International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2020)Volume 8, Issue 3
Early rehabilitation methods, including postural changes and respiratory physical therapies, have been shown to prevent pulmonary complications; however, strategies to prevent pulmonary complications in sepsis patients remain poorly defined. This clinical study was to evaluated if early rehabilitation provided by specialized physical therapist in an emergency center could reduce respiratory complications in sepsis patients.
We evaluated sepsis patients for demographic characteristics, the number of days until rehabilitation, and the incidence of pulmonary complications. Kaplan-Meier curves were constructed to analyze the incidence of pulmonary complications for the study sample stratified by specialized physical therapists. Cox regression analysis examined the relationship between early rehabilitation provided by specialized physical therapists and the incidence of pulmonary complications.
The number of days until rehabilitation was significantly shortened after assigning a specialized physical therapist. Assigning specialized physical therapist was significantly associated with pulmonary complications for sepsis patients and, in the multivariable model, specialized physical therapists (hazard ratio=0.34; 95%confidence interval=0.16-0.74; p=0.006) and the number of days until rehabilitation (hazard ratio=1.12; 95% confidence interval=1.08-1.19; p=0.047) were significantly associated with pulmonary complications. Early rehabilitation decreased the incidence of pulmonary complications in sepsis patients.
[University Hospital Medical Information Network Clinical Trials Registry, number UMIN000039793 (2020/3/12)].
Sepsis patients; Early rehabilitation; Pulmonary complications; Specialized physical therapist
Sepsis is defined as a powerful systemic response to severe infection. The incidence of severe sepsis is estimated to be between 50 and 100 cases per 100,000 people in developed countries [1]. Sepsis patients have significantly worse functional outcomes, particularly in the physical and cognitive domains, than age-matched normal [2] and other hospitalized patients [3]. Recently, sepsis patients in the intensive care unit (ICU) have developed post-intensive care syndrome, [4] which is classified by a declined in physical, cognitive or mental functions and ICUacquired weakness (ICU-AW), [5,6]. As a result of ICU-AW, diffuse muscle weakness may develop. In addition, respiratory complications are common manifestations of sepsis-associated organ dysfunction [7,8]. In the postoperative period, pulmonary complications following major upper abdominal surgeries increase morbidity [9] mortality [8,9] hospital stay, and medical costs [10,11]. Therefore, pulmonary complications in sepsis patients would also affect clinical outcomes and the medical economy. In the intensive care, the effectiveness of early rehabilitation methods, including postural changes and respiratory physical therapy, has been shown to prevent pulmonary complications, including pneumonia and atelectasis [12-15]. Therefore, many previous studies include patients with postoperative and acute lung injury, patients who are in intensive care or on ventilators; disease specificity among patients is inferior due to the wide variety of diseases. In 2018, a randomized controlled trial reported a rehabilitation intervention that was limited to sepsis patients [16]. Since the contents of rehabilitation were also limited in this report, strategies to prevent pulmonary complications in patients with sepsis remain poorly defined. We have already treated patients based on the Awakening and Breathing Coordination, Delirium monitoring/ management, and Early exercise/mobility bundle [17]. In addition, in the 2017 fiscal year, specialized physical therapist was staffed at the advanced emergency critical care center (AECCC) as a part of the early rehabilitation.
We hypothesized that early rehabilitation for sepsis patients would reduce the incidence of pulmonary complications. The purpose of this clinical study was to evaluate if early rehabilitation provided by specialized physical therapist in the emergency center could reduce respiratory complication in sepsis patients who required intensive care or had worsening complications.
This study was a retrospective cohort study. Regarding bias, the outcome assessors and researchers were blinded.
Ethical approval
The study protocol was approved by the Ethics Committee of Shinshu University (No,4161), and we obtained written informed consent from all participants after the study protocol was explained in detail. However, an opt-out format was adopted for participants who could not be contacted. This study was registered with University Hospital Medical Information Network Clinical Trials Registry, number UMIN000039793 (2020/3/12). This study was conducted in accordance with the standards set forth by the latest revision of the Declaration of Helsinki.
