
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2023)Volume 14, Issue 3
Purpose: This double-blind, split-mouth randomized clinical trial investigated whether etoricoxib or dexamethasone is effective to control postoperative pain, edema, and trismus after extraction of impacted mandibular third molars.
Methods: Twenty-eight patients received a single dose of dexamethasone (4 mg) (G1) or etoricoxib (120 mg) (G2) before surgery and were examined for the presence of pain, edema, and trismus for 72 hours. Pain was evaluated by the Visual Analogue Scale (VAS) and total administration of rescue analgesic medication (paracetamol, 500 mg tablets). Edema was quantified by the VAS and five facial measures, whereas trismus was assessed by measuring the maximum opening of the mouth. Twenty-eight patients in need of impacted third molar surgery met the eligibility criteria.
Results: Patients in G2 used rescue analgesic medication 12 hours after surgery and reported minimal pain experience in the VAS (0.335 cm), suggesting that postoperative pain was significantly controlled with the administration of etoricoxib (P<0.0001). Patients who received dexamethasone experienced pain levels 3.6-fold greater in the VAS (1.21 cm) and used the rescue analgesic medication more frequently, with a mean of 3.4 tablets. While the facial measures showed no significant differences between the groups concerning edema, self-assessed VAS data indicated that G1 patients experienced edema more frequently. There were significant differences regarding the control of trismus between the groups (P>0.05).
Conclusion: Our findings indicated that etoricoxib (120 mg) was significantly more effective in controlling postoperative pain than dexamethasone (4 mg) and that both drugs were comparable for the control of edema and trismus.
Analgesic; Anti-inflammatory drug; Third molar; Tooth extraction; Pain
Mandibular third molar extraction has been considered a suitable pharmacological model to test the efficacy of analgesic and anti-inflammatory drugs for acute pain, edema, and trismus [1,2]. The extraction of impacted third molars is one of the most common surgical procedures not only in dental care but also in general medicine [3,4]. Nevertheless, inflammatory events such as pain, edema, and trismus may occur and dramatically affect the patient's quality of life, especially in the first three postoperative days [5-7]. Hence, some pharmacological strategies have been extensively used to prevent postoperative pain and discomfort, which include a preoperative administration of corticosteroids and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) [8,9].
Corticosteroids have been prescribed since the 1960 for their potent anti-inflammatory and immunosuppressant effects. Dexamethasone is a corticosteroid that has been routinely used to reduce pain and discomfort after third molar extractions [10]. The mechanism of action of corticosteroids relates to the inhibition of the enzyme Phospholipase A2 (PLA2), which reduces the release of arachidonic acid in the cells around the inflamed focus. This process downregulates the synthesis of prostaglandins and leukotrienes and diminishes neutrophil accumulation, which explains, at least partly, the greater potency of corticosteroids as compared to NSAIDs [11,12].
NSAIDs are commonly prescribed for their analgesic, antipyretic and anti-inflammatory properties [13,14]. However, the long- term administration of NSAIDs is associated with serious side effects, such as gastrointestinal and cardiovascular disorders which can be minimized with the administration of low doses [15-17]. Etoricoxib is a selective cyclooxygenase-2 inhibitor that promotes minimal gastrointestinal disorders and minimal risk of fluctuating blood pressure [18,19]. Scientific evidence suggests that preoperative administration of etoricoxib is safe. Yet, while the pharmacokinetics and pharmacodynamic properties of etoricoxib are well documented, little is known about its analgesic and anti-inflammatory efficacy in impacted third molar surgery [20].
The efficacy of preemptive analgesia with corticosteroids and NSAIDs was demonstrated in previous studies there is no consensus in the literature on the most effective drug protocol to prevent postoperative pain after mandibular third molar surgery [21,22]. In a meta-analysis, showed that there is insufficient evidence to conclude that dexamethasone is better than NSAIDs or methylprednisolone as a preemptive analgesic. To elucidate this issue, we carried out a double-blind, split-mouth randomized clinical trial comparing the efficacy of preoperative dexamethasone and etoricoxib in a single dose to control pain, edema, and trismus after extraction of bilateral impacted mandibular third molars [23].
This study was previously approved by the Research Ethics Committee of the School of Dentistry at the Federal University of Alfenas (UNIFAL-MG), under protocol no. 2.543.762, and complies with the recommendations of the Declaration of Helsinki. Eligible participants were instructed on the risks and benefits of third molar surgery and the use of analgesic drugs. Those who agreed to participate signed an informed consent form.
This study had a double-blind, split-mouth randomized design. Patients were recruited from August to December 2017 at the Surgery Clinic of the School of Dentistry, Unifal-MG. A total of 474 patients with bilateral impacted mandibular third molars were screened. The eligibility criteria consisted of age range from 18 to 30 years; presence of mandibular third molars with similar mesioangular and vertical positions (winter’s classification) and with similar angles and degrees of impaction. Further information on patient recruitment and the reasons for exclusion are described in Figure 1. A total of 436 patients were excluded from the study for several reasons, including diabetes (n=6), ineligible age (n=82), use of systemic medications and medical history of systemic conditions, hypersensitivity to the tested drugs, or periodontal disease (n=138) and smoking habits (n=35). The final sample size was composed of 38 participants of both sexes, aged 18 years to 30 years, who were randomly allocated into the study drugs, as further described.
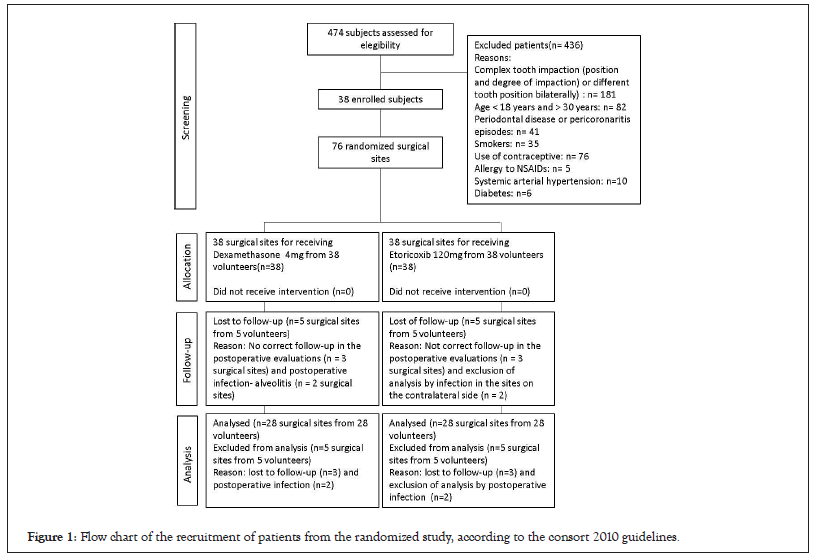
Figure 1: Flow chart of the recruitment of patients from the randomized study, according to the consort 2010 guidelines.
