the ETI group.
Keywords: Endotracheal intubation; Laryngeal mask; Laryngeal mask airway; Laryngectomy; Laryngeal cancer
Laryngeal carcinoma accounts for 1.9% of cancers worldwide. Most of these are diagnosed in the early stages (T1N0M0 and T2N0M0). A larynx preserving operation is preferable, and open partial horizontal laryngectomy is a function-sparing surgical technique used to treat laryngeal carcinoma [1]. In order to reduce patient suffering, head and neck surgeons generally perform laryngectomy after general anesthesia with endotracheal intubation instead of tracheotomy before laryngectomy [2]. Endotracheal intubation can be challenging in laryngeal carcinoma patients. Laryngeal carcinoma tissue can fill the glottis space, often leading to difficult airway. Laryngeal carcinoma tissue is also prone to bleed [3]. Most importantly, intubation in laryngeal carcinoma patients can lead to tumor cultivation in the lungs [4]. The disadvantages of endotracheal intubation might be avoided by using laryngeal mask airway as an alternative ventilation method during anesthesia and surgery.
According to the Royal College of Anaesthetists Fourth National Audit Project (NAP4), laryngeal mask airway has become the primary airway management device for general anesthesia in the UK (56.2%) [5]. In addition to avoiding disadvantages of intubation associated with laryngeal carcinoma, ventilation with laryngeal mask airway was observed to have three general advantages over the tracheal tube: lower incidence of cough during emergence, lower incidence of postoperative sore throat and lower incidence of postoperative vomiting [6]. In addition, laryngeal mask airway intubation was accomplished in less time and with less force than McCoy and Macintosh laryngoscope intubation in a manikin study [7].
Laryngeal mask airway plays an important role in management of difficult airway, as discussed in the recent guidelines from the Difficult Airway Society [8]. It has been used successfully during surgery to remove a supra-stoma granuloma [9] and during fiberoptic bronchoscopy to remove a bronchial tumor [10].
In this study we compare hemodynamic and ventilation parameters in patients undergoing partial laryngectomy with endotracheal intubation or with laryngeal mask airway.
Study design and study subjects
This was a randomized controlled clinical trial (ChiCTRIPR- 16007903). The research protocol was approved by the ethics committee for human studies at the Fudan University Eye, Ear, Nose and Throat Hospital. Personal informed consents were obtained from all study subjects. The sample size was calculated using the following formulas:
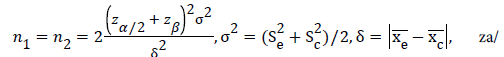
2=z0.05/2=1.96,zß=z0.2=0.84. Base on our clinical experience and reference of previous study, we hypothesize that δ should be greater than 10 mmHg of systolic blood pressure (SBP), and σ was about 7 mmHg, to reach a clinical significance [11]. Therefore, we calculated that 11 patients would provide 80% power at the 5% (two-tailed) significance level to identify this treatment effect. We recruited 30 adult patients rating as grade III by American Society of Anesthesiologists (ASA) diagnosed with glottic laryngeal carcinoma T1N0M0 or T2N0M0, aged 44-71 years, body mass index (BMI) 18-26, undergoing partial laryngectomy and receiving general anesthesia to this study. Patients with bronchial pulmonary and cardiovascular diseases were excluded. General clinical characteristics including gender, age, height, body weight and medical history were recorded.
Study subjects were randomly assigned to the laryngeal mask (LMA) group or the endotracheal intubation (ETI) group, with 15 subjects in each group, based on random numbers generated by Microsoft Office Excel (Microsoft Corp, Redmond, WA, USA).
Intubation and monitoring of subjects
One minute after anesthesia induction with 0.04 mg/kg midazolam, 2.5-3 mg/kg propofol, 0.2–0.4 μg/kg sufentanil and 0.6 mg/kg rocuronium, a flexible LMA (Teleflex, Morrisville, NC, USA) or reinforced tracheal tube (Mallinckrodt Medical, Athlone, Ireland) was inserted by anesthesia providers with a minimum of four years endotracheal intubation experience (Figures 1B and 1C). Mechanical ventilation was provided with a Primus anesthetic machine (Dräger, Lübeck, Germany).
