International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2024)Volume 12, Issue 1
Introduction: Myelomeningocele is one of the most common types of closed neural tube defect. Repair of this malformation should be conducted as early as possible to avoid contamination with the external environment. In 2011, an American randomized clinical trial was carried out showing there are neurological benefits in performing intrauterine surgery compared to postnatal surgery, with fewer cases of cerebrospinal fluid shunt and hindbrain herniation. In Brazil, this technique is not yet widespread and many services perform repair after birth.
Objective: To describe the epidemiological profile of individuals with myelomeningocele seen in an initial consultation, in a rehabilitation network in Brazil, between 2021 and 2023, with an emphasis on reducing cerebral herniation and fewer cases of hydrocephalus with ventriculoperitoneal shunt.
Method: This is a retrospective longitudinal study of individuals with neural tube closure defects seen in an initial consultation, based on electronic medical records at the Associação de Assistência à Criança Deficiente (AACD), between January 2021 and May 2023.
Results: A total of 262 patients diagnosed with spina bifida were evaluated, 237 patients with myelomeningocele. Of these, 59 (24.89%) were submitted to intrauterine repair, and 178 (75.11%) to postnatal repair. Hydrocephalus was more frequently observed in patients undergoing postpartum correction (92.3%) than intrauterine repair (78.2%) (p=0.004). In addition, ventriculoperitoneal shunt implantation was more frequent in patients undergoing postpartum repair (86.2%) than intrauterine procedure (13.8%) (p<0.001). It was not possible to identify a statistical difference as to hindbrain herniation, since only 14.3% of patients had the condition investigated. However, prematurity was more frequent in patients submitted to intrauterine repair (79.6%), whereas 66.3% of patients undergoing postnatal repair were not premature (p<0.001).
Conclusion: Patients undergoing intrauterine myelomeningocele repair had better neurological outcomes than those submitted to postnatal surgery, even with a higher frequency of prematurity.
Myelomeningocele (MMC) is one of the most common types of closed Neural Tube Defects (NTD). It is characterized by extrusion of the spinal cord into a sac filled with cerebrospinal fluid, due to a failure in the fusion of the posterior arches of the spine. This congenital malformation causes failure of the spinal canal to close over the spinal cord and spinal cord dysplasia, generating varied degrees of motor deficit, urinary and fecal incontinence, in addition to changes in the central nervous system [1].
Among these neurological changes, hydrocephalus with Ventriculoperitoneal Shunt (VPS) and Arnold Chiari II syndrome, which is characterized by brain herniation, are the most relevant, the latter being one of the main causes of death in these patients in the first 5 years of life [2]. Repair of this condition usually occurs soon after birth to avoid contact with the external environment and infection [3]. In Brazil, the prevalence of MMC is approximately 14 cases per 10,000 live births, differing from the North American estimate of 2.02 to 2.62 cases per 10,000 live births [4,5].
In 2011, a randomized clinical trial was carried out comparing safety and efficacy of correcting this malformation by intrauterine surgery versus postnatal surgery. It was entitled Management of Myelomeningocele Study (MOMS) and showed the benefits of intrauterine closure surgery, with a significant reduction in the need for intrauterine ventriculoperitoneal shunting when compared to postnatal repair. In addition to reducing the presence of Arnold Chiari II syndrome, it improved neurological outcomes [1].
However, when performing these fetal surgeries, there is greater risk of maternal and gestational complications, such as increased risk of premature rupture of membranes, premature birth, and surgical wound dehiscence. Therefore, in Brazil, fetal medicine teams are using various intrauterine surgical techniques to improve the neurological prognoses of patients with MMC and reduce the risks of maternal and fetal complications. To perform these surgeries, there are some eligibility criteria, including single fetus pregnancy, gestational age, maternal clinical conditions, no history of other chromosomal abnormalities, etc. [6,7].
This article describes a retrospective study aimed to characterize the epidemiological profile of individuals with neural tube closure defects, treated in a Brazilian rehabilitation organization, and to find outcomes that are in line with the literature, with an emphasis on reducing the incidence of Arnold Chiari II syndrome and the need for VPS. The epidemiological description of this group will provide relevant and updated data for comparison with current national and international research data, and for scientific research, as a functional follow-up of these individuals.