Patients
The subjects of this study were sepsis patients who entered the AECCC of Shinshu University Hospital between April 2014 and March 2018. Participants ≥ 18 years who received intensive treatment and were diagnosed with sepsis [18] (≥ 2 criteria of a systemic inflammatory response plus proven or strongly suspected infection), sepsis (sepsis plus organ failure) or septic shock (sepsis with hypotension and unresponsive to fluid management) and who met the inclusion criteria were enrolled. Patients with head injuries, burns, spinal injuries, lower limbs with multiple fractures, and those with septic shock who were unresponsive to maximal treatment, moribund or had an expected mortality within 24 h were excluded. Participant age, sex, body mass index, sequential organ failure assessment score, [19] systemic inflammatory response syndrome score, [20] disseminated intravascular coagulation score, laboratory data, primary source of infection, use of therapeutic medication, use of mechanical ventilation, length of hospital stay, the number of days until rehabilitation was achieved, the baseline Barthel index [21,22] and the incidence of pulmonary complications were recorded.
Participants in the intervention arm underwent an individualized and early-targeted physical rehabilitation program prescribed by the AECCC research physical therapist within 48 h of the diagnosis of sepsis. The program ran once or twice daily, for 20-40 min, until discharge from the AECCC. This physical rehabilitation program included pulmonary rehabilitation (deep breathing, periodic non-invasive ventilation and supported cough), passive range of motion, active and passive ranges of motion in both the upper and lower extremities, sitting out of bed, transfers, electrical muscle stimulation (General Therapeutic electrical Stimulator; Homer Ion co.itd), ambulation, and other mobilization techniques, as appropriate. Participants in both groups received standard AECCC care, which included the physical therapy program provided by specialized physical therapist at the AECCC. The physical rehabilitation received by both groups was recorded. Therapeutic interventions were continued on a regular basis throughout the hospital stay of the patient, until he or she returned to a previous functional or was discharged.
Safety measures
Recently published literature included falls to the knees, endotracheal tube removal, systolic blood pressure more than 200 mmHg, systolic blood pressure less than 90 mmHg and desaturation less than 80% [23]. In this study, we focused on these adverse events and developed a rehabilitation program.
Primary outcomes
The primary outcome measure was the association between early mobilization by specialized physical therapy and the onset of a pulmonary complication. Pulmonary complications were diagnosed from the medical records by multiple doctors.
Sample size
Sample size calculations were conducted using the G-power 3.1 software. A sample size of 64 per group (total 128) was calculated with an effect size of 0.5 and 80% power with a type 1 error rate of 0.05 with the Bonferroni adjustment.
Statistical analyses
The patients were divided into two groups based on if they were admitted before or after assigning by specialized physical therapist. Patients admitted between April 2017 and March 2019 were admitted after assigning by specialized physical therapist, while histological control patients with sepsis were admitted from April 2014 to March 2017, before assigning by specialized physical therapist. We used the product-limit method to derive pulmonary complications. Kaplan-Meier curves were constructed to display pulmonary complications for the study sample and were stratified based on the specialized physical therapist (Log-rank test). Moreover, multivariable analysis (Cox regression analysis) of pulmonary complication was developed as the most parsimonious model. Next, as a sub analysis, we performed multivariable analysis (Cox regression analysis), which included the number of days until rehabilitation was achieved as an analysis item. All statistical tests assumed unequal variance with a p value<0.05 considered statistically significant. All analyses were performed using the EZR statistical program [24]. Descriptive statistics (mean ± standard deviation, or median [25%,75].) were calculated.
In total, 153 patients (68%) were recruited; 93 patients were recruited between April 2014 and March 2017, while 60 patients were recruited between April 2017 and March 2019 group (Figure 1). Forty-five pulmonary complications (10 pneumonia, 23 atelectasis, 12 respiratory failures, including pulmonary edema and acute respiratory distress syndrome) were observed in this study (complication rate=29.4%).
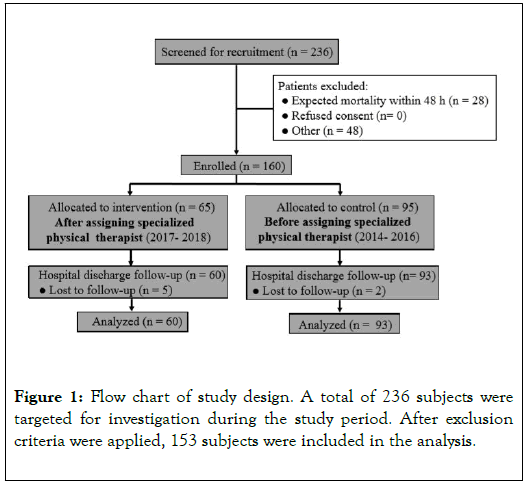
Figure 1. Flow chart of study design. A total of 236 subjects were targeted for investigation during the study period. After exclusion criteria were applied, 153 subjects were included in the analysis.
