Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2022)Volume 7, Issue 3
Kawasaki Disease (KD) is an inflammatory vacuities present primarily in pediatric patients; it is the leading cause of acquired heart disease in children of developed countries. The cause of KD is unknown but is presumed to be of infectious etiology. In this case, we report a 2-year-old female patient with a clinical diagnosis of KD who also has high levels of Epstein–Barr Virus (EBV) IgG and IgM antibodies. Many reported cases of KD have overlapping clinical symptoms with EBV. Interestingly, this patient also has false positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) IgM antibodies in the era of the COVID-19 pandemic. In this case report, we seek to discuss the significance of positive EBV antibodies and false positive SARS-CoV-2 IgM antibodies in the era of COVID-19 in a pediatric patient with a concomitant diagnosis of KD. We document this case to contribute to further understanding the relationship between EBV and KD with EBV as a possible trigger in a pediatric patient who also meets clinical criteria for Multisystem Inflammatory Syndrome in Children (MIS-C) during the COVID-19 pandemic.
Kawasaki disease; Pediatrics; SARS-CoV-2; Epstein–Barr Virus
Kawasaki Disease (KD) (aka mucocutaneous lymph node syndrome) is a multi-organ inflammatory vasculitis affecting mainly pediatric patients. Incidence of disease is highest in children living in East Asia or who are from Asian ancestry. In the United States, the incidence of Kawasaki Disease is estimated to be 20 per 100,000 annually for children under 5 years of age [1]. This vasculitis is a clinical diagnosis KD diagnostic criteria include continuous fever over five days and four out of the five classic physical examinatio findings; conjunctival injection, changes to the oral mucous membranes (red/fissured lips,lip fissures/ strawberry tongue), swollen peripheral extremities, polymorphous rash, and cervical lymphadenopathy [2]. The mainstay of treatment is Intravenous Immunoglobulin (IVIG) and high dose Acetylsalicylic Acid (ASA). In this case report, we present a patient with clinical Kawasaki Disease whose laboratory findings show high levels of Epstein-Barr Virus (EBV) IgG and IgM and was reported to have a false positive SARS-CoV-2 IgM in the age of the COVID-19 virus.
Many reported cases of Kawasaki disease have overlapping symptoms with EBV, and during the COVID-19 pandemic, there are also many overlapping symptoms with a new pediatric COVID-19 disease termed Multi-system Inflammatory Syndrome in Children (MIS-C).
As of today, there is no single known trigger for the development of Kawasaki Disease. Studies have reported an array of possible triggers including infectious, environmental, and immunologic etiologies. One theory states that Kawasaki Disease may represent a final common pathway of immune-mediated vascular inflammation following a variety of inciting infections and/or environmental antigens [3]. This brief report intends to describe EBV as a possible trigger for the development of Kawasaki Disease in a pediatric patient who also meets clinical criteria for MIS-C during the COVID-19 pandemic.
A 2-year-old female is brought to the emergency department with a 5-day history of fever, cough, and sore throat. The fever has been presented daily and unremitting despite antipyretic therapy. She has been irritable with decreased oral intake. On laboratory evaluation, a urinalysis revealed trace protein and elevated White Blood Cell (WBC) count. She was sent home with a prescription for Cephalexin with a diagnosis of urinary tract infection.
The subsequent day, she returns to the emergency department with her mother who states she now has increased oral secretions and is unable to swallow. Her fever persists despite the antibiotic therapy. On examination, she is febrile to 101.2° (rectal thermometer) and tachycardic at 152 beats/minute. On physical examination she has significant nasal congestion, conjunctival erythema, lip fissures, a skin rash consistent with red patches on her abdomen and back,and bilateral anterior cervical lymph node enlargement (Figure 1a-1c).
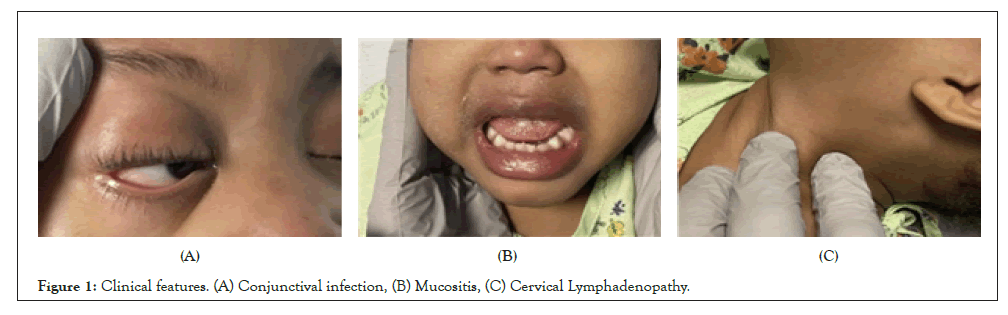
Figure 1: Clinical features. (A) Conjunctival infection, (B) Mucositis, (C) Cervical Lymphadenopathy.