This is a retrospective longitudinal study of individuals with closed Neural Tube Defects (NTD) seen in an initial consultation at the Associação de Assistência à Criança Deficiente (AACD), with information obtained from electronic medical records. The data collected included patients’ personal data, neurological level of involvement at initial assessment, associated comorbidities, past surgical history, need for placement of a ventriculoperitoneal shunt, and presence of Arnold Chiari II malformation. Data was collected through an active search of all medical records of patients who underwent initial consultations from the Health Department regulatory system, the medical insurance system authorized by the AACD and privately, between January 2021 and May 2023. This initial assessment was performed by physicians. Patients diagnosed with myelomeningocele were selected.
Medical records with no initial consultation or with any other diagnosis (neurological or orthopedic) associated with NTD were excluded from the study. Medical records with incomplete information were treated as missing data. All tests conducted considered a two-way α (p value) of 0.05 and a 95% Confidence Interval (CI) and were carried out with computational support from R1 or IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, N.Y, USA) software. Data were described with frequency and confidence interval for qualitative variables and with measures of central tendency (mean and median) and measures of dispersion (standard deviation, interquartile range, minimum and maximum) for quantitative data. The existence of an association among qualitative variables was tested with the chisquared test, and Yates correction was applied when the expected frequency in one of the classes was less than 5. The association between quantitative and qualitative variables was assessed using the Wilcoxon test. The sensitivity of the chi-squared test for the main outcome (occurrence of Arnold Chiari II malformation and need for VPS) was calculated with the G* Power software.
During the study period, a total of 262 patients with neural tube closure defects were investigated. Of these, 21 patients had different diagnoses of myelomeningocele (nine lipomeningocele, three sacral agenesis, three spina bifida occulta, two meningocele, two syringohydromyelia, one encephalocele, and one syringomyelia). Furthermore, three patients were excluded from the study because they had no initial consultation in the electronic medical record, and one patient had a diagnosis associated with Edwards syndrome. The final sample had 237 patients with myelomeningocele; in that, 59 (24.89%) underwent intrauterine repair, and 178 (75.11%) postnatal surgery.
In this sample, 119 patients were female (50.2%), mean age of 49 months at the initial consultation, ranging between 2 and 214 months. Most patients were treated in city of São Paulo-SP with 122 (51.4%) consultations, followed by the cities of Recife-PE, with 74 (31.2%) consultations, Porto Alegre-RS with 12 (5.1%) consultations, Osasco-SP, and Mogi das Cruzes-SP with 11 (4.6%) consultations each, and, finally, Uberlândia-MG with 7 (3%) consultations.
The neurological level of involvement was assessed at the initial consultation, based on the analysis of the physical examination, and it was divided into three categories: thoracic, lumbar, and sacral. In the group undergoing intrauterine repair, 51 patients (86.4%) had a lumbar involvement, seven (11.9%) sacral, and one case (1.7%) had thoracic involvement. In the postnatal group, 118 patients (66.3%) had a lumbar involvement, 35 patients (19.7%) thoracic, and 25 cases (14%) had sacral involvement.
