Internal Medicine
Open Access
ISSN: 2165-8048
ISSN: 2165-8048
Review Article - (2022)
Recently, Double Balloon Enteroscopy (DBE) has become a routine procedure in clinical practice for evaluation of small bowel diseases. Various population studies of DBE have reported the indications, diagnostic yields, therapeutic value and complication rates for small bowel diseases. Compare to other endoscopic technology that allows for the visualization of the small intestine, DBE has the advantage of having diagnostic biopsy and therapeutic procedures carried out at the same time for small intestinal lesions. Although the small bowel is a rare site for neoplasia, accounting for a little over 3% of the tumors that arise in the digestive tract. Benign lesions in small bowels are precursors to malignant lesions. We aimed to review the diagnostic yield and safety of DBE in small bowel tumors.
Small bowel tumors; Endoscopy; Double balloon enteroscopy; Diagnosis
SBTs: Small Bowel Tumors; DBE: Double Balloon Enteroscopy; VCE: Video-Capsule Endoscopy; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; GISTs: Gastrointestinal Stromal Tumors; OGIB: Obscure Gastrointestinal Bleeding; NETs: Neuroendocrine Tumors; SBFT: Small Bowel Follow-Through
The small intestine in humans is a long and tortuous organ, 5 to 7 meters in length and freely mobile in the abdominal cavity. Because of these anatomical features, endoscopic examination using conventional endoscopes has been challenging. Due to the difficulty associated with endoscopic examination, the small intestine was previously examined mainly by radiological methods such as contrast radiography, Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and angiography. Recent developments of Double Balloon Endoscopy (DBE) [1], have made endoscopic examination of the entire small bowel practical. This method has now changed the diagnostic algorithms for small bowel disease. DBE has an accessory channel and good maneuverability in the distal small intestine; this has enhanced endoscopic treatment of various small bowel diseases.
DBE is an advanced type of endoscopic procedure which brings the advantage of reaching the whole small bowel using anterograde or the retrograde route. This procedure is both diagnostic and interventional for a variety of small intestinal diseases, such as vascular lesions, tumors, polyps and inflammatory bowel diseases. DBE might be a bit laborintensive, but it enables tissue sampling and interventional therapies including hemostasis, balloon dilation against benign stricture, and polypectomy [2]. Since the invention of DBE, deep enteroscopy such as single-balloon enteroscopy and spiral enteroscopy [3,4], has been introduced.
Small bowel tumors
Small Bowel Tumors (SBTs) include a heterogeneous group of benign and malignant lesions. The most common primary morphological subtypes are adenocarcinomas (31%-45%), neuroendocrine tumours (NETs) (14%-52%) and sarcomas (8%-13%) [5-11]. Adenocarcinomas occur most frequently in the duodenum (46%-63%) [5,8,9,12].whereas NETs are most frequently seen in the ileum [5,7,9,13]. It mostly originates from the duodenum followed by jejunum then ileum with about 10% with unknown origin [14]. Incidence of all malignant tumors of the small intestine ranges from 0.5 to 1.5 out of 100,000 in males and 0.2 to 1.0 out of 100,000 in females [15]. The small intestine is about 70%-80% of the total length of the gastrointestinal tract, about 5-7 meters in length, however, neoplasms of this region are rare [16,17]. Only 3%-6% of gastrointestinal neoplasms and just about 1%-3% of malignant tumors of the gastrointestinal tract develop into the small intestine [16,17]. Pre-malignant lesions and polyposis syndromes are associated with the increased risk of developing small bowel carcinoma warranting screening, surveillance and appropriate treatment [18]. Epidemiological knowledge of SBTs helps to increase the awareness of this disease [19,20]. SBTs can be classified as malignant (including; adenocarcinoma, neuroendocrine tumor, lymphoma, sarcoma, etc. or benign (including; adenoma, leiomyoma, Lipoma, fibroma, Hemangioma, etc. [21]. Malignant SBTs are categorized into primary and secondary tumors. Benign SBTs are more common than malignant SBTs, accounting for up to 75% of all SBTs in an autopsy series [22]. Making a diagnosis of SBTs is difficult and the optimum technique varies depending on the site and size of the tumor. Upper gastrointestinal radiographic methods including Small Bowel Follow-Through (SBFT), CT, enteroclysis and enterography may reveal intestinal or lymph node masses, mucosal defects and sometimes intussusception [23]. Therefore, as part of the diagnostic workup in patients suspicious of SBTs, endoscopic examinations should be performed.