Study design
Participants were submitted to extraction of the left and right mandibular third molar separately and were blinded to the drug administered preoperatively. The sequence of extractions (first and second) of the right and left mandibular molars was randomly assigned for each participant, followed by a computer- generated allocation of the two preemptive treatments, namely: G1, 4 mg of dexamethasone (Decadron® 4 mg, Merck Sharp and Dohme Farm. Ltda, Campinas, Sao Paulo, Brazil); and G2, 120 mg of etoricoxib (Arcoxia® 120 mg, Merck Sharp and Dohme Farm. Ltda, Campinas, Sao Paulo, Brazil). Both drugs were administered 1 hour before the surgery, and an interval of 21 days was considered between the surgical procedures, which were shown to be sufficient for mouth opening to return to normality [24].
Surgical procedure
All surgical procedures were performed by the same operator, who was blinded to the study groups. Intraoral and extraoral antisepsis was performed with 0.12% and 2% chlorhexidine digluconate, respectively. The inferior alveolar, buccal and lingual nerves were anesthetized with 2% lidocaine hydrochloride with 1:100,000 epinephrine (DFL Ind. Com. S.A., Rio de Janeiro, RJ, Brazil) up to 2 anesthetic tubes. Latency time, duration of the anesthesia, and surgical time were recorded.
An incision was made, the surgical flap was detached, and ostectomy and odontosection procedures were performed using a high rotation carbide drill (KG Sorensen, Cotia, SP, Brazil) under heavy irrigation with saline solution (0.9% sodium chloride, Glicolabor Ind. Farm. Ltda, Ribeirão Preto, SP, Brazil). The tooth was extracted and the alveolar bone was cleaned, irrigated with saline solution, and sutured with 4-0 silk thread (Ethicon, Johnson and Johnson, New Jersey, USA). Patients were given rescue analgesic tablets after surgery (Tylenol®, 500 mg paracetamol, orally, Janssen-CILAG Pharmaceuticals Ltda., Sao Jose dos Campos, SP, Brazil), to treat potential episodes of uncontrolled pain. Patients were verbally oriented and received booklets that contained written guidelines for postoperative care.
Assessment of pain, edema and trismus
Postoperative pain was assessed by the Visual Analogue Scale (VAS) and the number of rescue analgesic tablets administered. Participants were asked to fill out the VAS before and after surgery (1, 2, 3, 6, 12, 24, 48, and 72 hours). They were also instructed to count the number of rescue analgesic tablet that were used at 6, 12, 24, 48, and 72 hours following the procedure [25].
Facial edema was quantified through five linear facial measures and by the VAS before and after surgery (24, 48, and 72 hours). The facial points were marked with a dermographic pen in the following regions of the face: mandibular angle (gonion point- Go-most lateral point of the mandible angle); tragus (T); labial commissure (cheilion point-Ch-labial commissure); nose wing (Alare-Al-most lateral point of the nasal alar contour), lateral corner of the eye (exocanthion-Ex-external commissure of the ocular fissure) and mentum (pogonion-Pg-most anterior point of the chin). The reference points proposed by Neupert, et al. [10] were used in the present study with the abbreviations and definitions established by Farkas [26]. The mandibular angle (Go) was used as a reference point from which the linear distance to the other points was measured in mm using dental floss. The difference observed in each measurement between pre and postoperative records determined the facial volume variability in the postoperative period.
The self-assessment of edema by the VAS consisted of a 10 cm line whose one end corresponded to no edema whilst the other end indicated the greatest possible edema. The assessment of mouth opening was performed by measuring the upper-lower interincisal distance from the maxillary left central incisors with the aid of a caliper. Measurements were performed before and after surgery (24 hours, 48 hours, and 72 hours).
Statistical analysis
The data were analyzed by two-tailed tests, considering an alpha error of 0.05. When interactions were tested, an alpha error of 0.15 was applied. Statistical tests were performed in the SAS 9.3 and Sudaan Callable 11.0. The data were checked for normality and expressed descriptively by mean, standard deviation, median, and interquartile range, as appropriate. Pairwise comparisons between the experimental groups considered the cluster of events within individuals. Accordingly, bivariate analyses were performed using Wald-chi-square controlling for cluster or Friedman tests for categorical and continuous variables with non- normal distribution, respectively. As for normally distributed outcomes, a mixed-model analysis of variance was carried out (considering the individual as a random factor), followed by residual analysis for assumption tests.
Multivariate analyses for non-normally distributed continuous outcomes were performed using non-parametric statistics. A mixed-model was used (Proc Mixed Routine and the command AnovaF), with the MIVQUE0 estimation method and an unstructured covariance matrix per group. Whenever appropriate, confounders were included in the analysis (teeth, sequence of treatment, sex, and age). The risk of taking rescue analgesic was estimated by Poisson regression with robust error estimators, considering the cluster of events within individuals. Given some known possible differences in pain between the sexes and the possibility of a painful event to influence another, the model was adjusted and two-level interactions were tested between the treatment and order of treatment and the surgical side (left or right).
The study flowchart, patient recruitment, and the reasons for exclusion are shown in Figure 1. A total of 38 individuals met the eligibility criteria and were included in the study. These participants experienced no complications during the surgical procedure such as nausea, vomiting, or low blood pressure. However, two female patients developed an infection on one side of the surgical wound and eight patients (4 females) dropped out on the first three postoperative days claiming that they had other commitments. Hence, 28 individuals completed the trial protocol, of which 10 were males (35.7%) and 18 were females (64.4%) with an average mean of 21 years (SD=2.9; min=18, max=30). Although females were slightly younger (mean of 20.9 years, SD=2.7) than males (mean of 21.2 years, SD=3.4), there was no statistical difference in the participants age (P=0.7953). Despite the facts that groups were randomized before the study and mostly because of sample loss, G1 was more frequently assigned to the right molar (57.1%, n=16) than to the left molar (43.1%, n=12) and vice versa, although such a difference was not significant (P=0.2850). No patient was excluded due to a surgical time longer than 30 minutes, which corresponds to the latency period of the anesthetic drug (Figure 1) [27].