Among the most prevalent comorbidities, 35.8% of patients with myelomeningocele had Congenital Clubfoot (CCF). Only 1.5% of patients have no co-morbid conditions. Below, the consolidated table of all population characteristics according to the type of procedure (Table 1).
| Intrauterine repair | |||||
|---|---|---|---|---|---|
| No | Yes | ||||
| Variables/Categories | N | % (CI95) | N | % (CI95) | p value |
| Sex | |||||
| Female | 93 | 52.25 (44.92-59.5) | 26 | 44.07 (31.94-56.77) | |
| Male | 85 | 47.75 (40.5-55.08) | 33 | 55.93 (43.23-68.06) | 0.28 |
| AACD | |||||
| Mogi das Cruzes | 7 | 3.93 (1.78-7.57) | 4 | 6.78 (2.33-15.32) | |
| Osasco | 4 | 2.25 (0.76-5.25) | 7 | 11.86 (5.47-21.89) | |
| Porto Alegre | 9 | 5.06 (2.53-9.02) | 3 | 5.08 (1.45-12.95) | <0.001 |
| Recife | 66 | 37.08 (30.24-44.34) | 8 | 13.56 (6.63-23.96) | |
| São Paulo | 90 | 50.56 (43.26-57.85) | 32 | 54.24 (41.58-66.49) | |
| Uberlândia | 2 | 1.12 (0.23-3.56) | 5 | 8.47 (3.31-17.58) | |
| Neurological level of involvement | |||||
| Thoracic | 35 | 19.66 (14.34-25.96) | 1 | 1.69 (0.18-7.65) | |
| Lumbar | 118 | 66.29 (59.13-72.93) | 51 | 86.44 (76.04-93.37) | 0.033 |
| Sacral | 25 | 14.04 (9.53-19.71) | 7 | 11.86 (5.47-21.89) | |
| Hydrocephalus | |||||
| No | 13 | 7.74 (4.41-12.51) | 12 | 21.82 (12.52-34) | 0.004 |
| Yes | 155 | 92.26 (87.49-95.59) | 43 | 78.18 (66-87.48) | |
| Mode of delivery | |||||
| Vaginal | 20 | 14.93 (9.67-21.68) | 1 | 1.89 (0.2-8.48) | 0.011 |
| Cesarean section | 114 | 85.07 (78.32-90.33) | 52 | 98.11 (91.52-99.8) | |
| Any comorbidity? | |||||
| No | 3 | 2.05 (0.58-5.38) | 0 | 0 (0-0) | 0.723 |
| Yes | 143 | 97.95 (94.62-99.42) | 50 | 100 (100-100) | |
| CCF? | |||||
| No | 98 | 67.12 (59.23-74.35) | 28 | 56 (42.23-69.1) | 0.157 |
| Yes | 48 | 32.88 (25.65-40.77) | 22 | 44 (30.9-57.77) | |
| Premature? | |||||
| No | 57 | 66.28 (55.88-75.6) | 10 | 20.41 (11-33.19) | <0.001 |
| Yes | 29 | 33.72 (24.4-44.12) | 39 | 79.59 (66.81-89) | |
| Cranial magnetic resonance imaging MRI? | |||||
| No | 169 | 95.48 (91.65-97.84) | 43 | 74.14 (61.89-84.04) | <0.001 |
| Yes | 8 | 4.52 (2.16-8.35) | 15 | 25.86 (15.96-38.11) | |
| Arnold Chiari II? | |||||
| No | 3 | 16.67 (4.93-38.14) | 5 | 31.25 (13.06-55.57) | 0.317 |
| Yes | 15 | 83.33 (61.86-95.07) | 11 | 68.75 (44.43-86.94) | |
| PVD? | |||||
| No | 37 | 22.84 (16.89-29.75) | 26 | 56.52 (42.16-70.09) | <0.001 |
| Yes | 125 | 77.16 (70.25-83.11) | 20 | 43.48 (29.91-57.84) | |
Table 1: Descriptive statistics of patient characteristics according to the type of neural tube closure, with Number of patients per category (N) and percentage with 95% Confidence Interval (CI) and chi-square test for association.
Malformation repair
Regarding gestational data, in the group undergoing intrauterine repair, all patients were born by cesarean delivery. The minimum and maximum ages for correction were 20 and 30 weeks, respectively. The mean gestational age for surgery of this malformation was 24 weeks, with 75% of patients undergoing repair at a gestational age of 26 or less weeks.
In the postnatal group, a total of 114 patients (64.4%) were born by cesarean section, 20 patients (11.3%) by vaginal delivery, and the remaining 43 patients (24.3%) did not have this information recorded in the initial consultation. The mean age for correction was 3 days of age, varying between 1 and 34 days.
Prematurity
Prematurity means the birth occurred at gestational age of less than completed 37 weeks [8]. Among premature patients, the gestational age at birth was significantly lower for patients with intrauterine surgery, with a median of 34 weeks, varying between 24 and 36 weeks. Premature patients with postnatal correction had a median gestational age of 36 weeks. The evaluated data are presented in (Table 2) (Figure 1).
