Journal of Antivirals & Antiretrovirals
Open Access
ISSN: 1948-5964
ISSN: 1948-5964
Research Article - (2021)Volume 13, Issue 3
Background: We depicted the survival rate of the patients with coronavirus disease 2019 (COVID-19). We focused on the patients who were detected lately after symptom development. The aim is to determine the socio-demographic risk factors associated with the delaying detection of COVID-19 patients.
Methods: We selected 300 COVID-19 patients from May to July 2020 for this cross-sectional study in the Molecular Biology Laboratory of Chittagong Medical College, Chattogram, Bangladesh.
We recorded clinical characteristics from over phone interviews and laboratory diagnosis by Real-time Reverse Transcriptase Polymerase Chain Reaction (rRT-PCR). We applied the Cox proportional hazard model to estimate risk factors affecting the delaying detection of COVID-19 patients.
Results: The female mortality rate was 44.9% higher compared to males. The graduates died 32% more than undergraduates, and unmarried peoples’ death rate was 56% more than married. Besides, those who traveled irregularly and in contact with symptomatic patients were 86% more died than non-travelers.
Conclusion: Early diagnosis of COVID-19 can save enormous life, and it should emphasize special attention on the significant explanatory variable.
COVID-19; Survival analysis; Delay of detection
COVID-19: Coronavirus Disease 2019; rRT-PCR: Real-time Reverse Transcription-Polymerase Chain Reaction; SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; MERS-CoV: Middle East Respiratory Syndrome Coronavirus; ICU: Intensive Care Unit; WHO: World Health Organization; PPE: Personal Protective Equipment; LML: Log-Minus-Log; CI: Confidence Interval; SE: Standard Error; df: Degrees of freedom; Exp(B): Odds ratio.
The Severe Acute Respiratory Syndrome (SARS-CoV) and the Middle East respiratory syndrome (MERS-CoV) strengthened as pathogens in the last two decades, both on humans and animals [1,2]. In December 2019, the outbreak of an emerging disease began in Wuhan, China, and spread rapidly in China and abroad. They caused over 50% mortality by respiratory tract infection, including extrapulmonary complications.SARS-CoV-2 was first identified last December by the "Chinese Centers for Disease Control and Prevention" [3,4].
Current studies show that SARS-CoV-2 can transmit person-toperson through respiratory droplets in closed containment [5,6]. The World Health Organization (WHO) reported it as a health crisis on 30 January 2020 and titled the disease caused by this virus Coronavirus Disease-19 (COVID-19) on 11 February 2020. As of 31 July 2020, the number of patients has outgo 2,54,474 globally, and more than 6002 have now expired of COVID-19.
It depicted SARS-CoV-2's genome sequence identical to SARS-CoV, which is 79.5%. Interestingly, SARS-CoV-2 was 96% analogous to a bat coronavirus in the whole-genome sequencing [7].
From clinical characteristics and pathological dimensions, fatalpneumonia causes high mortality [8]. To keep going with this economic breakdown, maximum family members went outside of their homes to earn money. Regular household necessities bought by them from crowded markets in this pandemic situation. Besides, a long period of home restrictions made them unsteady to breathe fresh air, as a result, affected by COVID-19. But initially, symptoms were mild, and especially the young generation was unwilling to maintain healthy hygiene and follow restrictions. We tried to identify the hazard of late detection time of COVID-19 of those patients in our study.
The molecular biology laboratory of Chittagong Medical College conducted a cross-sectional study on 300 COVID-19 patients from May 2020 to July 2020. Reverse Transcriptase-Polymerase Chain Reaction was performed by the QuantStudio 5 Real-Time PCR instrument (96-Well 0.2 ml Block) by Sansure Biotech Novel Coronavirus (2019-nCoV) Nucleic Acid Diagnostic Kit (PCRFluorescence Probing).