Benign tumors
Leiomyoma: Leiomyomas of the small intestine are the most common symptomatic benign SBTs, frequently occurring in the jejunum, followed by the ileum and lastly the duodenum [24,25]. Leiomyoma, after adenoma, is the most common tumor of the small bowel in human [4,26]. They are usually diagnosed incidentally either during small bowel evaluation for alternative reasons, necropsy evaluation or non-related surgical procedures [27]. Although described in human, other non-human primates such as dwarf galagos (Galagoides demidovii) and cotton-tap tamarins (Saguinus oedipus) are also suspected of the occurrence of this tumor [27,28]. They are typically vascular lesions and have a propensity to ulcerate and bleed, accounting for up to 65% of symptomatic patients developing gastrointestinal bleeding or iron deficiency anemia [24]. When evaluated endoscopically, they are usually single, gray-white, and firm and may display central umbilication [24].
Adenoma: Adenomas of the small intestine are the most common benign SBTs [24]. They are benign dysplastic lesions commonly seen in the duodenum, particularly in the ampullary region and may be categorized as tubulovillous, villous or Brunner's gland adenomas [29]. Like the colon, adenomas in the small intestine (particularly villous adenomas) are precursors to small bowel adenocarcinoma [30-32]. Non-ampullary small bowel adenomas greater than 1 cm in size have an increased risk of malignant transformation [33]. Most adenomas are single, although they can be multiple, especially when associated with an inherited syndrome such as hereditary familial polyposis. All patients undergoing local resection must undergo endoscopic surveillance [34].
Lipoma: Lipomas of the small intestine are benign, nonepithelial cell tumors of mesenchymal origin, that do not typically cause symptoms unless larger than 2 cm in size [34]. They are typically found in the colon, but may also be found in the small intestine, particularly the ileum (about 50%), less so in the duodenum (about 25%) and jejunum (about 25%) [35]. Small bowel lipoma is the third most common benign SBTs [24]. They are mostly found incidentally during surgeries and autopsies [24]. Small bowel lipomas are typically harmless collections of fat on the wall of the intestine. As such, treatment and surveillance are not indicated. Treatment is warranted, in the event of symptoms or complications, seen mostly in lipomas larger than 2 cm in size, such as bleeding, anemia, obstruction, volvulus or intussusception [36].
Hemangioma: Hemangiomas of the small intestine are most often seen in the mid-jejunum or ileum, accounting for up to 0.05% of all benign intestinal neoplasms [24,37,38]. Hemangiomas originate from the submucosal vascular plexus and are classified into capillaries, cavernous or mixed lesions. Gas coyen in the mid-19th century were the first to discover and describe it as a blue rubber nevus syndrome, “Naevi of the viscera” [39]. Recently, these lesions are increasingly diagnosed owing to the advent of small bowel endoscopy with video capsule endoscopy and enteroscopy [39,40]. They vary in size from tiny to large lesions, and may be multiple, with the jejunum being the common site of involvement. They may cause abdominal pain, bleeding and/or obstruction. Advances in endoscopic techniques with argon plasma coagulation, and sclerotherapy, have led to successful endoscopic interventions, however large lesions need surgical resection [41-43].
Familial adenomatous polyposis
This is an autosomal dominant condition associated with an increased risk of SBTs, caused by mutations of the Adenomatous Polyposis Coli (APC) gene on chromosome 5 [44]. Familial adenomatous polyposis is characterized by the development of hundreds to thousands of adenomatous polyps in the colorectum during childhood and adolescence. Without surgical intervention, patients will almost inevitably develop colorectal cancer by the age of 40 years. Therefore, prophylactic colectomy is usually performed before age 25 [45].