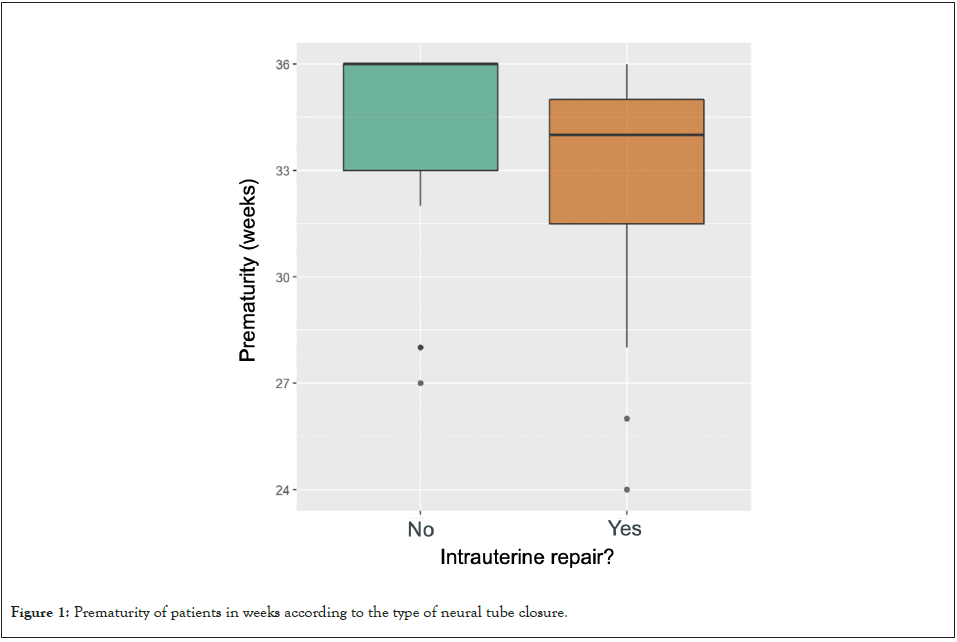
Figure 1: Prematurity of patients in weeks according to the type of neural tube closure.
| Prematurity weeks (<37 weeks) | ||||||
|---|---|---|---|---|---|---|
| Intrauterine repair? | Valid N | Absent | Mean (± SD) | Median (IQR) | Min-Max | p value |
| No | 29 | 0 | 34.41 (± 2.72) | 36 (33-36) | 27-36 | 0.002 |
| Yes | 39 | 0 | 33.05 (± 2.92) | 34 (31-35) | 24-36 | |
Table 2: Descriptive statistics of prematurity of patients according to type of neural tube closure with Number of patients (N); mean and Standard Deviation (SD); median and Interquartile Range (IQR); and minimum and maximum values of the variable with the Wilcoxon (Mann-Whitney) test for association.
The frequency of premature birth was significantly associated with type of surgery, and was higher in patients undergoing intrauterine repair (79.6%), versus postnatal correction (66.3%) (p<0.001), as shown in Table 1.
Hydrocephalus with ventriculoperitoneal shunt
Hydrocephalus was present in 43 patients (74.1%) undergoing intrauterine surgery. In 12 (20.7%) patients submitted to prenatal repair, none presented hydrocephalus, whereas 3 (5.2%) cases did not have this information in their medical records. In the group submitted to postnatal surgery, 155 patients (87.1%) presented with hydrocephalus, whereas 13 (7.3%) did not. The remaining 10 patients (5.6%) had no information available in the record. Therefore, hydrocephalus was associated with type of surgical repair, since it was significantly more frequent in the postpartum repair group (92.3%; p=0.004) than in the intrauterine surgery (78.2%), as shown in Table 1.
In patients undergoing intrauterine surgery and presenting with hydrocephalus, only 20 cases (46.5%) required a ventriculoperitoneal shunt. The remaining 22 cases (51.2%) had no indication for VPS, and only one (2.3%) had no information available in the medical record. Among patients with hydrocephalus undergoing postnatal surgery, 125 (80.6%) required VPS. Twenty-eight patients (18.1%) did not require VPS, and two cases (1.3%) had no information recorded in the medical records. Therefore, the need for VPS is more frequent in patients who had postpartum neural tube closure repair (86.2%), as compared to those undergoing an intrauterine procedure (13.8%) (p<0.001), as shown in (Table 3).
| Intrauterine repair | |||||
|---|---|---|---|---|---|
| No | Yes | ||||
| Variables/Categories | N | % (CI95) | N | % (CI95) | p value |
| VPS | |||||
| No | 35 | 58.73 (46.41-70.27) | 26 | 41.27 (29.73-53.59) | <0.001 |
| Yes | 93 | 86.21 (79.9-91.09) | 20 | 13.79 (8.91-20.1) | |
Table 3: Descriptive statistics of VPS development according to the type of neural tube closure, Number of patients per category (N), percentage with 95% Confidence Interval (CI), and chi-squared test for association.
Furthermore, patients submitted to intrauterine correction had VPS implanted later, on average 208 days after birth, whereas in patients undergoing postnatal surgery, the VPS was implanted, on average at 55 days, with statistical significance (p=0.001), as shown in (Figure 2).