Ventilation parameters were as follows: pressure ventilation mode, ventilation pressure: 12, respiratory rate: 12, oxygen concentration: 50%. Anesthesia was maintained with sevoflurane at the depth of 1.3 minimum alveolar concentration. Heart rate (HR), SBP, diastolic blood pressure (DBP) and pulse oxygen saturation (SPO2) were recorded before induction, after induction, immediately after intubation, and 5 and 10 minutes after intubation, immediately after tracheotomy, 5 minutes and 10 minutes after tracheotomy. Tidal volume (TV) and end tidal CO2 (ETCO2) were measured immediately after intubation, and 5 and 10 minutes after intubation, immediately after tracheotomy, 5 minutes and 10 minutes after tracheotomy. Arterial blood gas was analyzed with a ABL80 FLEX blood gas analyser (Radiometer, Copenhagen, Denmark) for pH, partial pressure of oxygen (PO2), partial pressure of CO2 (PCO2), oxygen saturation (SaO2), base excess (BE) and bicarbonate (HCO3- ) at the time of tracheotomy and after tracheotomy at a time interval equal to the time from intubation to tracheotomy (Figure 1A).
Figure 1: Study design. (A) Schematic showing data collection time line. (B) Preoperative fibrolaryngoscope of a subject suffered from glottic laryngeal cancer (white arrow). (C) Laryngoscope photo of a patient ventilated with laryngeal mask airway. White arrow indicates tumor tissue, black arrow indicates the grille of laryngeal mask airway. (D) Laryngoscope photo of a patient ventilated with endotracheal tube. White arrow indicates tumor tissue, black arrow indicates the endotracheal tube.
Statistical analysis
Continuous data were expressed as means (standard deviations, SDs). Comparison analysis was performed using the Student’s t-test for continuous variables and Chi-square for categorical data. Statistical analyses were performed using statistical software Statistical Product and Service Solutions (SPSS) (version 20.0, IBM Corp., Armonk, NY, USA). The level of statistical significance was P<0.05, and P<0.001 was considered to be very significant.
A total of 30 eligible patients (29 male, 1 female) were included in this study. No patients were excluded from the study. Demographic characteristics of study subjects are shown in Table 1. There were no significant differences between the ETI and LMA groups in terms of gender, age, height, body weight or BMI.
Ventilation was satisfactory in both groups, based on blood gas analysis and ventilation parameters, and no hypoxia occurred during the operation in either groups. No significant differences in arterial blood pH, PCO2, PO2, SaO2, BE or HCO3- were observed between the two groups (Table 1). SpO2, TV and ETCO2 did not differ significantly between the two groups at any time point. SpO2 was >95% in both groups at every time point (Figure 2 and Table 2).
| Time points | Properties | ETI group (n=15) | LMA group (n=15) | ETI vs. LMA |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | P value | ||
| Gender | 14 M / 1 F | 15M | 1 | |
| Age | 57.87 ± 8.04 | 60.53 ± 6.67 | 0.33 | |
| Height | 170.07 ± 4.98 | 168.07 ± 6.10 | 0.33 | |
| Body weight | 64.33 ± 3.83 | 64.20 ± 4.80 | 0.93 | |
| BMI | 22.26 ± 1.38 | 22.75 ± 1.63 | 0.39 | |
| Before tracheotomy | pH | 7.35 ± 0.05 | 7.33 ± 0.04 | 0.35 |
| PCO2 | 47.62 ± 5.13 | 49.50 ± 5.77 | 0.35 | |
| PO2 | 149.47 ± 54.86 | 121.80 ± 29.19 | 0.1 | |
| SaO2 | 98.64 ± 1.32 | 98.17 ± 4.83 | 0.72 | |
| BE | -0.55 ± 1.48 | -0.71 ± 0.92 | 0.71 | |
| HCO3- | 25.16 ± 1.29 | 25.24 ± 1.06 | 0.85 | |
| After tracheotomy | pH | 7.36 ± 0.04 | 7.35 ± 0.04 | 0.46 |
| PCO2 | 45.52 ± 5.07 | 47.65 ± 5.32 | 0.27 | |
| PO2 | 160.67 ± 40.07 | 150.60 ± 48.27 | 0.54 | |
| SaO2 | 99.69 ± 0.32 | 99.36 ± 1.03 | 0.24 | |
| BE | -0.37 ± 1.57 | -0.51 ± 0.97 | 0.76 | |
| HCO3- | 25.01 ± 1.21 | 25.13 ± 1.22 | 0.79 |
Gender was analyzed using Chi square test. pH, PCO2, PO2, SaO2, BE and HCO3- are expressed as means ± SDs and were analyzed using the Student’s t-test. M: Male; F: Female; PO2: Partial pressure of oxygen; PCO2: Partial pressure of CO2; SaO2: Oxygen Saturation, BE: Base Excess; HCO3-: Bicarbonate.