Table 1 shows the descriptive statistics of all outcomes during the 72 hours study follow-up. Some variables are expressed in medians and quartiles due to non-normal data distribution. On average, the time spent on each surgical section (latency, surgical time, and suture) did not differ between the treatment groups (P>0.05). The VAS data indicated that patients in G1 experienced higher pain intensity than those in G2 in all postoperative periods (P<0.001). The maximum average pain occurred at 6 hours for G1 while it continued to increase up to 12 hours in G1. Moreover, patients in G1 took more rescue analgesic tablets throughout the study than those in G2 (P<0.0001). G1 also was associated with higher levels of edema (VAS data) in all postoperative periods and the entire study period as compared to G2, but no statistical differences in edema were observed through facial measures. Even though study participants experienced trismus over time, that is, a decline in mouth opening measurements, there was no statistical difference between G1 and G2 (P>0.0001) (Table 1).
| DEXA (G1) | ETORI (G2) | ||||
|---|---|---|---|---|---|
| Mean(SD) | MD(Q1-Q2) | Mean(SD) | MD(Q1-Q2) | p* | |
| Surgical time(min) | |||||
| Latency | 6.2(2.5) | 5.7(4.2-8.0) | 5.9(2.5) | 5.0(4.5-8 .0) | 0.4255* |
| Time 1 | 18.1(5.6) | 17.5(14.5-21.0) | 17.7(5.1) | 18.5(13.5-22.0) | 0.9754 |
| Time 2 | 25.5(7.0) | 24.5(20.0-31.0) | 24.6(5.7) | 24.5(20.5-27.5) | 0.9642 |
| Surgical time (total) | 31.7(5.6) | 30.5(25.7-33.5) | 30.5(6.9) | 30.5(25.7-33.5) | 0.6153 |
| Pain VAS | |||||
| Baseline | 0 | 0 | 0 | 0 | |
| 1 hrs | 0.58(0.4) | 0.53(0.15-0.95) | 0.13(0.2) | 0.02(0.00-0.25) | 0.0011 |
| 2 hrs | 1.13(0.7) | 0.93(0.76-1.34) | 0.28(0.3) | 0.15(0.03-0.45) | 0.0002 |
| 3 hrs | 1.54(1.0) | 1.16(0.80-2.46) | 0.48(0.4) | 0.44(0.10-0.80) | 0.0025 |
| 6 hrs | 1.70(1.0) | 1.15(1.00-2.45) | 0.49(0.4) | 0.45(0.10-0.97) | <0.0001 |
| 12 hrs | 1.96(1.3) | 1.75(1.10-2.57) | 0.45(0.4) | 0.35(0.07-0.87) | <0.0001 |
| 24 hrs | 1.86(1.2) | 1.96(1.05-2.55) | 0.49(0.4) | 0.37(0.08-0.91) | <0.0001 |
| 48 hrs | 1.24(0.8) | 1.08 (0.70-1.94) | 0.44 (0.4) | 0.26 (0.04-0.73) | 0.0007 |
| 72 hrs | 0.91(0.8) | 0.69 (0.20-1.07) | 0.26 (0.3) | 0.05 (0.00-0.55) | 0.0003 |
| Analgesic rescue (n) | 3.4(2.4) | 3(2-5) | 0.4(0.8) | 0(0-1) | <0.0001 |
| Edema (VAS) | |||||
| 12 hrs | 0.01(0.1) | 0 | 0.01(0.1) | 0 | 0.763 |
| 24 hrs | 2.06(0.8) | 2.02(1.33-2.51) | 1.13(0.4) | 1.03(0.93-1.18) | 0.0025 |
| 48 hrs | 2.34(0.8) | 2.37(1.91-2.84) | 1.34(0.4) | 1.21(1.05-1.60) | 0.0011 |
| 72 hrs | 2.11(0.6) | 2.02(1.76-2.57) | 1.15(0.3) | 1.05(1.00-1.29) | 0.0007 |
| Edema GoT | |||||
| 12 hrs | 5.85(0.17) | 5.90(5.77-5.98) | 5.89(0.26) | 5.90(5.80-6.06) | 0.4896 |
| 24 hrs | 5.89(0.17) | 5.93(5.81-6.01) | 5.92(0.26) | 5.93(5.84-6.11) | 0.5328 |
| 48 hrs | 5.92(0.17) | 5.96(5.84-6.04) | 5.95(0.25) | 5.97(5.86-6.12) | 0.5132 |
| 72 hrs | 5.90(0.16) | 5.95(5.83-6.03) | 5.95(0.26) | 5.96(5.86-6.12) | 0.4789 |
| Edema GoEx | |||||
| 12 hrs | 9.87(0.30) | 9.91(9.65-10.15) | 9.88(0.30) | 9.92(9.64-10.10) | 0.8909 |
| 24 hrs | 10.10(0.51) | 10.01(9.77-10.36) | 10.12(0.47) | 10.16(9.80-10.42) | 0.7567 |
| 48 hrs | 10.17(0.31) | 10.18(9.95-10.43) | 10.19(0.30) | 10.25(9.94-10.37) | 0.8242 |
| 72 hrs | 10.14(0.36) | 10.11(9.88-10.41) | 10.18(0.31) | 10.18(9.91-10.33) | 0.6522 |
| Edema GoCh | |||||
| 12 hrs | 8.38(0.29) | 9.13(8.84-9.26) | 8.38(0.31) | 9.11(8.86-9.25) | 0.9692 |
| 24 hrs | 9.06(0.29) | 9.14(8.88-9.31) | 9.07(0.31) | 8.40(8.17-8.60) | 0.9147 |
| 48 hrs | 9.07(0.28) | 8.42(8.13-8.55) | 9.09(0.32) | 9.10(8.85-9.27) | 0.807 |
| 72 hrs | 8.86(0.29) | 8.88(8.66-9.04) | 8.91(0.36) | 8.95(8.75-9.15) | 0.6045 |
| Edema GoPg | |||||
| 12 hrs | 10.07(0.21) | 10.09(10.00-10.20) | 10.10(0.17) | 10.10(10.00-10.11) | 0.6039 |
| 24 hrs | 10.60(0.30) | 10.70(10.29-10.84) | 10.56(0.32) | 10.47(10.32-10.81) | 0.5234 |
| 48 hrs | 10.51(0.21) | 10.55(10.38-10.66) | 10.52(0.19) | 10.49(10.43-10.59) | 0.8265 |
| 72 hrs | 10.45(0.24) | 10.52(10.26-10.64) | 10.44(0.24) | 10.44(10.29-10.58) | 0.8904 |
| Edema GoAl | |||||
| 12 hrs | 10.67(0.37) | 10.63(10.40-10.93) | 10.69(0.37) | 10.70(10.50-10.84) | 0.8521 |
| 24 hrs | 11.01(0.37) | 10.96(10.72-11.27) | 11.02(0.37) | 11.03(10.82-11.16) | 0.8766 |