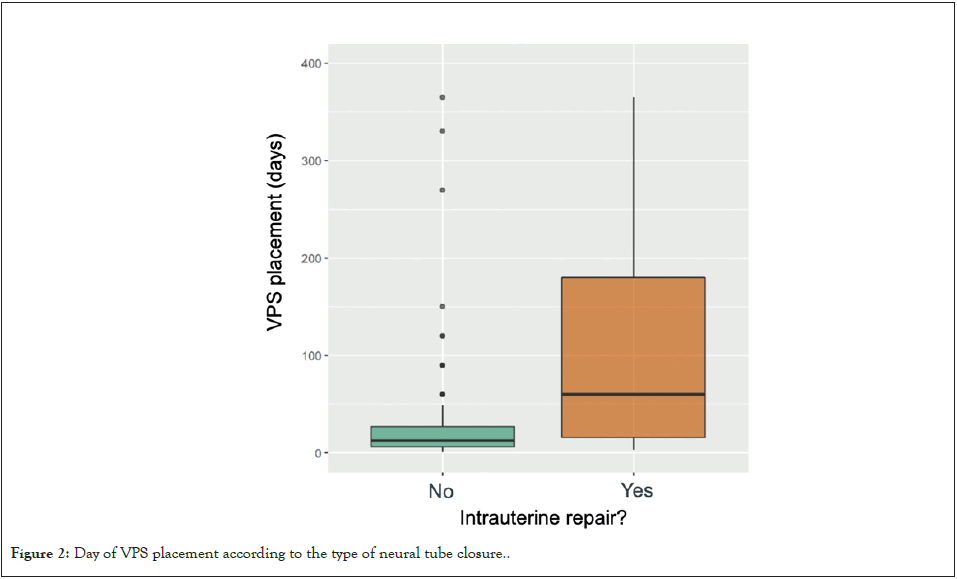
Figure 2: Day of VPS placement according to the type of neural tube closure..
In this context, it was possible to identify the statistical difference between the surgical groups and the need for VPS implantation. The study sample (208 patients for this variable) was sufficient to find a small effect (0.194), but the observed effect exceeded this value; therefore there was a statistical difference. Considering the non-implantation of VPS as successful treatment, intrauterine surgery had a success likelihood of 56.5%, whereas postnatal repair had 22.8%, with an absolute risk reduction in intrauterine surgeries by 33.7% (95% CI: 17.8%-48.2%).
Arnold Chiari II syndrome
Analysing the presence of Arnold Chiari II syndrome, 43 patients (72.9%) undergoing intrauterine surgery had no information about it. The diagnosis was made in 11 patients (18.6%) and five (8.5%) did not present the syndrome. In this context, it is worth mentioning that 44 patients (74.6%) had no brain Magnetic Resonance Imaging (MRI) performed, although it is one of the diagnostic methods for this malformation. Only 15 patients (25.4%) in the intrauterine group had this MRI at the initial consultation. In the postnatal group, 159 patients (89.9%) had no report of Arnold Chiari II. In view of the above, it was not possible to find a statistical association between the occurrence of Arnold Chiari II syndrome and the surgical groups, since only 14.3% of patients had the condition investigated, which reduces the sensitivity of the sample to detect an association.
This was the first Brazilian study to show the different outcomes comparing intrauterine and postnatal repair for myelomeningocele. The results presented are in line with what was presented in the MOMS. In 2011, Adzik, et al., carried out a randomized clinical trial, comparing the outcomes between pre and postnatal surgeries for myelomeningocele [1]. It was possible to identify reduced need for ventriculoperitoneal shunt of 82% in postnatal approach and 40% intrauterine surgery, and a reduction in Arnold Chiari II syndrome of 96% and 64% in postnatal and intrauterine repairs, respectively. Despite a greater number of gestational complications in the intrauterine group, such as oligohydramnios and placental detachment, there were no maternal deaths. In addition, although approximately 13% of patients were preterm with less than 30 weeks of gestation, the prenatal group showed better neurological outcomes than the postnatal group. These results were so relevant that the study was interrupted before the deadline due to proof of efficacy of intrauterine surgery benefits; in that, out of the initial 200 pregnant women, only 183 participated in the randomization [1].
In the Brazilian context, this study was extremely important since, for legal reasons, it is not possible to interrupt pregnancy based on prenatal diagnosis of the condition herein addressed. Therefore, the use of an approach that improved fetal prognosis was necessary. However, the use of the surgical technique presented in the MOMS cannot be replicated in Brazil, for it is not permitted to use the same surgical stapler mentioned, due to lack of legal administrative authorization [9]. Faced with this situation, Brazilian fetal teams have developed different surgical approaches to maintain the neurological benefits present in the base study, with minimal maternal-fetal complications.