Lymphangioma
Lymphangiomas are benign vascular tumors and are extremely rare in adults and in the gastrointestinal tract. Although the etiology remains unclear, they may be associated with anomalous development of the lymphatics or inflammation and obstruction of developed lymphatic vessels [46]. The majority of cases are asymptomatic and thus detected incidentally. Nevertheless nonspecific symptoms, including abdominal pain, nausea, vomiting and weight loss may be present [47]. Lymphangiomas rarely require specific treatment, unless complications, such as bleeding, intussusception and protein-losing gastroenteropathy are present [48]. Lymphangiomas are uncommon benign tumors, accounting for only 3% of the SBTs. They can be cavernous or cystic.
Malignant tumors
Malignant tumors arising from the small bowel have a poorer prognosis compared to tumors from other parts of the gastrointestinal tract [49].
Neuroendocrine Tumor (NET): Neuro Endocrine Tumors (NETs) of the Gastrointestinal (GI) tract are rare, but the incidence and prevalence of NETs are steadily rising, possibly owing to the detection of early-stage disease and stage migration [50]. Survival for all NETs improved over time, especially for advanced-stage GI-NETs, and particular for pancreatic NETs in particular, reflecting major therapeutic improvements [51]. However, molecular data which may explain the clinical heterogeneity of this class of tumors, from indolent to highly aggressive and divergent treatment responses, are lacking [52]. NETs comprise a genetically diverse spectrum of malignant solid tumors arising from the secretory cells of the neuroendocrine cell system that may produce peptides causing characteristic hormonal syndromes [53]. Therefore, GI-NETs are categorized as “functioning” when patients are clinically symptomatic (carcinoid syndrome) or “non-functioning.” The majority of NETs occur sporadically. However, they may occur as part of complex familial endocrine cancer syndromes such as type 1 Multiple Endocrine Neoplasia (MEN 1), von Hippel-Lindau Disease, and Neurofibromatosis type 1 (NF1) [54-56].
Adenocarcinoma: Small bowel adenocarcinomas are rare and unique tumors, which are often diagnosed at an advanced stage due delayed clinical presentation and non-specific symptoms (i.e., abdominal pain, weight loss, nausea and vomiting, occult GI tract bleeding), coupled with a limited sensitivity of conventional radiological imaging for the detection of this type of cancer [57,58]. Adenocarcinoma begins in the lining of the small intestine in glandular cells. These tumors develop and occur in the upper part of the small intestine and may grow to block the intestine [24].
Lymphoma: Lymphoma is generally diagnosed on the basis of characteristic imaging and confirmed with core biopsy. Unlike most other small bowel tumors, the mainstay of treatment is chemotherapy and resection can generally be avoided. Resection may be appropriate for those who present with perforation, bleeding or obstruction but these patients should still receive systemic chemotherapy [59]. Immunohistochemistry and cytometric studies have distinguish whether lymphomas are of Bcell or T-Cell origin, with the former expressing CD19 and CD20. The most common types of gastrointestinal lymphomas encountered in small bowel are diffuse large-B-cell lymphoma, enteropathy associated T-cell lymphoma, extranodal marginal zone B-cell lymphoma (also known as lymphoma of mucosa associated lymphoid tissue, MALT), mantle cell lymphoma and Burkitts lymphoma [60].
Sarcomas and Gastrointestinal Stromal Tumors (GISTs): Sarcoma is a heterogeneous group of malignancies historically treated with classic cytotoxic chemotherapy, Soft tissue sarcomas are rare tumors that represent a major challenge due to varying clinical presentations and often interdisciplinary treatment concepts. GISTs are tumors that originate from mesenchymal cells of the gastrointestinal tract that mostly express the c-kit proto-oncogene protein [61]. The protein, also known as CD117, is located on the cell membrane and has tyrosine kinase activity, acting as a growth factor receptor. Mutation in the c-kit oncogene occurs in about 80% of the cases, resulting in an activation of cell proliferation, inhibition of apoptosis and angiogenesis [61].
GISTs are more frequently located in the stomach (50%-60%), small intestine (20%-30%), colon and rectum, peritoneum, esophagus and mesentery (10%) [62]. Endoscopically, they are presented as a protruded sub epithelial lesion, sometimes ulcerated, and with dilated vessels [63]. The majority is diagnosed in an advanced stage after causing severe bleeding. Capsule Endoscopy (CE) represents the first endoscopic approach for Obscure Gastrointestinal Bleeding (OGIB), and might diagnose a suspected GIST. Device-Assisted Enteroscopy should be the next tool for diagnostic confirmation and possible biopsies [64].