Patients with a SARS-CoV-2 infection confirmed by an rRT-PCR of a nasopharyngeal and oropharyngeal combined sample within 3 days of onset of symptoms included in the study. Presence of symptoms, days of illness, contact with symptomatic patient/health personnel, types of PPE used, traveling history, supplemental oxygen therapy requirement, hospital admission history, ICU support requirement, co-morbid conditions, baseline investigations, and prescription collected by the research team through interviewing over the phone.
The WHO website has provided several rRT-PCR protocols for detecting SARS-CoV-2 in different countries [9]. Here an automated system repeated the amplification process for about 45 cycles until we could detect the viral cDNA, usually by a fluorescent signal from different channels such as FAM, ROX, and CY5. We considered the SARS-CoV-2 open reading frame-ORF 1ab, and the specific conserved sequence of coding nucleocapsid protein N gene as the target regions for the conserved sequence of the double-target genes to achieve detection of sample RNA through FAM and ROX signal changes, respectively. CY5 signal detected internal standard gene fragments (Rnase P). Here a single tube contained the specific primers, probes, dNTPs, MgCl2, Rnasin, PCR buffer, RT enzyme, and Taq enzyme to run the entire RT-PCR reaction (24 tests/kit). We fixed positive internal control to monitor PCR inhibitors in test specimens and normal saline as a negative control. We sorted 300 SARS-CoV-2 positive patients for our study. These respondents gave us complete history and relevant data.
Cox proportional hazard model (1972) is a well-admired model used in survival analysis [10]. It can assess the importance of various covariates in the survival time of individuals through the hazard function. It makes us capable of estimating the relationship between the hazard rate and explanatory variables without having assumptions on the shape of the baseline hazard function. In our study, the cox proportion hazard model was used to analyze the factor affecting COVID-19 patients’ mortality because of late diagnosis by considering any extra heterogeneity present in the data. We used the log-rank test to test the equality of the hazard function. Our testing null hypothesis was all the survival curves were the same. To explore the relationship among factors having multiple-categories, we applied the Bonferroni test.
This study described 300 patients with confirmed COVID-19 from May 09, 2020, to July 12, 2020, in Molecular Biology Laboratory, Chittagong Medical College, Chattogram.
In the above Table 1, censored were those who were alive during the study period, whether he/she was in isolation at home or the hospital. We found 1% of females, 9% of males, were not alive at a p=0.006 level of significance. 0.7% of health professionals and service holders died. We found 1% of students deceased only in the study period. In contrast, the people related to the ‘others’ profession 7.7% died, which is much more.
| Backgroud characteristics | Catagories | Censored | Condition of patients (Died) | Log rank (Mantel-cox) | df | p-value | |
|---|---|---|---|---|---|---|---|
| Sex | Female | 87(29.0%) | 3(1.0%) | 7.675 | 1 | 0.006* | |
| Male | 183(61.0%) | 27(9.0%) | |||||
| Education | Undergraduate | 96(32.0%) | 15(5.0%) | 1.632 | 1 | 0.201 | |
| Graduate | 174(58.0%) | 15(5.0%) | |||||
| Occupation | Health personnel | 16(5.3%) | 2(0.7%) | 5.764 | 3 | 0.124 | |
| Service holder | 49(16.3%) | 2(0.7%) | |||||
| Student | 57(19.0%) | 3(1.0%) | |||||
| Others | 148(49.3%) | 23(7.7%) | |||||
| Place of residance | Urban | 195(65.0%) | 9(3.0%) | 5.086 | 1 | 0.024* | |
| Rural | 75(25.0%) | 21(7.0%) | |||||
| Marital status | Unmarried | 60(20.0%) | 0(0.0%) | 1.025 | 1 | 0.311 | |
| Married | 210(70.0%) | 30(10.0%) | |||||
| Age | 0-18 | 20(6.7%) | 1(0.3%) | 1.221 | 3 | 0.748 | |
| 19-39 | 90(30.0%) | 3(1%) | |||||
| 40-59 | 94(31.3%) | 14(4.7%) | |||||
| 60 and above | 66(22.0%) | 12(4.0%) | |||||
| Family member's affected or not | Not affected | 135(45.0%) | 21(7.0%) | 11.688 | 1 | 0.001* | |
| Affected | 135(45.0%) | 9(3.0%) | |||||
| Travelling history | Contact with symptomatic patient | 114(42.7%) | 3(1.1%) | 17.788 | 2 | 0.000* | |
| Travelling regularly | 90(33.7%) | 9(3.4%) | |||||
| No travelling history | 36(13.5%) | 15(5.6%) | |||||
Note: (*) Indicates variable is the significance level at % level of significance
Table 1: Distribution of survival status along with the log rank test with the selected variables.
Rural patients died 7%, where urban people were only 3% (p=0.024). The death of married persons was 10%. Middle-aged adults had a 4.7% death rate, but only 0.3% of children died. The unaffected family member group had 7% of death with the 0.001 level of significance than the affected family member group. Surprisingly, 5.6% of patients died (p=0.000) those who had no traveling history.
For testing the proportional hazard assumption, we checked whether the independent variables meet the proportional assumption by using a log-minus-log (LML) plot. The LML plot is a graph constructed by applying the log-log transformation of the survival function. It is a graph of the logarithm of time against the logarithm of the negative logarithm of the estimated survival function. In Figure 1 we have seen that curves of each risk factor are not crossing but they are parallel. That means all the risk factors defined properly and satisfied the proportional hazard (PH) assumptions.
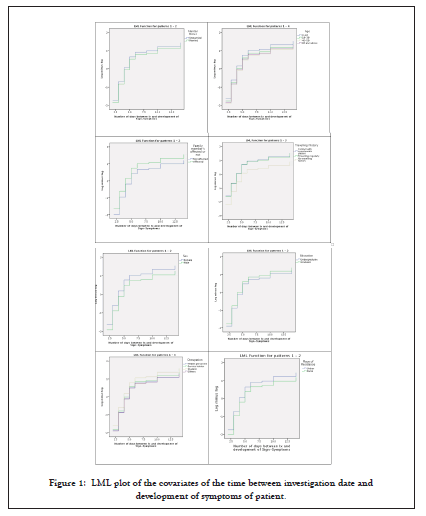
Figure 1: LML plot of the covariates of the time between investigation date and development of symptoms of patient.
From Table 2, female mortality (hazard) rate was 44.9% higher ((p=0.009) CI (9%, 91%)) compared to the male. The factor education was likely to have in more hazardous conditions; graduate entities were likely to 1.316 times higher (CI (1.000, 1.732)) risk compared to undergraduate. Students were 1.353 times more (CI (.995, 1.840)) in hazard than ‘others’ category.
| Variables | Categories | B | SE | df | Sig. | Exp(B) | 95.0% CI for Exp(B) | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Sex | Female | 0.371 | 0.142 | 1 | 0.009 | 1.449 | 1.097 | 1.915 |
| Male | 1.000 | |||||||
| Education | Undergraduate | 1 | 1.000 | |||||
| Graduate | 0.275 | 0.140 | 0.050 | 1.316 | 1.000 | 1.732 | ||
| Occupation | Health personnel | 0.022 | 0.264 | 3 | 0.933 | 1.022 | 0.610 | 1.714 |
| Service holder | 0.101 | 0.165 | 0.543 | 1.106 | 0.800 | 1.529 | ||
| Student | 0.303 | 0.157 | 0.054 | 1.353 | 0.995 | 1.840 | ||
| Others | 1.000 | |||||||
| Place of residance | Urban | 0.249 | 0.137 | 1 | 0.069 | 1.283 | 0.981 | 1.678 |
| Rural | 1.000 | |||||||
| Marital status | Unmarried | 0.444 | 0.239 | 1 | 0.064 | 1.559 | 0.975 | 2.492 |
| Married | 1.000 | |||||||
| Age | 0-18 | 3 | 1.000 | |||||
| 19-39 | 0.126 | 0.260 | 0.629 | 1.134 | 0.681 | 1.890 | ||
| 40-59 | -0.012 | 0.162 | 0.005 | 0.988 | 0.719 | 1.358 | ||
| 60 and above | -0.084 | 0.162 | 0.267 | 0.920 | 0.670 | 1.263 | ||
| Family member's affected or not | Not affected | -0.336 | 0.122 | 1 | 0.006 | 0.715 | 0.563 | 0.908 |
| Affected | 1.000 | |||||||
| Travelling history | Contact with symptomatic patient | 0.621 | 0.192 | 2 | 0.001 | 1.860 | 1.277 | 2.710 |
| Travelling regularly | 0.591 | 0.199 | 0.003 | 1.807 | 1.223 | 2.669 | ||
| No travelling history | 1.000 | |||||||
Table 2: Estimated hazard ratio obtained from cox proportional hazard model.