Pedreira, et al., carried out a study with 10 Brazilian cases with endoscopic intrauterine closure [6]. The mean gestational age was 32 weeks, and there were no intraoperative fetal deaths. However, in two cases it was not possible to complete the surgery due to complications, and one patient, born at 29 weeks, died in the neonatal period due to necrotizing enterocolitis that progressed to sepsis. Despite these complications, six out of seven patients had their Arnold Chiari II malformation totally reversed, documented by Magnetic Resonance Imaging (MRI) performed before and after the procedure. In addition, only three patients required postnatal VPS, showing improvement in neurological outcomes. Given the above, even with a small number of patients, the endoscopic approach can be an alternative to reduce maternal-fetal risks and improve the neurological condition [6].
Furthermore, in Brazil, Botelho, et al., conducted a study of 39 cases submitted to intrauterine repair by mini hysterectomy [7]. Only three cases required postnatal VPS, corroborating the main hypothesis. In this study, despite a mean gestational age of 35 weeks, there were no cases of neonatal, fetal, or maternal death, nor of maternal or fetal complications until the patients were discharged. The only difference is that the incidence for VPS placement was slightly higher than in MOMS, with approximately 7.7% compared to 2.4%, which may have occurred due to the different groups of neurosurgeons who indicated the VPS using different criteria. The incidence of total or partial improvement in Arnold Chiari II syndrome identified by MRI was similar to the base study. This shows that, besides improving neurological outcomes in patients with MMC, this approach is an option that may pose fewer maternal and fetal risks, even with a history of prematurity [7].
Another Brazilian fetal medicine team led by Monron, et al., coordinated a retrospective cohort study analyzing the impact of open fetal surgery on neurological outcomes [9]. Over a period of 6 years, 319 pregnant women were screened and 237 pregnant women underwent this type of surgery, with few variations from the technique used in the MOMS. They did not observe any maternal deaths or severe maternal complications during the study. The perinatal loss rate was 2.1%, due to placental abruption, umbilical cord constriction, and premature rupture of membranes with severe oligohydramnios. Only one surgery could not be completed, which evolved into an emergency cesarean section with postnatal MMC repair. In this group, 27% had premature rupture of membranes and 24% had premature birth. The reversal of herniation of the posterior elements of the brain was 71.1% according to pre and postnatal evaluation with neonatal ultrasound and/or brain MRI, with results similar to the MOMS [9].
In the current study, VPS implantation was reduced by 86.2% in the postnatal group and 13.8% in the intrauterine group. Even not identifying the surgical technique employed in these patients, nor the presence of maternal and fetal complications inherent to the procedure, there was a relevant statistical difference, showing again that prenatal repair, regardless of the approach, brings neurological benefits. However, it was not possible to investigate Arnold Chiari II syndrome. One of the hypotheses to explain this obstacle is the difficult access to MRI, especially in the public health system. Hence, it was not feasible to determine whether there was a statistical difference, given the small fraction of the total sample.
In Brazil, it is still not possible to fully carry out this procedure because this type of surgery is not available within the scope of the Unified Health System (SUS), the Brazilian public health system, nor is it included in the Procedure List of the Agência Nacional de Saúde Suplementar (ANS), the Brazilian regulatory body for private health care plans [10,11]. Therefore, this not only creates a legal obstacle to carrying out such an approach, but also hinders the availability of access to treatment. Currently, a bill was proposed to conduct this surgery through the public health system, but it is still in the deliberation process.
The intrauterine myelomeningocele repair approach reduced VPS placement cases, with results similar to those observed in the MOMS. It was not possible to investigate Arnold Chiari II Syndrome, due to limited access to the diagnostic test. In Brazil, there is a lack of results showing long term motor and functional outcomes in these patients, to better monitor functionality and confirm the benefits of intrauterine surgery compared to postnatal surgery.
Citation: Binha AMP, Kuwae LM, Barros IHYD (2024) Comparison between Intrauterine and Postnatal Myelomeningocele Repair Surgery: A Retrospective Longitudinal Study in Brazil. Int J Phys Med Rehabil. 12:717.
Received: 21-Jan-2024, Manuscript No. JPMR-24-29266; Editor assigned: 23-Jan-2024, Pre QC No. JPMR-24-29266 (PQ); Reviewed: 08-Feb-2024, QC No. JPMR-24-29266; Revised: 16-Feb-2024, Manuscript No. JPMR-24-29266(R); Published: 26-Feb-2024 , DOI: 10.35248/2329-9096.24.12.717
Copyright: © 2024 Binha AMP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited