
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 4
Background: The most challenging aspect for the anesthesiologist in case of requiring general anaesthesia is the insertion of a Tracheal tube. Airway management and endotracheal intubation are fundamental skills for the safe conduct of anaesthesia. Despite of popularity of Macintosh laryngoscope in routine surgeries, failures during intubation are not uncommon, especially in patients with unanticipated difficult airway. Recent advances gives opportunity with development of video laryngoscope which does not require alignment of the oral-pharyngeal-laryngeal axes that may reduce the difficult in endotracheal intubation. So in this study, we compared Hemodynamic parameters and duration of Intubation between Macintosh laryngoscope and Truview video laryngoscope. Review Video laryngoscope is device with unique blade which provides 42° anterior reflected view of larynx and glottis without alignment of oral pharyngeal laryngeal axes.
Objectives: A type of prospective Double blind Randomised controlled trial carried out at tertiary care unit during 2020- 2021 with 60 adult patients, after taking approval of Institutional Ethical Committee(Ref no. IEC/Certi/223/06/2020) and written informed consent in their own language according to institutional protocols and explaining the cause, pathology and consequences of the process.
Methods: In this Prospective, Randomized controlled study on 60 patients of 18 to 60 years of age and either sex after matched inclusion criteria with American society of Anesthesiologists class I, II and III, who were posted for elective surgery requiring general Anaesthesia with endotracheal intubation. Patients are equally divided in to two groups, Group M (n=30) and Group T (n=30), in which intubation was done using Macintosh laryngoscope and Truview Video laryngoscope respectively. Duration of intubation and Hemodynamic Parameters were measured at different time interval. Statistical analysis was done by using SPSS Statistical Software version 24.0. Mean and standard deviation were calculated. Unpaired ‘t’ test were applied between Group M and Group T. p value of <0.05 is considered statistically Significant and p value<0.001 was considered statistically highly significant.
Results: Truview Video laryngoscope make easiear intubatrion as compared to Macintosh laryngoscope, But total duration of intubation was more with Group T (38.16 ± 4.47 seconds) as compared to Group M (14.66 ± 4.02 seconds) which was statistically Highly Significant (p value<0.001). There was fewer rises in hemodynamic parameters with Truview Video laryngoscope as compared with Macintosh laryngoscope.
Conclusion: Truview Video laryngoscope provides easier intubation and better hemodynamic stability. But duration of intubation was more with Truview Video laryngoscope as compared to Macintosh laryngoscope.
Macintosh laryngoscope; Truview video laryngoscope; General Anaesthesia
Airway management and endotracheal intubation are fundamental skills for the safe conduct of Anaesthesia practice. In general Anaesthesia with endotracheal intubation, the most challenging aspect for the Anesthesiologist is the insertion of an endotracheal tube. Video laryngoscopes offer easy intubation and in addition, some of them offer to record the intubation procedure [1]. Macintosh laryngoscope is the most popular laryngoscope in this time, but failures during intubation are common in patients with unanticipated difficult airway (1.5%-8.5% of all general anaesthesia). Better laryngoscopes are being designed in an effort to reduce the incidence of unpredicted complications in such patients but their clinical efficacy and practical application in operating rooms still pending for approval [2]. The recent development of a number of indirect video laryngoscopes which does not require the oral-pharyngeal-tracheal axes alignment, thus they may reduce the difficulty of endotracheal intubation in unanticipated difficult airway. Two relatively low cost indirect laryngoscopes, Airtraq and the Truview video laryngoscope which could be easily included in ambulance equipment inventories [3]. Direct laryngoscopy can cause arterial hypertension and tachycardia due to proprioceptor stimulation of the supraglottic structures. As Macintosh laryngoscope requires a considerably more lifting force to align oro-pharyngeeal axes, many adverse hemodynamic changes can occur during direct laryngoscopy [4]. Present study was done to compare Duration of intubation, hemodynamic stability and ease of intubation between these two laryngoscopes.