Labs ordered at that time showed an elevated C - Reactive Protein (CRP), normal WBC, and urinalysis positive for protein and ketones (suggesting dehydration). A Computed Tomography (CT) scan of the neck with contrast revealed retropharyngeal edema, tonsillar hypertrophy, and lymphadenopathy (Figure 2). She was admitted to the pediatric floor with fever of unknown origin for further evaluation and management. Echocardiography showed normal function and anatomy (Figure 3).
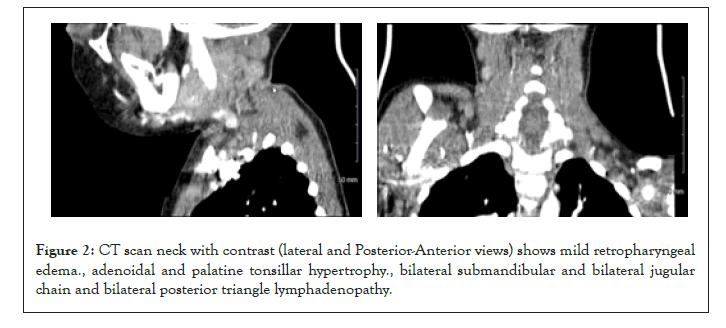
Figure 2: CT scan neck with contrast (lateral and Posterior-Anterior views) shows mild retropharyngeal edema., adenoidal and palatine tonsillar hypertrophy., bilateral submandibular and bilateral jugular chain and bilateral posterior triangle lymphadenopathy.
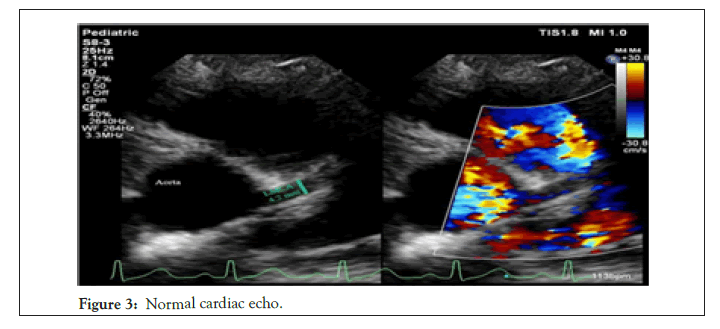
Figure 3: Normal cardiac echo.
During the patient's hospital stay, she completed empiric antibiotic treatment with Ceftriaxone and Clindamycin. Full laboratory workup including viral respiratory panel, mycoplasma IGM, and EBV antibodies were completed. Because of the medical climate during the age of the COVID-19 pandemic, we ordered a SARSCoV- 2 IgG and IgM serum test. The initial SARS-Cov-2 IgM came back with positive results and the IgG was negative. On repeat serum tests done the same day, she was negative for both SARSCov- 2 IgM and IgG. Sedimentation rate (ESR) was elevated, along with elevations in lactate dehydrogenase and D-Dimer. EBV IgM, IgG and nuclear antigen/antibody resulted with an extremely high positive value.
On hospitalization day 2 (day 7 of fever), KD diagnosis was made clinically after meeting all criteria IVIG and ASA treatments began at that time. The major clinical criteria for the Kawasaki Disease scoring system include fever duration, conjunctivitis, mucous membranes, lymph node enlargement, presence of a rash, and hands/feet involvement. Additional clinical criteria include values of ESR/CRP, albumin, and platelets, age of patient, and hydrops of gallbladder. If the total score is greater than or equal to 9, the diagnosis is consistent with Kawasaki Disease, and the patient should be managed accordingly. In our patient, she had fever duration longer than 5 days (3 points), conjunctivitis (2 points), red and fissured lips (3 points), and a CRP level greater than 2.5 (1 point) for a total of 9 points. She responded very well to the IVIG, and her fever began to decrease.