| 48 hrs | 11.13(0.37) | 11.08(10.85-11.39) | 11.15(0.37) | 11.15(10.95-11.29) | 0.863 |
| 72 hrs | 11.10(0.37) | 11.05(10.83-11.35) | 11.12(0.37) | 11.12(10.92-11.27) | 0.8413 |
| Trismus | |||||
| 0 | 51.2(4.8) | 50.0(47.5-53.5) | 51.7(0.9) | 50.5(48.5-55.5) | 0.6941 |
| 24 hrs | 40.3(5.4) | 40.0(37.0-43.5) | 40.3(0.9) | 39.0(37.0-44.0) | 0.8419 |
| 48 hrs | 40.9(6.8) | 40.7(37.0-46.5) | 41.9(0.9) | 41.5(38.0-45.0) | 0.9962 |
| 53 hrs | 44.7(5.8) | 45.1(40.0-49.0) | 44.7(1.0) | 44.0(40.0-49.1) | 0.9657 |
Note: p* values for nonparametric tests (Friedman test for dependent observations) ; Latency: Time required after local anesthesia was applied to start the incision without pain stimuli manifested by the patient; Time 1: Time taken to perform the actual extraction (time recorded after the latency period until the tooth is removed); Time 2: Time taken to perform the suture; GoT: Gonion point-tragus; GoEx: Gonion-Exocanthion; GoCh: Gonion-Cheilion; GoPg: Gonion-Pogonion); GoAl: Gonion-Alare; VAS: Visual Analogue Scale; DEXA: Dexamethasone; ETORI: Etoricoxib; SD: Statistical Difference.
Table 1: Distribution of outcomes (surgical time, pain, edema, trismus and analgesic rescue consumption) during the follow-up for surgeries preceded by Dexa or Etori treatment.
Pain assessment by the VAS
Although the bivariate analysis showed no statistical significance, there was an imbalance in treatment assignment for T38 and T48 and a possible influence of the right hand-sided operator on pain outcomes (VAS) (Figures 2A and 2B).
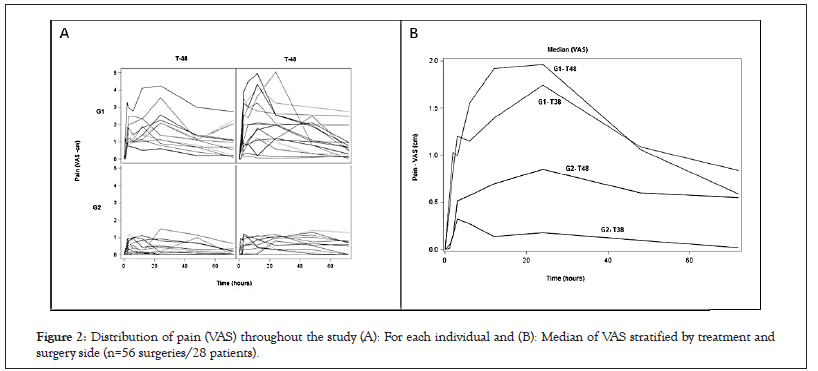
Figure 2: Distribution of pain (VAS) throughout the study (A): For each individual and (B): Median of VAS stratified by treatment and surgery side (n=56 surgeries/28 patients).
The final model for the effect of treatment on pain throughout the study adjusted for the side of the surgery and the order of treatment revealed a statistically significant effect of treatment and an interaction of treatment and surgical time (P<0.0001). This interaction is depicted in Figure 2B, which shows the change in median pain values over time. The interaction is represented by higher pain intensity in G1 up to the first 12 hours followed by a faster decline in pain after 24 hours, as compared to G2. Although the order of treatment was not statistically significant (P=0.2667), having surgery on the right side showed was associated with increased postoperative pain over time as compared to the left side (P=0.0002). Sex was not statistically associated with pain in the adjusted model (P=0.2667).
Administration of rescue analgesic
As observed in Table 1, the mean use of rescue analgesic tablets was higher in G1 than G2 (P<0.0001). A detailed description of the use of rescue analgesics by sex, side of the surgery, and the order of treatment, is presented in Table 2. Only 28.6% of the patients in G2 used rescue tablets as compared to 85.7% in G1 (Table 2).
| Total number of analgesic rescue | p* | ||||
|---|---|---|---|---|---|
| 0 | 1a3 | 4+ | |||
| n(%) | %(SE) | %(SE) | %(SE) | ||
| Sex | |||||
| Male | 20(35.7) | 64.7(10.0) | 23.5(9.3) | 11.8(7.9) | 0.1658 |
| Female | 36(64.3) | 40.6(6.8) | 31.2(10.1) | 28.1(6.9) | - |
| Treatment | |||||
| G1 | 28(50.0) | 14.3(6.7) | 46.4(9.6) | 39.3(9.4) | <0.0001 |
| G2 | 28(50.0) | 71.4(8.7) | 28.6(8.7) | 0(0.0) | - |
| Surgery side | |||||
| Left | 28(50.0) | 46.4(9.6) | 46.4(9.6) | 7.1(5.0) | 0.0557 |
| Right | 28(50.0) | 39.3(9.4) | 28.6(8.7) | 32.1(9.0) | - |
| Age(years) | |||||
| <=18 | 8 | 12.5(11.2) | 75.0(12.7) | 12.5(10.2) | 0.3266 |
| 19-20 | 20 | 50.0(10.2) | 25.0(10.8) | 25.0(8.0) | - |
| 20+ | 28 | 46.4(8.1) | 35.7(7.1) | 17.9(6.5) | - |
| Idade(left side) | |||||
| <=18 | 4 | 0.0(0.0) | 100(0.0) | 0.00(0.0) | 0.0063 |
| 19-20 | 10 | 70.0(14.8) | 30.0(14.8) | 14.3(6.5) | - |
| 20+ | 14 | 42.8(13.5) | 42.9(13.8) | - | |
| Idade(right side) | |||||
| <=18 | 4 | 25.0(22.2) | 50.0(25.5) | 25.0(22.5) | 0.5757 |
| 19-20 | 10 | 30.0(14.8) | 20.0(12.9) | 50.0(16.1) | - |
| 20+ | 14 | 50.0(13.6) | 28.6(12.3) | 21.4(11.7) | - |
Note: p*-value for wald chi-square considering the cluster effect within individuals. G1: Dexamethasone (4 gm); G2: Etoricoxib (120 mg); SE: Stable parameter.
Table 2: Distribution of consumption of analgesic rescue during the study.
Most patients who took the rescue analgesic tablet in GI did so after the third postoperative hour. In addition, the highest mean use of analgesics was in the first 24 hours. In G2, rescue tablets were more frequently used at the twelfth postoperative hour, when the registered pain score was the highest. The administration of four or more tablets was only observed among individuals in G1 (39.3%).
Patients undergoing impacted third molar surgery on the right side used the rescue medication more frequently than those submitted to left-side surgery, especially four or more tablets, even though it was not statistically significant (P=0.0557). Overall, age was not significantly associated with the use of rescue analgesic medication.
The risk analysis revealed that the overall probability of taking medication in G2 in the additive model was 3.1 (95% CI: 1.65– 5.49) fold higher than that of G1 (P<0.001), with virtually no effect of potential confounders. None of the potential confounders was statistically associated with the use of pain medication. However, our findings indicated that the youngest patients were 1.63-fold more likely to take the rescue tablet as compared to the oldest ones (Table 3).
| Total n(%) |
Drug Use % |
RR*crude(95% CI) | Model 1 | Model 2 | |
|---|---|---|---|---|---|
| RRadj(95% CI) | RRadj(95% CI) | ||||
| Sex | |||||
| Male | 20(35.7) | 35.3 | 1 | 1 | 1 |
| Female | 36(64.3) | 59.4 | 1.42(0.81-2.48) | 1.36 (0.82-2.24) | 1.33(0.83-2.22) |
| Age | |||||
| 23+(ref) | 28(50.0) | 43.6 | 1 | 1 | 1 |
| 20-22 | 20(35.7) | 50 | 0.93(0.55-1.57) | 0.93(0.55-1.57) | 1.12(1.71-1.77) |
| <20 | 8(14.3) | 87.5 | 1.63(1.09-2.44) | 1.63(1.09-2.44) | 1.74(1.12-2.70) |
| Surgery side | |||||
| Right | 28(50.0) | 53.6 | 1 | 1 | 1 |
| Left | 28(50.0) | 60.7 | 1.13(0.67-1.91) | 1.00(0.66-1.51) | 1.05(0.72-1.52) |
| Treatment | |||||
| G1 | 28(50.0) | 85.7 | 1 | 1 | - |
| G2 | 28(50.0) | 28.6 | 3.00(1.64-5.91) | 3.01 (1.65-5.49) | - |
| Surgery order | |||||
| First | 28(50.0) | 57.1 | 1 | 1 | - |
| Second | 28(50.0) | 57.1 | 1.00 (0.59-1.69) | 1.05 (0.72-1.52) | - |
| Treament / order | |||||
| G2 first(ref.) | 1.00(1.00-1.00) | ||||
| G2 second | 2.81(0.66-12.08) | ||||
| G1 second | - | - | - | - | 5.01(1.32-19.09) |
| G1 first | 6.58(1.71-25.26) | ||||
Note: RR*: Crude or adjusted relative risk and 95% Confidence Limits estimated using Poisson Regression with robust estimators taking into consideration cluster of treatments within individuals; Model 1: Additive model without interaction term; Model 2: Model with interaction term of treatment and order of surgery.
Table 3: Relative risk of taking analgesic rescue during the first 72 hours after the surgery.
Although potential confounders had a limited overall effect on the treatment, the test of interaction term revealed interesting behavior. Even though consumption of 4 pills or more was more frequent after surgeries on the right side (32.1%) vs. left side (7.1%), this difference was not captured in the model testing only any consumption of pain killers (RR=1.0; 95% CI: 0.59-1.69). However, when interaction (p=0.0992) was tested between treatment and the order of treatment there was a tendency of consuming more medication in the second surgery than in the first one.
Assessment of edema by the VAS and facial measures
Postoperative edema was assessed over time by the VAS scale and the use of facial measures. As shown in Figure 3A, the data distribution for the entire experimental period and medians indicated no significant influence of the side of the surgical procedure on edema outcomes. The effect of treatment on edema (VAS) overtime was also adjusted for sex, age, and side of surgery. The data indicated that the presence of edema in G1 was statistically higher than that in G2 throughout the study (P<0.0001). Moreover, the time of surgery was also an important factor in the model (P<0.0001) as well as an interaction between the time of surgery and treatment (P=0.0001). This interaction is probably due to the faster progression of edema in G1 than G2, especially in the first 24 hours as shown in Figure 3B. None of the potential confounders [sex (P=0.6002), side of the surgery (P=0.5662) or age (P=0.6002)] were statistically significant.
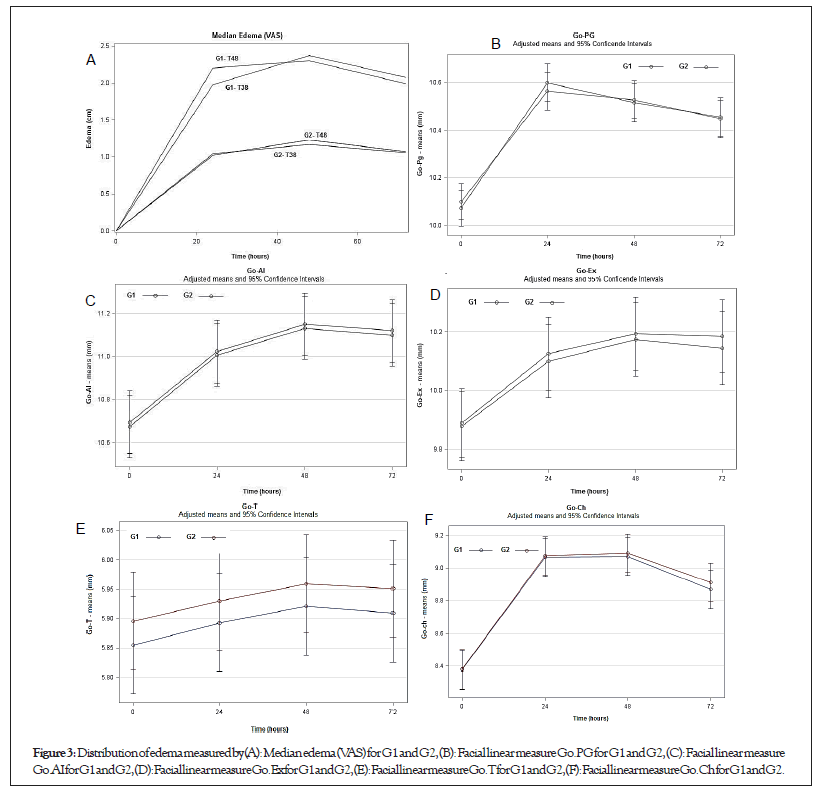
Figure 3: Distribution of edema measured by (A): Median edema (VAS) for G1 and G2, (B): Facial linear measure Go.PG for G1 and G2, (C): Facial linear measure Go.AIfor G1 and G2, (D): Facial linear measure Go.Ex for G1 and G2, (E): Facial linear measure Go.T for G1 and G2, (F): Facial linear measure Go.Ch for G1 and G2.
The distribution of facial edema (mean and 95% CI from the mixed-model analysis) for each facial measure over time revealed no overall difference between the treatments (P>0.70), although the presence of edema increased significantly over time (P<0.0001), especially in the first 24 hours (Figures 3A-3F).
Assessment of trismus
The mouth opening data had a normal distribution. No statistically significant differences in mouth opening measurements were observed between the groups (P=0.7037) after adjustment for sex, tooth, and age, and considering data dependency (Figure 4).
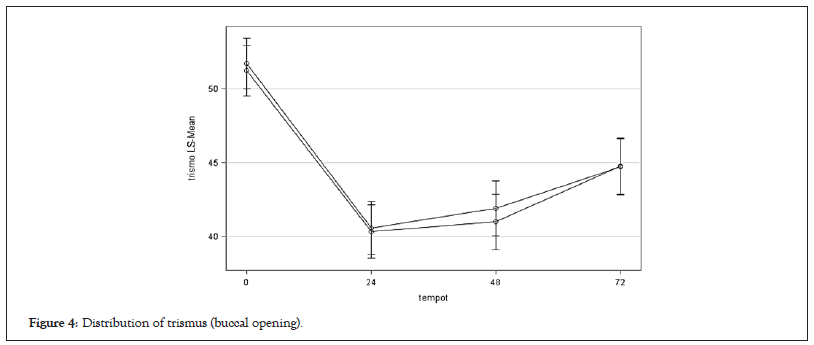
Figure 4: Distribution of trismus (buccal opening).
The clinical design used in our study is considered sensitive to determine the effects of anti-inflammatory drugs against acute inflammatory reactions triggered by the extraction of impacted mandibular third molars. Pain and inflammation are host responses to pro-inflammatory stimuli that are released in the event of a tissue trauma. Among other actions, these stimuli induce the production of an isoform of the enzyme Cyclooxygenase (COX) named COX-2, whose action on the arachidonic acid generates prostaglandins that mediate pain and inflammation. COX-2 also plays a role in the production of prostaglandins through the central nervous system, which increases pain sensitivity [28]. Both steroidal and non-steroidal analgesic drugs act by inhibiting the same chain reactions that degrade the phospholipids of injured cell membranes responsible for the allergic and inflammatory response [29].
Mandibular third molar surgery is commonly associated with significant postoperative discomfort and moderate to severe pain corresponding to 7 to 10 cm in the VAS [30,31]. De Menezes and Cury, et al reported that postoperative pain duration in mandibular third molar extraction ranges from short to moderate and reaches its maximum intensity after 12 hours [32]. Chopra, et al. reported that postoperative pain reaches a maximum intensity from 3 to 5 h after surgery and that it may continue for 2 to 3 days, and then gradually diminishes until the 7th day [33]. The peak of edema occurs after 12 to 48 hours and resolves only between the 5th and 7th days [34,35]. As a result, pharmacological strategies have been used to control pain, edema, and trismus after traumatic extractions. However, the scientific community proposes to investigate analgesic/anti-inflammatory drugs to establish a drug protocol that has maximum effectiveness in reducing the expected discomfort and enable the patient to return to normal functions as early as possible [36].
Dexamethasone and methylprednisolone are the corticosteroids most used for preemptive analgesia in third molar surgery [37]. The efficacy of preemptive analgesia with the use of corticosteroids and NSAIDs was demonstrated in previous studies comparing with a placebo or different doses of the drug. However, there is no consensus in the literature on which medication is the most effective when used preventively to decrease postoperative pain in these surgical procedures. Other studies also present controversial results with the use of anti-inflammatory drugs [38,39].
There are only a few comparative studies between COX-2- selective NSAIDs and corticosteroids, we compared the effects of 4 mg dexamethasone and 120 mg etoricoxib-administered in a single dose in the immediate preoperative period-on pain, edema, and trismus outcomes following the extraction of impacted mandibular third molars. The choice for the dexamethasone dose of 4 mg was based on the study by Agostinho, et al. which analyzed the efficacy of two doses of dexamethasone (4 mg and 12 mg) for the control of pain, edema, and trismus after third molar surgery and observed no significant difference (a=0.05) between them [40].
As for etoricoxib, in a previous randomized, placebo-controlled, double-blind, single-center study with a third-molar extraction model, 120 mg etoricoxib was shown to be the minimum dose that had maximal efficacy in patients with moderate to severe pain associated with dental surgery [41,42]. Etoricoxib was shown to be a single-dose oral drug with greater efficacy than other commonly used analgesics [43]. The choice for etoricoxib, which has a half-life of approximately 25 hours, was because it reaches maximum intensity around 3 to 12 hours after surgery, which could potentially reduce the need for rescue analgesics in the postoperative period [44].
In our study, patients who received either dexamethasone or etoricoxib presented only mild postoperative pain (with mean VAS values of 1.3622 and 0.3777 for G1 and G2, respectively). The VAS measurements showed that etoricoxib controlled pain significantly better than dexamethasone. From the 2nd postoperative hour and throughout the experimental period, G1 patients presented greater pain symptomatology. However, there was higher pain intensity in G1 until the first 12 hours, followed by a faster decline after 24 h, as compared to G2. The significant reduction in pain levels in G1 after one day was probably due to the use of rescue medication. G2 did not show any significant differences in postoperative pain levels, with only mild pain and a lower consumption of rescue analgesic tablets. Thus, as compared to the peak of pain observed in G1 (12 h), etoricoxib was 3.6-fold more potent for pain control than dexamethasone. Therefore, the reduction of pain in G1 from the first 24 hours associated with a decline in the use of rescue analgesics suggests that the anti-allergic effects of dexamethasone were less expressive than those of etoricoxib.