After the Institutional Ethics Committee's approval and written informed consent of patient in their own vernacular language, This Prospective Randomized, single blind study was conducted on 60 patients of 18 to 60 years of age, either sex, ASA grade I, II and III and BMI between 18.5 to 29.9kg/m2 who were posted for elective surgery requiring general Anaesthesia with endotracheal intubation. Patients having upper respiratory tract infection, coughing, cardiopulmonary disease, coagulopathies, raised intracranial tension, BMI more than 30kg/m2, ASA grade IV and V, predicted difficult airway, head and neck, pathology and patient undergoing emergency surgeries are excluded. All patients were informed and made to understand the details of entire anesthetic procedure during preoperative visits in preoperative area. Patients are equally divided in to two groups, Group M and Group T (30 patients in each), intubation was done using Macintosh laryngoscope and Truview Video laryngoscope respectively. Laryngoscopy and intubation were carried out by the same experienced anesthesiologist in both groups. As pre anaesthetic evaluation was done on the previous day of surgery and was reviewed on the day of surgery. A detailed medical and surgical history was taken. Systemic and General Examination was carried out and relevant investigations were advised. The purpose and procedure of the study was explained in their own vernacular language and informed consent was obtained from the patient and their relative in their own language as per hospitals rules and regulations. All the patients were kept nil by mouth for atleast 6 hours. Baseline values of pulse, respiratory rate, SpO2 with pulse oximetry finger probe and blood pressure were recorded upon arrival of the patient to the preoperative room. After that the 18-gauge or 20-gauge venous cannula was inserted into the dorsum of the hand or forearm under all antiseptic precautions. All the patients were premedicated with Inj. Promethazine 0.5 mg/kg, Inj Pentazocine 0.5 mg/kg, Inj. Glycopyrrolate 4 μg/kg deep intra muscular 30 min before induction. Inj. Ondansetron 0.1 mg/kg i.v, Inj. Midazolam 20 μg/kg i.v, was given 10 min before induction. After premedication vital data like temperature by palpation, pulse in radial artery, non-invasive blood pressure, respiratory rate and SpO2 with pulse oximetry finger probe were recorded.
All the patients were transferred to operation theatre for operation and monitors like pulse oxymeter, ECG and non-invasive blood pressure cuff were attached to the patient. Intravenous induction of Anaesthesia was accomplished in all patients using Baines circuit and appropriate size face mask. To decrease pressure response during laryngoscopy intravenous inj Xylocard 1.5 mg/kg and inj MgSO4 40 mg/kg was given 3 minutes before induction to all the patients. Induction began with application of face mask and pre-oxygenation using 100% oxygen for 3 minutes. Intravenous induction agents with Inj. Propofol 1.5-2 mg/kg i.v. slow. After centralization of eyeball, Inj. succinylcholine 2.0 mg/kg IV was given. After giving Succinylcholine, intermittent positive pressure ventilation with 100% oxygen was given for 45 to 60 seconds before proceedings for insertion of conventional Macintosh laryngoscope in group M and Truview video laryngoscope in group T respectively. Insertion of Macintosh blade was done with extension of head from left side of angle of mouth and after insertion, blade of Macintosh was kept in midline of oral cavity and displacing the tongue to see the epiglottis and glottis so that alignment of axis of oral pharyngeal and larynx came into one line that facilitated the negotiation of endotracheal tube.
Insertion of Truview blade was done with neutral position of head without extension and after insertion, the oxygen from the oxygen jet port was started at 10 litre/min, blade of Truview was kept in midline of oral cavity and head of the patient was fixed to see the view of epiglottis and vocal cord in the monitor of Truview PCD screen as shown in Figure 1. At the time of negotiation of endotracheal tube, the head of patient which was otherwise more mobile was fixed and Truview blade little elevated. So that alignment of axis of oral pharyngeal and larynx came into one line that facilitated the negotiation of endotracheal tube.
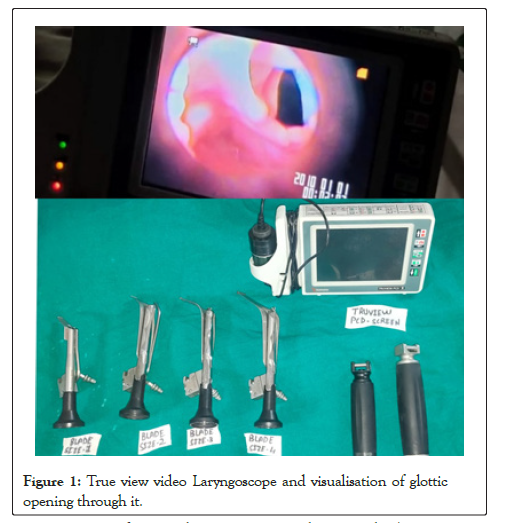
Figure 1: True view video Laryngoscope and visualisation of glottic opening through it.