Diagnosis of SBTs is often done at an advanced stage due to the non-specificity of the symptoms, the low degree of suspicion and the difficulty in assessing the organ. Cross-sectional imaging techniques including CT or MRI can be used for the diagnosis, and SBTs staging [65].
Until recently, the small bowel was the only part of the alimentary tract that was not completely accessible by endoscopy [66]. Only indirect evaluation was possible using small-bowel follow-through barium examination or enteroclysis, but patient discomfort, the high radiation dose, and labor intensiveness limit these barium studies [66]. CT is often used as a frontline tool in the evaluation of abdominal symptoms. CT, CT enterography, and CT enteroclysis can identify masses, but these methods occasionally lack the sensitivity to diagnose small tumors and have a limited capacity to differentiate between tumor types [67]. The advent of Video Capsule Endoscopy (VCE) and DBE is a significant breakthrough for the visual diagnosis of SBTs located deep in the small bowel.
In a Japanese multicenter study, DBE identified 144 SBTs (13.9%) in 1,035 patients undergoing DBE [68]. In the same study, the most common indication for DBE was the suspected presence of a SBT (42.4%) [68]. For subjects without SBT, the most common indication was obscure GI bleeding. Malignant lymphoma and GIST were the most frequent (21.5%) and the second-most frequent SBTs (18.8%), respectively [68].
Double balloon enteroscopy procedure in small bowel tumors
DBE is a procedure developed by Yamamoto and colleagues in 2001 [69], an exciting new endoscopic technique that allows for a complete visualization and therapeutic interventions in the entire small intestine. Preliminary experiences with DBE have illustrated the capability to perform total small-bowel enteroscopy with a good safety profile and patient tolerance for this procedure [69-76]. DBE is a novel technique of great interest to clinician, as it offers the opportunity to examine the whole small bowel without any carrying out invasive operation. Diagnostic and therapeutic ability of the procedure influences the importance and common use of DBE for patients with documented or suspected small bowel disease.
DBE is a procedure used to view the inner portion of the small intestine, a special instrument made up of two tubes (one inside the other) is inserted via oral or anal route into the small intestine [77]. The DBE system consists of a mainframe, a 200 cm-long enteroscope, a 150 cm-long overtube and an air pump. Two latex balloons are attached to the tip of the endoscope and the overtube (Figure 1), which can be infated and defated with air by a pressure-controlled pump system. The inner tube, which is an endoscope with a light and lens for viewing, is moved through part of the small intestine, and a balloon at the end of it is inflated to keep the enteroscope in place. The outer tube is moved through the small intestine to reach the end of the enteroscope. To reduce the friction when performing a procedure, water can be injected into the space between the enteroscope and the overtube. As described by Yamamoto, et al. [77], the standard technique is to guide the scope in the small bowel with sequential infation and defation of the two balloons for the “push and pull back” maneuveras. These steps are repeated many times as the tubes move through the whole small intestine [77].
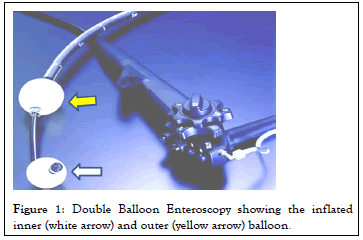
Figure 1: Double Balloon Enteroscopy showing the inflated inner (white arrow) and outer (yellow arrow) balloon.
Patient preparation for DBE procedure
Twelve hours of solid food and approximately 4 hours of clear liquid fasting will be enough for a patient to be prepared for oral DBE. However, standard colonoscopy preparation with restricted diet and laxatives will be needed for anal route examination [78]. Peroperative sedation is necessary as the procedure duration is long and low patient tolerance is expected to disturb the success of the procedure. Many options can be used for sedation but conventional conscious sedation with propofol is mainly used. Deep monitored sedation (with propofol, midazolam and/or fentanyl) can be preferred for oral examination with prolonged duration of the procedure [79]. The double balloon system allows the endoscope to advance very deep into the small intestine: An organ that is approximately 20 feet in length! This procedure allows for diagnosing and treatment of various small bowel diseases [80-87].