Table 1: Demographic characteristics and arterial blood gas analysis.
Figure 2: Trends in change of hemodynamic and ventilation parameters. Measurements were recorded before induction, after induction, after intubation, 5 min after intubation, 10 min after intubation, tracheotomy, 5 min after tracheotomy and 10 min after tracheotomy. Hemodynamic parameters HR, SBP and DBP fluctuated significantly in group ETI compared with LMA after intubation. There were no significant difference in ventilation parameters tidal volume and End-tidal CO2, and no desaturation of SpO2 in group LMA. *P<0.05, **P<0.001. Systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse oxygen saturation (SpO2).
| Time points | Properties | Group ETI (n=15) | Group LMA (n=15) | ETI vs. LMA |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | P value | ||
| Before induction | HR | 73.00 ± 14.87 | 77.07 ± 15.50 | 0.47 |
| SBP | 142.73 ± 21.60 | 140.20 ± 11.67 | 0.69 | |
| DBP | 81.87 ± 14.10 | 80.47 ± 7.63 | 0.74 | |
| SPO2 | 98.87 ± 0.92 | 98.20 ± 1.66 | 0.18 | |
| After induction | HR | 67.60 ± 9.74 | 75.07 ± 13.82 | 0.1 |
| SBP | 115.07 ± 30.78 | 119.47 ± 23.92 | 0.67 | |
| DBP | 68.67 ± 19.53 | 72.47 ± 12.82 | 0.53 | |
| SPO2 | 99.60 ± 0.63 | 99.27 ± 0.96 | 0.27 | |
| After intubation | HR | 84.67 ± 14.23 | 74.47 ± 11.77 | 0.04* |
| SBP | 137.53 ± 35.50 | 99.67 ± 9.21 | 0.00** | |
| DBP | 82.53 ± 22.48 | 61.20 ± 8.10 | 0.002* | |
| SPO2 | 99.33 ± 0.98 | 98.93 ± 1.16 | 0.32 | |
| TV | 410.47 ± 59.34 | 431.20 ± 83.04 | 0.44 | |
| ETCO2 | 38.07 ± 4.37 | 39.07 ± 3.20 | 0.48 | |
| 5 Minutes | HR | 67.13 ± 12.44 | 66.27 ± 9.66 | 0.83 |
| SBP | 110.53 ± 24.61 | 94.00 ± 11.28 | 0.02* | |
| DBP | 67.33 ± 16.57 | 57.67 ± 9.08 | 0.06 | |
| SPO2 | 99.27 ± 1.03 | 98.87 ± 1.41 | 0.38 | |
| TV | 394.67 ± 48.13 | 415.20 ± 74.80 | 0.38 | |
| ETCO2 | 37.20 ± 3.86 | 38.07 ± 4.42 | 0.57 | |
| 10 Minutes | HR | 64.73 ± 12.66 | 66.67 ± 10.51 | 0.65 |
| SBP | 107.80 ± 17.05 | 100.20 ± 15.55 | 0.21 | |
| DBP | 65.27 ± 9.11 | 62.80 ± 12.47 | 0.54 | |
| SPO2 | 99.07 ± 1.22 | 99.07 ± 1.16 | 1 | |
| TV | 387.93 ± 47.46 | 410.93 ± 52.92 | 0.22 | |
| ETCO2 | 37.07 ± 3.95 | 39.00 ± 6.06 | 0.31 | |
| Tracheotomy time | 13.80 ± 2.46 | 13.87 ± 3.23 | 0.95 | |
| Immediately after tracheotomy | HR | 78.87 ± 12.49 | 87.67 ± 15.20 | 0.09 |
| SBP | 112.47 ± 13.12 | 116.93 ± 19.70 | 0.47 | |
| DBP | 69.53 ± 10.23 | 73.73 ± 13.35 | 0.34 | |
| SPO2 | 97.40 ± 3.18 | 97.07 ± 4.32 | 0.81 | |
| TV | 398.87 ± 65.74 | 430.27 ± 84.32 | 0.27 | |
| ETCO2 | 40.13 ± 5.34 | 42.27 ± 5.73 | 0.3 | |
| 5 Minutes | HR | 66.33 ± 11.51 | 75.07 ± 12.00 | 0.05 |
| SBP | 104.13 ± 13.15 | 106.53 ± 16.13 | 0.66 | |
| DBP | 63.47 ± 11.47 | 68.07 ± 13.16 | 0.32 | |
| SPO2 | 98.53 ± 2.00 | 98.73 ± 1.22 | 0.74 | |
| TV | 403.67 ± 80.39 | 422.80 ± 55.68 | 0.46 | |
| ETCO2 | 38.60 ± 5.26 | 38.07 ± 4.22 | 0.76 | |
| 10 Minutes | HR | 67.67 ± 11.62 | 71.87 ± 11.37 | 0.33 |
| SBP | 101.73 ± 16.01 | 113.20 ± 17.90 | 0.08 | |
| DBP | 62.67 ± 13.21 | 69.40 ± 11.19 | 0.14 | |
| SPO2 | 98.93 ± 1.10 | 98.73 ± 1.03 | 0.61 | |
| TV | 393.27 ± 82.60 | 425.47 ± 74.45 | 0.27 | |
| ETCO2 | 37.27 ± 4.98 | 38.27 ± 5.15 | 0.59 |
Data are shown as means ± SDs. Comparison analysis was performed using the Student’s t-test*P<0.05, **P<0.001. HR: Heart Rate; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; SpO2: Pulse Oxygen Saturation; TV: Tidal Volume; ETCO2: End Tidal CO2.