Maintenance of Anaesthesia was carried out with 50% oxygen, 50% nitrous oxide, IPPV, traces of inhalational agents(sevoflurane, isoflurane) and bolus of Inj. Atracurium 0.5 mg/kg i.v. followed by in doses of 0.1 mg/kg i.v. as and when required. Analgesia was done with Inj. Paracetamol 15 to 20 mg/kg i.v. infusion after induction of Anaesthesia. In our study, primary objectives were time taken for insertion of intubating device (in seconds); Time taken for insertion of endotracheal tube (in seconds); Total Time taken for endotracheal intubation (in seconds) and Compare hemodynamic stability. Secondary objectives were Numbers of attempts for intubation; any alternative intubation technique or any assistance is required or not; External laryngeal pressure required or not; Use of sty let required or not. All the patients were monitored continuously throughout the procedure and surgery. Temperature, Pulse, non-invasive blood pressure, respiratory rate, SPO2 and ECG were recorded at 0 min, 30 sec, 1min, 3min, 5 min, 10 min, 15 min, 20 min, 30min, 60 min and 90 min interval.
After completion of surgical procedure, residual neuromuscular block was antagonized by inj. Neostigmine 50 ug/kg and inj. Glycopyrrolate 8 ug/kg. After adequate reversal of neuromuscular blockade which is observed by limb movements and head rise of patient and fulfilling the standard criteria of extubation, endotracheal tube was removed. After removal of endotracheal tube, patient was observed and was shifted to post Anaesthesia care unit with pulse oximetry monitoring. Relatives were allowed to sit at the bedside immediately on admission to post Anaesthesia care unit. Postoperatively patients were observed for complications like mucosal trauma, bleeding, hoarseness of voice, arrhythmia, bradycardia, tachycardia, desaturation, hypoxia, bronchospasm, laryngospasm involuntary movement, secretions, hypotension and hypertension. Statistical analysis was done by using SPSS Statistical Software version 24.0. Mean and standard deviation were calculated. Unpaired ‘t’ test were applied between Group M and Group T. p value of<0.05 was considered statistically Significant and p value<0.001 was considered statistically highly significant.
Table 1 shows, in group M mean age was 34.53 years with SD 11.85, in group T mean age was 35.06 year and SD 12.22 which was statistically insignificant. In group M mean weight was 58.66 kgs with SD 10.82 in group T mean weight was 59 kgs and SD 5.93 which was statistically insignificant. In group M12 were male and 18 were female, in Group T 14 were male and 16 were female.
| Demographic data | Group M | Group T | p value |
|---|---|---|---|
| Age (in years) | 34.53 ± 11.85 | 35.066 ± 12.22 | 0.86 (NS) |
| Weight (in kg) | 58.66 ± 10.82 | 59 ± 5.93 | 0.88 (NS) |
| Gender (male: female) | 12:18 | 14:16 |
Note: p-value<0.05 is considered significant; p value>0.05 is considered non-significant; NS: Not Significant; SD: Standard Deviation.
Table 1: Demographic data (age, sex and weight) of patients in both groups: Mean ± SD.
Table 2 shows duration of insertion of intubating devices was 7.93 seconds with Standard deviation 2.18 seconds in Group M and 19.2 seconds with Standard deviation 2.85 seconds in group T. Duration of insertion of device between two groups was comparable and shows statistically significant difference between the two groups. Duration of insertion of endotracheal tube was 6.73 seconds with Standard deviation 2.40 seconds in Group M, and 18.96 seconds with Standard deviation 3.29 seconds in group T. Duration of insertion of endotracheal tube between two groups, was comparable and shows statistically significant difference between the two groups. Total duration of endotracheal intubation was 14.66 seconds with Standard deviation 4.02 seconds in Group M and 38.16 seconds with Standard deviation 4.47 seconds in group T. Total duration of endotracheal intubation between two groups, was comparable and shows statistically significant difference between the two groups. Group M was better than group T.
| Time for insertion of intubating device | Time for insertion of endotracheal tube | Total time | p value | |
|---|---|---|---|---|
| Mean+SD (in sec) | Mean+SD (in sec) | Mean+SD (in sec) | ||
| Group M | 7.93 ± 2.18 | 6.73 ± 2.40 | 14.66 ± 4.02 | <0.001 HS |
| Group T | 19.2 ± 2.85 | 18.96 ± 3.29 | 38.16 ± 4.47 | <0.001 HS |
Note: p value<0.05 is considered significant; p value<0.001 is considered highly significant; HS: Highly Significant; SD: Standard Deviation.
Table 2: Comparison of time taken for endotracheal intubation between two groups.