Adherence
There were no withdrawals during the conduct of the trial. All participants adhered and remained enrolled in the study for an average of 35 days.
Safety measures
There were no adverse events related to rehabilitation observed in this study.
Vital signs
As a further measure of safety, arterial blood pressure, heart rate, respiratory rate and oxygen saturation were monitored during all sessions of exercise. No exercise sessions resulted in an adverse event.
Procalcitonin and C-reactive protein levels
Procalcitonin and C-reactive protein levels were collected as laboratory data and as a safety marker for exercise. Adverse events in relation to procalcitonin and C-reactive protein levels did not result after exercise.
Demographics, AECCC and hospital measures
The number of days until rehabilitation was achieved was significantly shortened after specialized physical therapist compared to before specialized physical therapist was assigned (6.1 ± 3.7 days vs 2.6 ± 1.4 days, p0.001, Figure 2). The demographics of participants in the before assigning specialized physical therapist group (control group) and after assigning specialized physical therapist group (early rehabilitation group) are reported in Table 1. There were significant differences in the disseminated intravascular coagulation score, therapeutic medication, Barthel index baselineand frequency of pulmonary complications between the groups.
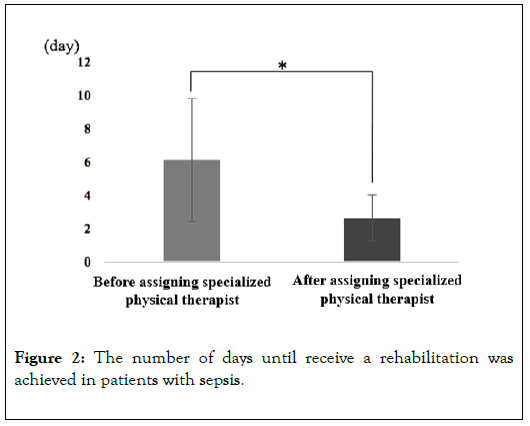
Figure 2. The number of days until receive a rehabilitation was achieved in patients with sepsis.
| Variable | Before assigning specialized physical therapist (n = 93) | After assigning specialized physical therapist (n = 60) | p-value |
|---|---|---|---|
| The number of days until rehabilitation(days) | 6.1 ± 3.7 | 2.6 ± 1.4 | p<0.001 |
| Age(yr) | 71.8 ± 13.9 | 70.3 ± 12.9 | 0.558 |
| Men/women, n(%) | 53 (57)/40(43) | 32 (53)/28(47) | 0.908 |
| BMI(kg/m2) | 21.2 ± 4.7 | 20.9 ± 3.5 | 0.72 |
| Severity score | |||
| SOFA score | 5.6 ± 3.6 | 6.6 ± 3.3 | 0.087 |
| SIRS score | 2.8 ± 1.0 | 2.7 ± 0.8 | 1.03 |
| DIC score | 1.9 ± 1.4 | 3.1 ± 2.8 | p<0.001 |
| PCT(ng/mL) | 8.1(1.6,32.3) | 17.1(3.3,58.9) | 0.064 |
| Primary source of infection | |||
| Pneumonia, n(%) | 11(12) | 8(16) | 0.487 |
| Other pulmonary disease, n(%) | 5(5) | 6(10) | 0.878 |
| Urinary tract infection,n(%) | 19(20) | 13(26) | 0.45 |
| Intra-abdominal infection,n(%) | 10(11) | 10(20) | 0.13 |
| Gastroenteritis,n(%) | 19(20) | 9(15) | 0.345 |
| Others,n(%) | 29 (31) | 14(23) | 0.09 |
| Therapeutic medication | |||
| Vasopressor,n(%) | 40(43) | 41(68) | p<0.001 |
| Steroid,n(%) | 11(12) | 24(40) | p<0.001 |
| Recomodulin,n(%) | 13(14) | 18(30) | 0.002 |
| Mechanical ventilation,n(%) | 34(37) | 21(35) | 0.903 |
| Barthel index baseline | 5(0,40) | 0(0,18.8) | 0.029 |
| Length of hospital stay(days) | 25.0(15,46) | 27.5(14.5,39.8) | 0.542 |
| Outcome | |||
| Pulmonary complications,n(%) | 35(38) | 12(20) | p<0.030 |
Data are counts (percentages), mean ± SD or median (25%,75%). Abbreviations: AECCC: Advanced Emergency Critical Care Center; BMI: Body Mass Index; SOFA, Sequential Organ Failure Assessment; SIRS: Systemic Inflammatory Response Syndrome; DIC: Disseminated Intravascular Coagulation; PCT: Procalcitonin.
