Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Case Report - (2022)Volume 11, Issue 3
Ovarian cancer is the most lethal gynecological malignancy in the industrialized countries and is characterized by an intraperitoneal spread involving the wall of the large bowel from serosa. Rarely, both at the time of diagnosis and in recurrences, neoplastic metastasis to colon and rectum spread through vessels presenting as an intraluminal masses that involve mucosa and submucosa and mimic a primitive colonic cancer. In this case report, we present a case of a 49-year-old patient that showed irregular bowel motion alternating diarrhea and constipation, after ten months from the first surgery with complete cytoreduction for ovarian cancer. Primitive cancer was a mixed high-grade epithelial adenocarcinoma, clear cell and serous, FIGO staging IIB. Colonoscopy showed an intraluminal fungating mass of about 3 cm at 7 cm from the anal verge, with macroscopic aspect suggesting a primitive colonic cancer. A biopsy was performed, and the diagnosis was consistent with recurrence of ovarian adenocarcinoma. No serosal infiltration was present. The patient was treated with left hemicolectomy. Furthermore, we reviewed the literature about other cases of intraluminal colonic recurrence and articles about differential diagnosis between primitive cancer of colon and rectum and metastasis/recurrence from ovarian cancer.
Ovarian cancer, Ovarian cancer recurrence, Colonic metastasis, Colonic cancer, Combined targeted therapies
Ovarian cancer is the most lethal gynecological malignancy in the industrialized countries; in 2020, it is estimated that 21,750 new cases and 13,940 deaths will occur in the United States and 29,000 deaths will occur in Europe. [1,2]
Most of the cases are epithelial cancer (90%), the remaining arise from the substance of the ovary, called stromal tumors, or from embryological differentiation.
About 70% of the ovarian cancers are diagnosed at advanced stages, because of the endoperitoneal spread occurs early in the natural history of this cancer, and there are no specific symptoms. Other ways of diffusion are lymphatic and endovascular.
Colon and rectum are one of the most frequent involved sites at the time of diagnosis, because of the early intraperitoneal seeding of the Douglas pouch and the subsequent invasion to the inner layers of the intestinal wall. The pathway of dissemination of ovarian neoplasm to the colon and rectum may involve four different routes: by direct infiltration of the bowel wall, by spreading through the peritoneum, or rarely lymphogeneus, or hematogenous. [3,4]
Although there have been many significant advances in the treatment of ovarian cancer over the past decade, recurrent ovarian cancer remains an almost uniformly fatal disease [5]. This report presents the case of a patient with recurrent ovarian cancer which an isolated metastasis to the rectum limited to the mucosa and submucosa was present without any serosal involvement.
Case Presentation
A 49-year-old patient underwent a total laparoscopic hysterectomy, bilateral oophorectomy and peritoneal washing for a 10-cm left ovarian mass. The intraoperative pathologic evaluation was positive for borderline tumor, so partial omentectomy and a biopsy on a micropapillary area on the peritoneum next to the left ovary were performed. No other suspicious area was detected during the evaluation of the explorable celomatic serosa. The definitive pathologic diagnosis was mixed high-grade epithelial adenocarcinoma, clear cell and serous, of the left ovary; right ovary was negative for malignancy; malignant tissue was present on the peritoneal biopsy (diameter 3 mm). Preoperative serum cancer antigen 125 (CA-125) was negative (26.2 U/ml), as Carcinoembryonic antigen (CEA) and cancer antigen 19.9 (CA- 19.9).
After two weeks from the first surgery, a laparotomy for complete surgical staging was performed, with complete omentectomy, appendicectomy, pelvic and paraaortic lymph node dissection, with no macroscopic residual disease. The appendicectomy was performed because during the staging operation the surgeon had the suspect of involvement. At the pathologic evaluation, no evidence of malignancy was found. According to the International Federation of Gynecology and Obstetrics (FIGO) staging system, the tumor was stage IIB. The patient was treated with four cycles of carboplatin (AUC 6). It was decided to treat the patient with a lesser number of doses because of the young age and the little and unique extraovarian implant.