Table 3 shows the means of pulse rate were statistically insignificant in group M and group T before intubation, at 20mins, 25 min, 30 min, 60 min with p value>0.05. The means of pulse rate were statistically significant in group M and group T after intubation at, 30 seconds, 1 min, 3 min, 5 min, 10 mins,15 mins with P value<0.05.
| Time | Group M | Group T | p Value | Remarks |
|---|---|---|---|---|
| (Mean± SD) | (Mean± SD) | |||
| (per minute) | (per minute) | |||
| Before intubation | 89.03 ± 12.21 | 84.4 ± 8.66 | 0.095 | NS |
| After intubation | 93.66 ± 13.31 | 87.53 ± 8.73 | 0.039 | S |
| 30 sec | 96.46 ± 12.21 | 90.6 ± 8.86 | 0.037 | S |
| 1 min | 96.93 ± 11.17 | 90.8 ± 8.87 | 0.021 | S |
| 3 min | 95.26 ± 9.81 | 88.73 ± 8.04 | 0.006 | S |
| 5 min | 92.4 ± 9.16 | 86.73 ± 7.63 | 0.011 | S |
| 10 min | 90.26 ± 9.33 | 84.8 ± 7.71 | 0.01 | S |
| 15 min | 88.93 ± 8.87 | 83.86 ± 7.23 | 0.01 | S |
| 20 min | 88 ± 8.63 | 84.13 ± 7.02 | 0.06 | NS |
| 25 min | 88.53 ± 8.51 | 84.33 ± 8.17 | 0.056 | NS |
| 30 min | 87.86 ± 8.18 | 85.06 ± 7.62 | 0.17 | NS |
| 60 min | 87.5 ± 8.1 | 84.36 ± 6.89 | 0.14 | NS |
Note: p value >0.05 is considered Non-Significant; p value <0.05 is considered significant; NS=Not Significant; S=Significant; SD=Standard Deviation.
Table 3: Comparison of mean pulse rate at different time interval between both groups.
Table 4 shows The means of Mean Arterial Pressure were statistically insignificant in group M and group T before intubation, at 15 mins, 20 mins, 25 min, 30 min, 60 min with p value>0.05. The means of Mean Arterial Pressure were statistically significant in group M and Group T after intubation at, 30 seconds, 1 minute, 3 minutes, 5 minutes, 10 minutes with p value<0.05. So, Table 3 and 4 shows hemodynamic parameters were better with Truview Video laryngoscope as compared with Macintosh laryngoscope.
| Time | Group M | Group T | p value | Remarks |
|---|---|---|---|---|
| (Mean ± SD) | (Mean ± SD) | |||
| (mmHg) | (mmHg) | |||
| Before intubation | 92.77 ± 6.34 | 89.8 ± 8.38 | 0.12 | NS |
| After intubation | 96.86 ± 7.25 | 92.08 ± 8.17 | 0.019 | S |
| 30 sec | 98.68 ± 6.82 | 94.6 ± 8.06 | 0.038 | S |
| 1 min | 97.15 ± 7.61 | 93.02 ± 7.81 | 0.042 | S |
| 3 min | 94.93 ± 6.98 | 90.88 ± 7.62 | 0.036 | S |
| 5 min | 92.64 ± 6.96 | 88.87 ± 6.82 | 0.038 | S |
| 10 min | 91.28 ± 6.92 | 87.88 ± 4.91 | 0.032 | S |
| 15 min | 90.77 ± 6.76 | 89.15 ± 4.89 | 0.29 | NS |
| 20 min | 91.22 ± 7.38 | 90.22 ± 6.28 | 0.57 | NS |
| 25 min | 89.51 ± 5.82 | 90 ± 5.09 | 0.73 | NS |
| 30 min | 92.11 ± 4.85 | 90.98 ± 5.00 | 0.31 | NS |
| 60 min | 92.50 ± 4.06 | 90.72 ± 3.97 | 0.12 | NS |
Note: p value >0.05 is considered Non-Significant; p value <0.05 is considered significant; NS=Not Significant; S=Significant, SD=Standard Deviation.
Table 4: Comparison of mean arterial pressure at different time interval in both groups.