Table 1: Demographic clinical characteristics in AECCC and hospital measures.
Kaplan-Meier curves
Figure 3 shows the Kaplan-Meier analyses of pulmonary complication for the study sample stratified by group. Based on this analysis, provided by specialized physical therapist was significantly associated with pulmonary complication for sepsis patients (p=0.033).
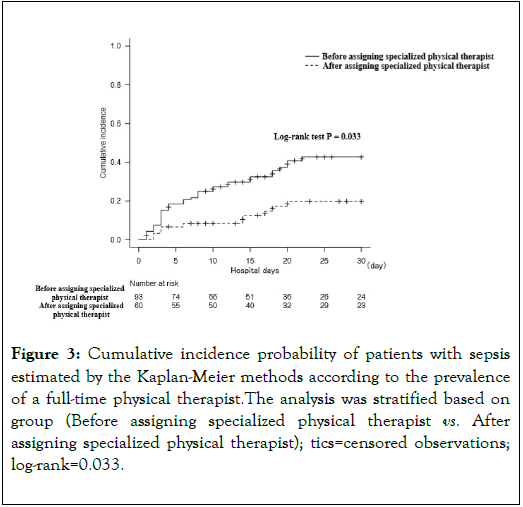
Figure 3. Cumulative incidence probability of patients with sepsis estimated by the Kaplan-Meier methods according to the prevalence of a full-time physical therapist.The analysis was stratified based on group (Before assigning specialized physical therapist vs. After assigning specialized physical therapist); tics=censored observations; log-rank=0.033.
Multivariate Cox regression analysis
Table 2 shows the Cox proportional hazard model. According to the multivariable analyses, provided by specialized physical therapist (hazard ratio=0.34; 95% confidence interval=0.16-0.74; p=0.006) and the number of days until rehabilitation was achieved (hazard ratio=1.12; 95% confidence interval=1.08-1.19; p=0.047) were significantly associated with the prevalence of pulmonary complications.
| Variable | Univariable analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| HR (95% CI) | p-value | HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Assigning specialized physical therapist | 0.48 (0.24-0.97) | 0.039 | 0.34 (0.16-0.74) | 0.006 | − | − |
| SOFA score | 1.02 (0.94-1.11) | 0.694 | 0.97 (0.89-1.07) | 0.603 | 0.99 (0.89-1.09) | 0.789 |
| The number of days until rehabilitation (days) | 1.21 (1.09-1.47) | 0.045 | − | − | 1.12 (1.08-1.19) | 0.047 |
| Vasopressor,n (%) | 1.42 (0.77-2.62) | 0.261 | 1.99 (0.93-4.30) | 0.077 | 1.52 (0.71-3.25) | 0.276 |
| Steroid,n (%) | 1.19 (0.63-2.28) | 0.591 | 1.37 (0.66-2.83) | 0.394 | 1.03 (0.50-2.10) | 0.935 |
| Barthel index baseline | 1.00 (0.99-1.02) | 0.981 | 1.00 (0.99-1.01) | 0.899 | 1.00 (0.99-1.02) | 0.896 |
Table 2: Cox proportional hazard pulmonary complications analysis.
The main finding of this study was that the incidence of pulmonary complications significantly decreased with early rehabilitation by providing specialized physical therapist in patients with sepsis. This result suggests that providing specialized physical therapist improved rehabilitation awareness in the AECCC, accelerated rehabilitation requests and the enrichment team medical care for sepsis patients. Sub-analysis of the present study revealed that the number of days until rehabilitation was achieved also contributed to the reduction of respiratory complications in patients with sepsis. To our knowledge, this is the first study to report thatearly rehabilitation by providing specialized physical therapist decreased the incidence of pulmonary complications in patients with sepsis. Many studies have not shown a difference between groups [25,26], but it can be noted that the ‘‘ standard care ’’ group had a high exercise level due to existing local practices. In our study, assigning specialized physical therapist would reduce the number of days until rehabilitation without changing the rehabilitation practices. We recognize this is as a novelty of our clinical study.