Glucocorticoids are effective for the control of acute and chronic inflammation by interfering in different pathways of the inflammatory response and leading to a decrease of inflammatory mediators at the site of injury. Suppressing each stage of the inflammatory response appears to be the primary mechanism of action of corticosteroids-cell recruitment (vasodilation and diapedesis), inhibition of granulation tissue formation, and inhibition of enzyme secretion (phospholipase, collagenase, and elastase) and pro- inflammatory mediators (prostaglandins and prostacyclins) [45]. Dionne, et al. evaluated in vivo the relationship between prostanoid levels at the injured tissue site after extraction of third molars and analgesia after administration of 4 mg of dexamethasone [46]. They observed that analgesia in the immediate postoperative period was not seen under the administration of 4 mg of dexamethasone, confirming the statements of Troullos et al. [47]. PGE2 suppression by dexamethasone was inadequate to prevent sensitization of the peripheral nociceptors involved in the mechanism of pain production. The use of corticosteroids is palliative rather than curative, given that it aims to decrease the severity of symptoms that the patient may experience [48]. The use of corticosteroids in different doses proved to be effective in controlling swelling and trismus. The reduction of trismus and inflammation due to third molar surgery and the beneficial effects seem to be greater when corticosteroids are administered preoperatively compared to their postoperative use.
NSAIDs reduce peripheral levels of PGE2 and produce analgesic effects via other mechanisms independent of the suppression of peripheral prostanoid levels. Several studies have evaluated the effects of NSAIDs administered preoperatively and postoperatively on third molar extractions [49-51]. Among them, Costa, et al. [20] showed that etoricoxib significantly reduced pain levels after impacted third molar surgery and the need for rescue medication compared to the placebo.
In our study, preemptive administration of 4 mg of dexamethasone did not allow an effective control of postoperative pain, although the recorded pain intensity was mild, yet statistically significant in the postoperative period. Numazaki and Fujii observed that doses of 8 mg of dexamethasone administered prophylactically in third molar extraction allowed better control of postoperative pain compared to 4 mg of dexamethasone and placebo [52]. Nevertheless, Agostinho, et al. [40] showed no significant differences (a=0.05) in the study outcomes between the two doses of dexamethasone (4 and 12 mg) (Student's t, Wilcoxon, and Friedman tests).
Evidence-based medicine has shown that NSAIDs are the best analgesic choice for dental pain [53]. NSAIDs act by inhibiting Cyclo-oxygenase (COX) enzymes that catalyze the conversion of arachidonic acid into prostaglandins, which are fatty acids involved in the generation of pain, inflammation, and fever [54]. Our results are in agreement with the reports of Ong and Seymour [53], especially the prophylactic analgesic protocol (preemptive dose).
Even though we are aware that the practice of starting pre- operative analgesic drugs is particularly controversial, we believe that postoperative pain can be prevented almost entirely through analgesic premedication, as demonstrated by Esteller-Martínez, et al. [55]. As also mentioned by Orozco-Solis, et al. [14], the medication was provided on a prophylactic basis-before the onset of pain and for ethical reasons, since we assumed that all patients would present postoperative pain because all surgeries involved a significant degree of tissue trauma.
Overall, the number of rescue analgesic tablets used in the postoperative period was low (mean of 3.43 tablets). Of the 96 rescue tablets used by patients in G1, 61 (63.54%) were administered in the first 24 h, as compared to 7 out of 12 (58.33%) in G2. In the first 12 h, G1 patients experienced pain more frequently, with a higher average of use of rescue analgesic. In the same observation period, patients in G2 experienced pain less frequently and used fewer rescue analgesics than those in G1. This indicates that etoricoxib was 3.6-fold more potent than dexamethasone since rescue analgesics were also available to patients in the two sessions for use in case of severe pain. There was no record in the VAS of severe pain (7 cm-10 cm). Only one patient presented pain recorded by the VAS above 4.3 cm (volunteer 15). According to the World Health Organization (WHO) pain scale, values below 3 indicate weak pain and above 3, moderate pain [56,57].
The analysis of patients who experienced acute postoperative pain showed that most of them had pain relief in both groups. Importantly, etoricoxib allowed significant postoperative pain control since most patients (71.4%) who underwent dental extractions did not take any rescue analgesic tablet and experienced only mild pain in the postoperative period. According to Moore et al. describing the proportion of patients with a clinically significant response is more informative than describing the mean values of pain obtained in the treatment groups [58]. In addition, achieving 50% or more of pain relief meets the Minimum Effectiveness Criterion 50 (MEC50). In a previous study, Sotto-Maior, Senna, Assis [35] compared the use of dexamethasone and etoricoxib in the control of pain and edema after surgery of mandibular third molars. The authors examined painful symptoms in the preoperative baseline and 24 and 48 hours postoperatively. However, this assessment model regrettably does not identify the first time when rescue analgesics were taken and the peak of pain in the first postoperative hours.
One can question the surgical complexity of the extractions in the present study, which could generate different tissue trauma in the volunteers. We note that our inclusion criteria consisted of young patients with mandibular third molars having similar mesioangular and vertical positions, as well as similar angles and degrees of impaction. Thereby, we could estimate a similar surgical trauma. However, some authors believe that surgical complexity cannot be estimated preoperatively using radiographs but it is best performed in the trans-operative period [59]. It has been suggested that patient factors also have a major impact in increasing the difficulty of third molar surgery, in particular, age, sex, height and ethnicity, but only age was previously related to increased surgical time and complications [60-62]. Currently, great emphasis is given to dental variables when teaching about the complexity of the third molar surgery. For experienced surgeons, it is evident that patient variables may also have a strong influence on the complexity of third molar surgery, which encouraged the study of Renton, Smeeton, and McGur [63].
Several studies reported by Renton, Smeeton, McGur [63] and other authors showed surgical times for third molar surgery ranging from 7.57 min to 105 min [64, 65]. The duration of surgery depends on several factors, including surgical difficulty, surgeon’s experience, surgical technique, and how time was measured. The mean surgical time of extraction (time 1) of 17.7 (G1) and 18.5 (G2) is similar to that reported in the literature [66].