After ten months from the first surgery, the patient presented irregular bowel motion alternating diarrhea and constipation. Colonoscopy was performed and an intraluminal fungating mass of about 3 cm was described at 7 cm from the anal verge. A biopsy was performed, and the diagnosis was consistent with adenocarcinoma of possible ovarian origin. At the computed tomography (CT) scan no other site of tumor involvement was present. No information about serum CA-125, CA- 19.9 and CEA were available.
Therefore, the patient underwent a left laparoscopic hemicolectomy with primary end-to-end colorectal anastomosis. No other macroscopic disease sites were present. The pathologic evaluation confirmed the metastasis from ovarian adenocarcinoma, without serosal infiltration, and no malignancy was found in the 39 lymph nodes (Figure 1). The patient was treated for recurrent ovarian cancer with carboplatin, gemcitabine and bevacizumab.
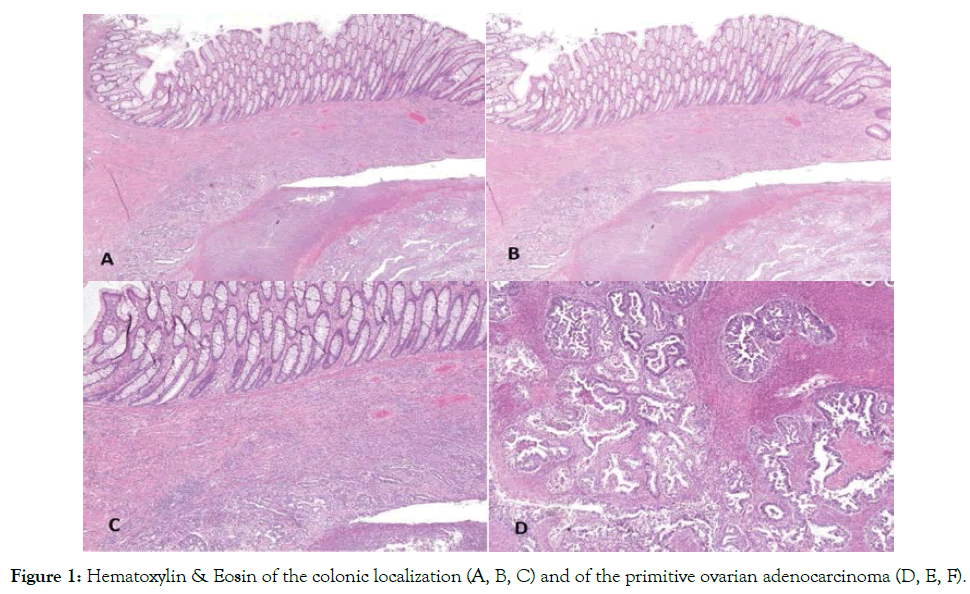
Figure 1. Hematoxylin & Eosin of the colonic localization (A, B, C) and of the primitive ovarian adenocarcinoma (D, E, F).
At the time of this report, there has been no evidence of recurrent or metastatic disease for 60 months (Figure 2).
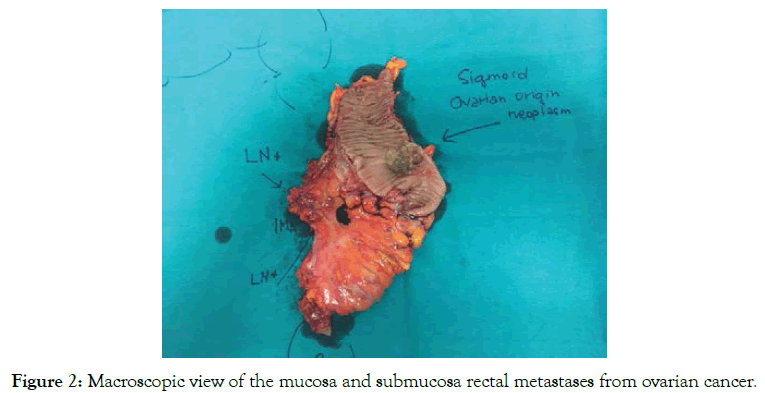
Figure 2. Macroscopic view of the mucosa and submucosa rectal metastases from ovarian cancer.