Table 2: Hemodynamics and ventilation.
The time to tracheotomy did not differ significantly between the two groups (13.80 ± 2.46 min for ETI group vs. 13.87 ± 3.23 min for LMA group). However, hemodynamics following intubation were more stable in the LMA group compared to the ETI group. Immediately after intubation, heart rate and blood pressure (both systolic and diastolic) were significantly lower in the LMA group than in the ETI group (74.47 ± 11.77 vs. 84.67 ± 14.23, 99.67 ± 9.21 vs. 137.53 ± 35.50, 61.20 ± 8.10 vs. 82.53 ± 22.48, respectively) (Table 2). Five minutes after intubation SBP was still significantly lower in the LMA group (94.00 ± 11.28 vs. 110.53 ± 24.61). At 10 minutes after intubation there were no significant differences in hemodynamics, and no significant differences in hemodynamics were observed at any later time points (Figure 2).
The use of laryngeal mask airway has become more common due to the advantages it presents compared to endotracheal intubation, particularly in patients with difficult airways. Otolaryngologists often have to face difficult airways [12], which pose challenges to anesthesiologists as well. In a survey of Canadian anesthesiologists' preferences in difficult intubation and "cannot intubate, cannot ventilate" situations, 21% chose laryngeal mask airway device [13]. A case was reported in which tracheal intubation was performed by using i-gel® laryngeal mask airway and a lightwand in a patient with difficult airway, allowing the safe induction of anesthesia in a situation where fiberoptic bronchoscopy was not feasible [14]. The NAP4 report stressed that placement of a supraglottic airway device such as LMA should be an early decision, and that attempts at laryngoscopy should be abandoned after four or fewer attempts [15].
In this study there were no significant differences in ventilation, as determined by blood gas analysis, SpO2 readings and TV and ETCO2 measurements, with laryngeal mask airway compared to endotracheal intubation, indicating that LMA performs as well as ETI in ventilation. LMA performed better than ETI in terms of hemodynamics following intubation. LMA also has the potential advantage of minimizing the possibility of tumor cultivation in the lung. Despite small number patients was recruited in this study, the sample size calculations were determined from previous reports and our clinical estimation, and statistical analysis showed ventilation with LMA was non-inferiority with ETI according to tidal volume, ETCO2, SPO2 and arterial blood gas analysis, while hemodynamic parameters HR, SBP (δ up to 37 mmHg) and DBP were more stable as responsing to intubation. Future studies with larger sample sizes and long term follow-up will be necessary to evaluate the effects of LMA versus ETI on tumor metastasis.
Since LMA is still a relatively new approach to ventilation, anesthesiologists must take care to inform otolaryngologists when LMA is in use. The laryngeal mask may be mistaken for tumor or lymph node tissue if the surgeon is not informed [16].
In conclusion, we found that ventilation with laryngeal mask airway in partial laryngectomy was effective, and hemodynamics were more stable compared with endotracheal intubation. Thus the use of laryngeal mask airway is beneficial for patients undergoing partial laryngectomy.
Thank Dingding Wang (Department of Anesthesiology, Eye, Ear, Nose and Throat Hospital, Fudan University, Shanghai 200031, China) for photographing the laryngoscope pictures. This study was supported by the Shanghai Municipal Science and Technology Commission Medical Guide Project (14411969700).
The authors state no potential conflicts of interest.