In our study, edema was self-assessed by the VAS and through the linear facial measures by Neupert from 24 to 72 hours postoperatively as compared to baseline data. Some authors have reported that the peak of edema occurs within 14 to 48 hours after surgery and that it only resolves between the 5th and 7th days. In the present study, greater VAS values for edema were recorded from 24 hours to the maximum evaluation period (72 hours), reaching a peak of edema after 48 hours in both groups. VAS measurement demonstrated that the patient perceives a change in their facial volume. Patients receiving 4 mg of dexamethasone had a greater perception of edema by the VAS as compared to those who received 120 mg etoricoxib, although the analysis of facial measures did not show any significant intra and intergroup differences. It is believed that the poorer pain control of dexamethasone caused patients, through discomfort, to identify a greater facial variation in the self-assessment (VAS). Edema outcomes changed over time and no measurement had returned to baseline levels after 72 hours postoperatively. Costa, et al. [20] found that groups treated with etoricoxib and a placebo, showed a peak of edema after 24 hours and that the reduction of swelling was only significant from the 5th to the 7th postoperative day. Therefore, etoricoxib did not show any significant anti- inflammatory effect on edema compared to the placebo group.
Sotto-Maior, Senna and Assis [35] did not observe a significant difference in edema with the preventive use of etoricoxib compared to dexamethasone. In addition, these authors observed an increase in facial edema during the first 48 h after surgery. It is important to note that facial edema is difficult to quantify accurately since the facial surface is irregular and convex. In addition, the same amount of edema may occur internally or externally, depending on the facial area involved, and it may be or not noticeable, which renders the comparison a challenging task [67].
Considering that edema develops with the surgical trauma and reaches its peak approximately 48 h after the operation, the half-life of the preemptive drug is a critical factor to consider. Dexamethasone, a long-acting steroid, may be effective between 36 h and 54 h [68] and etoricoxib has a half-life of approximately 25 hours. Another reason for the difference may be the dose of dexamethasone used in the present study (4 mg). Doses of 4 mg, 8 mg, or 12 mg of dexamethasone have already been used and the results are different and contradictory. While Laureano Filho, et al. [12] demonstrated that 8 mg of dexamethasone was more effective than 4 mg to reduce edema and trismus in mandibular third molar extractions, Agostinho, et al. [40] did not find any differences in edema, pain, and trismus at preemptive doses of 4 mg or 12 mg. The efficacy of oral administration of dexamethasone compared to other anti- inflammatory drugs (steroidal and non- steroidal) during mandibular third molar surgery was evaluated in a systematic review by Falci, et al. [23]. Despite the few studies evaluating the preemptive analgesic efficacy of dexamethasone compared to other types of anti-inflammatory drugs, as well as the high level of heterogeneity between the studies, dexamethasone may be indicated as an effective anti-inflammatory based on the results presented in the analysis. The authors pointed out that of the seven studies included in the analysis, three showed a low risk of bias, including the study by Agostinho, et al. [40]. Two had a moderate risk of bias because they did not provide adequate information about sample randomization and the last two studies exhibited a high risk of bias because they did not adequately report sample randomization or sample losses or the study follow-up protocol. Studies that showed a high risk of bias compared 4 mg and 8 mg dexamethasone 12 and dexamethasone with etoricoxib [35]. Therefore, the results of these studies should be evaluated with caution. The other study comparing 4 mg and 12 mg dexamethasone did not find differences between the two doses [40]. Therefore, we agree with the statement by Falci, et al. [23] that the ideal concentration of dexamethasone for preemptive analgesia remains unclear.
All patients in the study by Balakrishnan, et al. [24] experienced a peak of reduced mouth opening during the first and second postoperative day, which was due to tissue inflammatory reaction and perceived pain. Of the 50 patients participating in their study, 43 gradually recovered the mouth opening after the 5th postoperative day and returned to preoperative measurements in 7 days. The other seven patients presented persistent reduction of mouth opening up to the 7th day due to the severity of pericoronaritis associated with the impacted third molar. In our study, one patient in G1 had normal mouth opening within the 72-hour postoperative period, and no patient in G2 returned to preoperative levels. Our findings showed that trismus was similar in both groups over time.
Several factors may be related to a reduced mouth opening. Trismus is caused by the edema associated with the tissue trauma resulting from the extraction or multiple punches during infiltration of the local anesthetic. In addition, the injected volume of the local anesthetic solution may cause a stretching of the medial pterygoid and initiate a spasmodic contraction [69]. Another factor that plays a role in mouth opening measurements is the section of the lower part of the tendon of the temporal muscle when the distal-buccal bone that covers the molar crown is removed. In addition, during retraction of buccal flaps, a downward and/or buccal traction with the retractor may lacerate the periosteum in the flap or extend the flap base beyond the outer oblique line, leading to increased pain, swelling, and trismus. If any muscle is damaged, a pain reflex is stimulated. This condition is called "muscle-guarding" and occurs when muscle fibers are elongated and provoke pain. The pain causes the muscles to contract, resulting in loss of range of motion. Thus, studies testing several doses of anti-inflammatory drugs are encouraged to control the mechanisms associated with the onset of trismus after impact mandibular third molar extraction.
Knowing that the inflammatory process after the trauma caused by tooth extraction can be preventively reduced with anti- inflammatories, the antialgic role attributed to etoricoxib was evident since both the pain record and the number of auxiliary analgesics consumed were smaller, although the pain recorded by the patients it was considered mild. As for the anti-inflammatory behavior, both drugs allowed similar records of self-assessment of edema (measured by VAS) and records of changes in facial volume (facial measures).
Considering the methodology employed in the study, it is concluded that our findings indicated that etoricoxib (120 mg) was more effective in controlling postoperative pain than dexamethasone (4 mg) and that both drugs were comparable for the control of edema and trismus.
The authors have no relevant financial or non-financial interests to disclose.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Google scholar] [PubMed]
[Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Villela GA, Mariano RC, de Menezes PHM, Saraiva MCP, Antoniali C (2023) Does Etoricoxib or Dexamethasone Control Inflammatory Pain, Edema, and Trismus After Impacted Third Molar Surgery? A Double-Blind, Split- Mouth Randomized Clinical Trial. J Anesth Clin Res.14:1106
Received: 30-May-2023, Manuscript No. JACR-23-23616; Editor assigned: 01-Jun-2023, Pre QC No. JACR-23-23616 (PQ); Reviewed: 15-Jun-2023, QC No. JACR-23-23616; Revised: 22-Jun-2023, Manuscript No. JACR-23-23616 (R); Published: 29-Jun-2023 , DOI: 10.35248/2155-6148.23.14.1106
Copyright: © 2023 Villela GA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.