Colon and rectum are frequently involved by ovarian cancer, mostly at the time of diagnosis. The most frequent way of seeding is the invasion from the serosa by direct contact with the ovarian mass or from transcoelomic serous metastasis [3,4].
Rarely, colonic metastasis firstly affects mucosa and submucosa. Zighelboim et al reported a case of recurrence of an epithelial serous endometrioid ovarian carcinoma as an intraluminal bowel lesion with serosal sparing [6]. Kohyama et al reported another case of a patient that presented a protruding colon metastasis with intussusception six years after the first surgery for ovarian cancer [7]. Finally, Kim et al described a case of a 70-year-old woman who underwent surgery for a stage FIGO IIIB papillary serous cystoadenocarcinoma of the ovary and then presented with a large fungating mass at the coloscopy 8 years later [8].
The aforementioned cases, as in this case, showed rare cases of colonic intraluminal recurrence from ovarian, that presented difficulties in differential diagnosis of colonic metastasis and primary colon cancer. In fact, the macroscopic appearance and histologic architecture are very similar.
In these cases, serum CA125 and CEA can be helpful for the differential diagnosis [6,8]. However, about 15-20 percent of the ovarian cancers have negative CA-125 [6-9].
Immunohistochemical staining can be useful to differentiate the origin of the tumor. Loy et al found a CK7 negative/CK20 positive immunophenotype in 94% of the metastatic colonic tumors, 5% of the mucinous primary ovarian carcinomas, and none of the endometrioid or serous subtype in a series of 165 ovarian tumors [10]. However, no literature about immunohistochemical staining for differential diagnosis on series of colonic tumors is present.
For stage IIB ovarian cancer, the indication is for adjuvant chemotherapy with Carboplatin and Taxol for six cycles. At the time of diagnosis, this disease was considered at stage IC, because the 3-mm implant on the ovarian fossa was bethought as part of the primary disease and not seeding of the peritoneum. For this reason, the decision was to give only four cycles of Carboplatin.
The patient described in this article was treated with a left hemicolectomy, as she was affected by primitive colonic cancer. The study of O'Hanlan et al showed that 70% of the specimens where the dissection was performed had lymph node metastasis, in a series of bowel resection for ovarian carcinoma and hypothesized a longitudinal spread through lymph channels [3].
In this setting, the resection of bowel in a sleeve fashion could spare neoplastic tissue in the mesenteric lymph node and channels. This case shows the necessity of adequate adjuvant chemotherapy even in the case of a minimal implant on the pelvic peritoneum, which could cause a worsening of the prognosis.
Based on our experience, we suggest keeping in mind rare recurrence sites of disease during the follow up, as in this case, so it is important to evaluate properly symptoms referred by the patient and organize the proper diagnostic investigations.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Giuseppe C (2022) Early Rare Colonic Recurrence of Epithelial Ovarian Cancer: A Case Report. J Women's Health Care 11:570. doi: 10.35248/2167-0420.22.11.570.
Received: 30-Jan-2022, Manuscript No. JWH-22-15688; Editor assigned: 01-Feb-2022, Pre QC No. JWH-22-15688(PQ); Reviewed: 18-Feb-2022, QC No. JWH-22-15688; Revised: 28-Feb-2022, Manuscript No. JWH-22-15688(R); Published: 11-Mar-2022 , DOI: 10.35248/2167- 0420.22.11.570
Copyright: © 2022 Giuseppe C, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.