The residents of urban areas were in 1.283 times (CI (.981, 1.678)) high-risk zone than the rural residents. Unmarried were 1.559 times (CI (.975, 2.492)) riskier for death than married persons. 19-39 year’s age group patients were 1.134 times (CI (0.681, 1.890)) more in hazardous context than 0-18 year’s age group. The unaffected family members' patients were 0.715 times (CI (0.563, 0.908)) less in risk than the affected family members' patients. Besides, the patients who were in contact with symptomatic patients were 86% more in hazard ((p=0.001) CI (28%, 71%)) than those who had no traveling history during this pandemic.
Delay of detection of COVID-19 plays a significant role in this survival analysis regarding the patient's status: he/she survived or not. By the cox proportional hazard model, we explored the hazard rate of several risk factors and explained the odds ratio. From this study, female (1.499 times) participants and graduates (1.316) were in more risky positions compare to other participants. The Students (1.353) were in more vulnerable positions, however, the service holders and the health and personnel were at low risk. The urban (1.283 times more affected) and the unmarried (1.559 times more affected), should be more careful as they both at high risk to befall in COVID-19. We should avoid traveling because the people who travel regularly were 1.807 times at high risk. Besides, it should restrict contact with symptomatic patients, as they were 1.860 times more vulnerable because of traveling.
This research has some limitations. First, SARS-CoV-2's information limited. Second, the information provided here based on current evidence only. Third, the sample size was small.
Late detection of COVID-19 can cause serious health hazards. Besides, its outcome is significantly worse than those who have comorbidities. Concomitantly it exacerbates the death of a patient. So, early earnestness to identify the SARS-CoV-2 virus and taking prompt treatment can save many lives.
Case record forms were approved by the Ethical Review Committee of the Chittagong Medical College and Hospital, Chattogram, Bangladesh, and written informed consent was obtained from each participant. No additional ethical approval is needed.
Our manuscript was approved the consent for publication from Department of Microbiology, Chittagong Medical College.
The data sets are available from the corresponding author on reasonable request.
The authors declare no conflict of interest.
This research received no external funding.
Sujan Rudra: Database management and statistical analysis; Shuva Das: Conceptualization, writing-original draft preparation; Md. Ehsanul Hoque: Writing-review and editing, supervision; Abul Kalam: Investigation and validation; Mohammad Arifur Rahman: Methodology and investigation; The authors read and approved the final manuscript. Sujan Rudra and Shuva Das can be treated as correspondence authors and equally contributed.
We thank all of the medical and ancillary hospital staff and the patients for consenting to participate. We would like to thanks the editors and referees whose constructive criticism led us to develop the presentation and maintain the quality of the paper. We would also like to thanks the Molecular Biology Laboratory of Chittagong Medical College, Chattogram, to give us almost all the opportunity for conducting the research.
Citation: Rudra S, Das S, Hoque ME, Kalam A, Rahman MA (2021) Delay of Detection of COVID-19 Patients in Bangladesh, An Application to Cox Proportional Hazard Model. J Antivir Antiretrovir. 13:218.
Received: 01-Feb-2021 Accepted: 15-Feb-2021 Published: 22-Feb-2021 , DOI: 10.37421/1948-5964.21.13.218
Copyright: © 2021 Rudra S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.