Her initial cardiac echocardiogram was inconclusive; a subsequent echocardiogram was then performed. Based on the coronary artery measurements discovered, there is no enlargement of the coronary arteries, as commonly seen with Kawasaki Disease. The most common arteries involved are the Right Coronary Artery (RCA) and Left Anterior Descending (LAD) artery. Any Z-score greater than or equal to 2 should be followed with serial echocardiography, as it can signify arterial dilatation (Figure 3 and Table 1) [4].
| Location | Measurement | Mean | Range | Z-Score |
|---|---|---|---|---|
| LMCA(mm) | 1.7 | 2.26 | 1.62-2.89 | -1.44 |
| LAD(mm) | 1.5 | 1.78 | 1.36-2.20 | -1.11 |
| RCA(mm) | 1.3 | 1.77 | 1.23-2.31 | -1.43 |
Note: A coronary artery with a Z score between +2.5 and +5.0 is considered a small aneurysm. A Z score between +5.0 and +10.0 is considered a large aneurysm. Our calculated Z scores ranged -1.44 to –1.11, meaning they were all very small.
Table 1: Baseline Characteristics of Participants in the Control and Intervention Groups.
Here, we present a case of a two-year-old female who meets clinical criteria for both Kawasaki Disease and MIS-C while also being EBV positive and having a false positive SARS-CoV-2 IgM test. This is of clinical importance for multiple reasons. The first and most compelling is that this will be one of the first cases of EBV as a potential trigger of KD since it was last reported in the 1970’s [5]. The second clinical significance lies in the fact that high antibody titers, in this case highly elevated EBV IgG and IgM, may be potential triggers of false positive SARS-CoV-2 testing. Lastly, and of great importance is the treatment of the patient may differ based on the etiology. Given that the patient meets criteria for both KD and MIS-C, should treatment follow that of KD including IVIG, high dose ASA for an extended period of time, and long-term cardiology follow up or should she be treated as an MIS-C patient. During the constant evolution of the COVID-19 pandemic, it is vital that we have reliable testing. Our patient initially tested negative for SARS-CoV-2 on a Polymerase Chain Reaction (PCR) general film array, confirmation testing showed positive IgM titers and later that same day negative IgM titers. Potential causes of this false positive test include oversaturation of the PCR from extremely high EBV IgM. An article published in The Journal of Clinical Microbiology described a similar incidence with high false positive SARS-CoV-2 tests in patients with highly elevated EBV levels. Here is an excerpt from their study “This specificity issue was consistently observed in patients suffering from acute infectious conditions, especially infection with Epstein-Barr virus (EBV) or Hepatitis B Virus (HBV). This suggests that they result from nonspecific immune activation rather than cross reactivity between non SARS-Cov-2 Abs and the SARS-CoV-2 proteins used in the assay” [6].
When a patient has a clinical diagnosis that meets criteria for different diseases, it can be difficult to determine how to treat the patient. Initial standard of care treatment of KD includes IVIG 2 g/kg and high dose ASA 80-100 mg/kg/day.. At the time of this patient's presentation, there was no standard of care treatment for MIS-C, and all management guidelines were driven from those used to treat KD.
With our patient, she was given IVIG, of note, no coronary changes were found but that can be a late finding and resolved with the initial IVIG treatment. Given the severity of patient symptoms and new evolution of MIS-C, our patient was treated as if KD was sole infection.
Kawasaki disease has no distinct etiology as there are many possible triggers including infectious, environmental, and immunologic causes. EBV is one common trigger along with other viral, bacterial and fungal infections that can cause a significant inflammatory reaction to trigger a Kawasaki disease clinical picture. In the age of the COVID-19 pandemic caused by SARS-CoV-2, reliable testing is of the greatest importance. Here, we show the possibility of very high infectious disease titers causing a false positive SARS-CoV-2 test. With many overlapping clinical symptoms between EBV, Kawasaki disease, and MIS-C, it is important to evaluate with accurate laboratory results to determine the most common etiology for the patient presentation which can alter the treatment course.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Sahhar HS, Basch RE, Downes K (2022) EBV Positive Kawasaki Disease with False Positive SARS Antibodies in the Age of COVID-19 Pandemic. Clin Pediatr. 7:208.
Received: 02-May-2022, Manuscript No. CPOA-22-16561; Editor assigned: 04-May-2022, Pre QC No. CPOA-22-16561 (PQ); Reviewed: 19-May-2022, QC No. CPOA-22-16561 ; Revised: 23-May-2022, Manuscript No. CPOA-22-16561 (R); Published: 02-Jun-2022 , DOI: DOI: 10.35248/2572-0775.22.7.208
Copyright: © 2022 Sahhar HS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.