Tracheal intubation by using video laryngoscope is the most innovative advancement and a completely different experience as compared with conventional Macintosh laryngoscope, and skills needed for indirect laryngoscopy using video laryngoscope are very different from those needed for direct laryngoscopy by conventional Macintosh or Miller laryngoscopes [5]. In our study, it took a significantly longer time to intubate with Truview when compared to Macintosh laryngoscope (p<0.001). The mean time to intubation in Group M was 14.66 ± 4.02 seconds, but in Group T, it was 38.16 ± 4.47 seconds. In 2007 Barak et al. conduct a study to compare Truview video laryngoscope and Macintosh laryngoscope in adult patients, and found that The time to intubation was more with Truview video laryngoscope (33 ± 12 s) as compared to Macintosh laryngoscope (24 ± 13 s) and the Truview video laryngoscope provides a better Cormack lehane view than the Macintosh laryngoscope. Similar Results are found in our study [6]. Timanaykar, et al. conduct a study to compare Truview blade with Macintosh blade for laryngoscopy and intubation, and found that the Truview video laryngoscope take more time to intubate the patient as compared to Macintosh laryngoscope. Similar Results are found in our study [7]. Samal, et al. conduct A Comparative Study between Truview PCD Video Laryngoscope and Macintosh Laryngoscope for Quality of Intubation and Hemodynamic Changes, and found that The Truview video laryngoscope provide better view of glottis, but take more time to intubate the patient as compare with the Macintosh laryngoscope. Similar Results are found in our study [4].
In our study, Mean Arterial Pressure was comparable in both groups with there was statistically significant difference between two groups at 0, 30 seconds, 1, 2, 3, 5, 10, minutes (p value<0.05). While statistically insignificant difference between two groups at before intubation 15, 20, 25, 30, 60 minutes (p value>0.05), mean pulse rate was comparable in both groups with there was statistically significant difference between two groups at 0, 30 seconds, 1, 2, 3, 5, 10, 15 minutes (p value<0.05), while statistically insignificant difference between two groups at 20, 25, 30, 60 minutes (p value>0.05).
Bag, et al. conduct study to compare Truview PCD laryngoscope and Macintosh laryngoscope in viewing glottic opening and ease of intubation, and found that the haemodynamic stability was significantly better with the use of Truview PCD laryngoscope when compared to Macintosh laryngoscope. Similar Results are found in our study [8].
Dambale, et al. conduct a Comparative study of Truview Evo- 2 laryngoscope and Macintosh laryngoscope for hemodynamic stability, and found that there was better hemodynamic stability with use of Truview video laryngoscope as lifting force required was less with Truview video laryngoscope when compared to Macintosh laryngoscope. Similar Results are found in our study [9].
Bhatia and Shah conducted a study to compare Truview Video laryngoscope and Macintosh laryngoscope for difficult intubation, and found that Tracheal intubation in patients with anticipated difficult airway using Truview blade provided significantly better laryngeal view as compared to Macintosh blade without the need to alignment of oropharyngeal and laryngeal axes, with less attempts and almost no change in hemodynamic parameters, but the time taken for intubation was more with Truview video laryngoscope. In our study Intubation is easier with Truview Video laryngoscope and time taken for intubation was more with Truview video laryngoscope. But hemodynamic parameters are better with Truview video laryngoscope as compared with Macintosh laryngoscope [10,11].
The anesthetist performing the intubation was not blinded due to the unfeasibility of blinding and the possibility of bias existed and The experience of the anesthetist was significantly less with the Truview laryngoscope as compared with Macintosh laryngoscope are limitations of this study.
From this study it was concluded that Truview Video laryngoscope provides easier intubation as compared with Macintosh laryngoscope. Truview video laryngoscope also provide better hemodynamic as compared with Macintosh Laryngoscope. But total duration of intubation is more with Truview Video laryngoscope than with Macintosh laryngoscope. Truview video laryngoscope, newer airway device, is more user friendly, simple, easy to use as compared to conventional Macintosh laryngoscope. Patients with predicted difficult airway, it should be kept ready to use in difficult airway cart and these video laryngoscope devices are also included in difficult airway algorithm 2013.
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar].
Citation: Kalathiya P, Trivedi V (2022) Comparison of Ease of Intubation and Haemodynamic Stability of Macintosh Laryngoscope versus Truview Video Laryngoscope. J Anesth Clin. Res. 13:1054.
Received: 13-Apr-2022, Manuscript No. JACR-22-16771; Editor assigned: 15-Apr-2022, Pre QC No. JACR-22-16771 (PQ); Reviewed: 26-Apr-2022, QC No. JACR-22-16771; Revised: 02-May-2022, Manuscript No. JACR-22-16771 (R); Published: 09-May-2022 , DOI: 10.35248/2155-6148.22.13.1054
Copyright: © 2022 Kalathiya P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.