The early rehabilitation program provided in this trial (rehabilitation approximately shortened by 4 days) is a feasible treatment can be performed in typical intensive care settings. This is a versatile method for reducing the number of days until achieving rehabilitation and it is easy to adopt in many hospitals. Further, changes in vital signs during the rehabilitation program and laboratory data suggested that an early rehabilitation program can be done safely for sepsis patients who required intensive care or had worsening complications. However, in facilities that do not have an adequate amount of well-trained staff, there are concerns about the feasibility of rehabilitation in the AECCC. Early mobilization is defined as physical activity that occurs within 2-5 days of admittance to the hospital in Europe and America [27,28]. In this study, the duration of time from admission to rehabilitation intervention after assigning the specialized physical therapist was 2.6 ± 1.4 days; this length of time was significantly lower than that in the control group. Therefore, we believe that this early intervention is effective in reducing pulmonary complications in patients with sepsis.
In a previous study, early rehabilitation was important for patients with sepsis because it improved the drainage of pleural effusion and increased the lung volume via optimal distribution of ventilation to the dorsal areas of the lungs [15]. Furthermore, respiratory physiotherapy was widely performed to prevent and recover pulmonary functions after thoracic or abdominal surgery [29]. Therefore, in this clinical study, early rehabilitation by specialized physical therapist (i.e. positioning, getting out of bed, aggressive evacuation and back release) prevented atelectasis or pneumonia and the severity of these diseases.
Patients who developed postoperative pulmonary complications had a longer hospital stay [12]. We hypothesized that preventing respiratory complications would shorten the hospital stay. However, there was no significant difference in the length of hospital stay. Most likely, this is because the family environment and social background of the patients influenced their discharge decisions. The demand and importance for early and intensive rehabilitation is increasing, especially in the fields of emergency and intensive care medicine. However, in order to provide rehabilitation safely at an emergency unit or ICU, it is important to prescribe a medical intervention based on information sharing and discussion by medical staff. In addition, we believe that human resource development is also very important for developing rehabilitation at the emergency unit and ICU. Finally, to get higher quality evidence, the findings presented here require confirmation in larger, multicenter studies.
This study has limitations that should be addressed. First, this study included patients from a single center, which limits the external validity or generalizability of the study. Second, prehospital factors that predict respiratory complications, such as obesity, respiratory function, and smoking, were not considered. Lastly, the details of rehabilitation programs, time differences depending on the judgment of the physical therapist, and their effects are not discussed in this clinical study. Future clinical studies should include patients from multiple centers and more prehospital factors should be considered.
Assigning specialized physical therapist at the AECCC significantly shortened the number of days until rehabilitation was achieved and decreased the incidence of pulmonary complication in patients with sepsis. Reducing the number of days from hospitalization to the start of rehabilitation was also associated with the reduction of pulmonary complications in patients with sepsis. Reducing the number of days until rehabilitation is easy to adopt in many hospitals. We recommend assigning specialized physical therapists in the emergency unit and ICU to reduce pulmonary complications in patients with sepsis.
The authors are grateful to the paramedics, nurses, and staff of the Department of Rehabilitation at Shinshu University Hospital. The authors would like to thank Editage for the review.
Yasunari Sakai accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Mr. Yamamoto, Mr. Karasawa and Mr. Sato, Mr. Nitta, Mrs. Okada contributed to the data collection. Mr. Yamamoto contributed to the statistical analysis. Mr.Ikegami, Mr. Imamura, Mr. Horiuchi have contributed to data collection and interpretation and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This research did not received a specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors declare that they have no competing interests.
Not applicable.
Not commissioned.
Citation: Sakai Y, Yamamoto S, Karasawa T, Sato M, Nitta K, Okada M, et al. (2020) Early Rehabilitation Provided by Specialized Physical Therapist in an Emergency Center Reduces Pulmonary Complications in Patients with Sepsis: A Retrospective Cohort Study. Int J Phys Med Rehabil 8:550. DOI: 10.35248/2329-9096.20.08.550
Received: 11-May-2020 Accepted: 25-May-2020 Published: 01-Jun-2020 , DOI: 10.35248/2329-9096.20.08.550
Copyright: © 2020 Sakai Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.