Roles of double balloon endoscopy in diagnosing and treatment of small bowel tumors
The most frequent clinical presentations of SBTs are Obscure Gastrointestinal Bleeding (OGIB), weight loss, diarrhea and abdominal pain [80]. Conversely, the diagnosis of SBTs is often done at an advanced stage due to the non-specificity of the symptoms, the low degree of suspicion and the difficulty in assessing the organ. It has been demonstrated that SBTs represent the second most common cause of OGIB, representing around 18.5% of these patients [81]. The combination of antegrade (orally) and retrograde (anal) routes allows the examination of the entire small bowel in about 70% of the cases using DBE [82]. It has been demonstrated that DBE has higher positive rate of diagnosis (85.9%) when compared to compute tomography scan (72.9%), when an SBT is suspected [83]. Although CT, VCE, fluoroscopic enteroclysis, and PET are useful for making a diagnosis of SBTs, only DBE enables a biopsy of lesions and thus a definitive diagnosis. DBE can identify SBTs undetected by other examinations and precisely localize tumors by tattooing so they can be readily identified during surgery. In the evaluation of SBTs, CT is often the initial examination, but its reported detection rate for SBTs smaller than 10 mm in size is low and also lower than that for VCE or DBE [65]. The double-balloon endoscope when inserted can easily achieve a high percentage of endoscopic observation for the entire small intestine. The double-balloon endoscopy features are not only good for insert ability, but also good maneuverability even after it is inserted distally. It is a useful method and because of its good maneuverability, it enables endoscopic observation and treatment even in the distal small intestine. DBE also allows endoscopic intervention, including argon plasma coagulation, polypectomy, and balloon dilation.
Diagnostic yield of double balloon enteroscopy
The reported diagnostic yields of DBE, ranges from 12.1 to 80% [84-90]. In an American study by Cangemi, et al. SBTs detection rate of 12.1% was reported [91,92]. Similarly, in an Asiatic retrospective study, Chen, et al. [83,84] reported 16.8% overall diagnostic yield. In another retrospective analysis of crosssectional case series, the authors concluded that DBE is a valuable tool for the detection and diagnosis of SBTs, especially when tumors were suspected [68]. Robles, et al. reported that DBE had modified the outcome of 25% patients. The authors underscored that DBE does not only have diagnosis capabilities but also therapeutics interventions [92]. The diagnostic yield variability of DBE among these studies can be attributed to diferences in the indications, inclusion criteria and other biases. DBE has a great impact on SBTs management, and some authors report changing therapeutic plans in almost two thirds of patients, including suspension of an emergency surgery, modification on the surgical approach, and the type of resection [84]. DBE is a useful and safe procedure for making a definitive diagnosis of metastatic SBTs and can also aid in the selection of the appropriate surgical procedure, and save time by assisting surgeons to locate tumors for resection.
Double balloon enteroscopy is a feasible technique that allows adequate examination of both the small and large bowel, specifically for various endoscopic procedures of small intestinal lesions. It is also a safe procedure, useful, and provides high clinical yield. Given its safety profile with low incidence of complications, DBE is regarded as safe and one of the most accurate diagnostic modality, allowing for endoscopic biopsy and therapeutics in addition. BDE has also proven to be a valuable tool for the detection and diagnosis of SBTs, especially when metastases are suspected. It is as well safe and effective in the resection of SBTs deep within the small bowel without laparotomy. It is therefore recommended that DBE should be performed as soon as possible if small bowel disease is suspected after negative upper and lower endoscopy. Notwithstanding, future prospective studies comparing DBE with other available imaging modalities is needed to assess the significance of DBE in small-bowel diseases.
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[PubMed]
[Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
[Cross Ref] [Google Scholar] [PubMed]
Citation: Adu IK, Zhang H (2022) Double Balloon Enteroscopy in Small Bowel Submucosal Tumor Diagnosis: A Short Narrative Review. Intern Med. S10:001.
Received: 25-Jan-2022, Manuscript No. IME-22-15711; Editor assigned: 27-Jan-2022, Pre QC No. IME-22-15711(PQ); Reviewed: 10-Feb-2022, QC No. IME-22-15711; Revised: 15-Feb-2022, Manuscript No. IME-22-15711(R); Published: 22-Feb-2022 , DOI: 10.35248/2165-8048.22.12.001
Copyright: © 2022 Adu IK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO