
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 10
Background and aim: Epidural analgesia using Bupivacaine for abdominal surgeries causes hypotension at the bargain of analgesia. This study was designed to compare effect of 0.0625% bupivacaine with 2% fentanyl and 0.125% bupivacaine with 2% fentanyl epidural infusion on haemodynamic parameters for 48 hrs in infraumbilical surgeries and VAS as the secondary objective with preserved hemodynamic parameters.
Materials and methods: A randomized, prospective, double-blind study was carried out in sixty consenting adult patients of either sex between the ages of 18-65 years undergoing infra umbilical surgery. Group 1 (n=30) patients received continuous epidural infusion of 0.0625% bupivacaine with 2 ug/ml fentanyl and group 2 (n=30) received 0.125% bupivacaine with 2 ug/ml fentanyl. Postoperatively hemodynamic parameters and VAS was recorded at interval of 3 hrs till 48 hrs. The infusion was stopped if there was hypotension even with lowest infusion rate (5 ml/ hr).
Results: In total, 60 patients were randomized (n=30 in each groups). After 9 hrs the infusion was stopped in 5 patients who increased to 6 after 12 hrs, 9 after 15 hrs, 12 after 21 hrs. Statistical difference was noted between two groups from 9 hrs to 48 hrs in SBP and DBP (p<0.05). Significant variation in hemodynamics was noted in whom the infusion was stopped. Significant difference in (Visual Analogue Scale) VAS was noted after 12 hrs, 15 hrs and 18 hrs among the patients in whom the infusion was stopped.
Conclusion: Satisfiable VAS could be achieved in group 1 with preserved haemodynamic parameters. On contrary infusion was stopped in 12 patients in group 2 in view of hypotension which led to increase in VAS due to pain.
Epidural; Bupivacaine; Abdominal surgery
The most common type of acute pain that the anesthesiologists deal with is postoperative pain with resultant neuroendocrine stress response causing protein catabolism, hyperglycemia, poor wound healing, decreased respiratory function, and increase in myocardial oxygen demand [1]. Pain relief can be provided by nonopioid analgesics or systemic opioids, regional neuraxial and peripheral analgesic techniques and route. Epidural being standard technique and safer resulting in shorter Intensive Care Unit stays. Addition of opioids to local anesthetics has several benefits such as improved dynamic pain relief, limited regression of sensory blockade, and decreased dose of local anesthetic. Use of lipophilic opioid (fentanyl) is preferred to hydrophilic as it provides rapid onset of action, rapid clearance, and prevents delayed respiratory depression [2]. Opioid and local anesthetic infusion by an epidural catheter is widely used as a postoperative pain management method after major abdominal surgeries [3]. It was found out by preliminary study that in most of the patients in whom 0.125% bupivacaine with 2% fentanyl infusion was started had to be stopped because of haemodynamic instability [4]. Hence we aimed at comparing the hemodynamic and analgesic effects of epidural 0.0625% bupivacaine with 2% fentanyl and 0.125% bupivacaine with 2% fentanyl postoperatively.
The rate of infusion was increased or decreased as per the hemodynamic parameters and VAS of the patient. Hemodynamic parameters, VAS (0-10), level of sensory block and level of motor block were monitored for 48 hrs postoperatively and need for rescue analgesia, side effects, and interventions if any were noted. Whenever the VAS score was more than 3, the rate of infusion was stepped up in a graded manner by 5 ml/h up to 12 ml/h. If not relieved after 12 ml/h, rescue analgesia was given in the form of injection paracetamol and tramadol 50 mg intravenously. The infusion was stopped if there was hypotension even with lowest infusion rate (5 ml/hr) and bolus of 500 ml crystalloid was given till systolic blood pressure reached more than 90 mm Hg or (Mean Arterial Pressure)MAP reached more than 60 mm Hg and other modalities of analgesia like paracetamol and tramadol were given intermittently. No other form of sedative or analgesia was permitted except rescue analgesia. In case of occurrence of motor block the infusion was stopped temporarily till the Bromage score was 0.
The findings were analyzed statistically using Chi-square test and Student’s t-tests using SPSS version 22 (SPSS, Inc., Chicago, IL). The P<0.05 was considered statistically significant.
This study was designed to compare effect of 0.0625% bupivacaine with 2% fentanyl and 0.125% bupivacaine with 2% fentanyl epidural infusion on haemodynamic parameters for 48 hrs in infraumbilical surgeries. The secondary objective was to compare the VAS score with maintaining stable haemodynamic parameters. The proposed study was conducted at Command Hospital (Air Force) Bengaluru after obtaining permission from the Institutional Ethical Committee. A total of 65 patients with consenting candidates who satisfy necessary inclusion/exclusion criteria during the 18 months period between Dec 2018 to Dec 2019. Patients accepted in ASA I and II in whom surgeries were performed by infra umbilical incision and required epidural infusion were included. Valid Written Informed Written Consent of patient and (Next of Kin) NOK in each case wherever applicable. Following were excluded from study: who were not willing for valid written informed consent and patients of ASA III or more, contraindications for epidural placement like coagulopathy, bleeding disorders. After Institutional Ethics Committee approval, a randomized, prospective, double-blind study was carried out in sixty ASA (American Society of Anesthesiologists) I and II consenting adult patients of either sex between the ages of 18-65 years undergoing infraumbilical surgery. Patients with ASA III and IV, those with infection at the site of epidural injection, coagulopathy or bleeding disorders, severely hypovolemic patients, those with raised intracranial pressure, sepsis, preexisting neurological deficit, demyelinating disorder, or severe spinal deformities were excluded from this study. Sample size of thirty in each group was calculated based on available reference studies, within 95% confidence limit and 80% of power. Hence over and above 60 five participants were included extra. Out of 65, five participants declined to participate in the study. Patients were randomized by computergenerated randomization charts into two study groups, Group 1 (n=30) received 0.0625% bupivacaine with 2 ug/ml fentanyl and Group 2 (n=30) received 0.125% bupivacaine with 2 ug/ml fentanyl postoperatively. Both groups were comparable with respect to their demographic data. Baseline blood pressure, pulse rate, and SpO2 were recorded. Adequate preloading (500 ml) was done with 18-gauge intravenous cannula. Patients received injection glycopyrrolate (0.002 mg/kg) and injection ranitidine (1 mg/kg) intravenously as premedication. Thereafter, an epidural catheter was inserted at the lumbar level (L1-L2 or L2- L3). The space was checked by loss of resistance technique and confirmed by the meniscus sign. Epidural test dose was given with 3 ml 2% adrenalized lignocaine. The absence of tingling numbness in the lower limbs and tachycardia was confirmed after 4-6 cm of catheter was placed in the epidural space. After fixation of catheter, patients were made supine and free injection of saline through the catheter was checked. Patients were premedicated with injection fentanyl 2 ug/kg and injection midazolam 0.02 mg/kg. Patients were preoxygenated with 100% O2 for 3 min. General anesthesia was given with injection propofol 2 mg/kg mixed with injection xylocard 20 mg intravenously. Suitable relaxant was given to facilitate tracheal intubation after confirming ventilation. Anesthesia was maintained with oxygen, air and sevoflurane. Muscle paralysis was maintained with injection vecuronium bromide intravenously. Group 1 patients received continuous epidural infusion of 0.125% bupivacaine with 2 ug/ml fentanyl after induction of general anesthesia at the rate 7 ml/h intraoperatively. The rate of infusion was adjusted as per the hemodynamic parameters of the patient. Group 2 patients received continuous epidural infusion of 0.0625% bupivacaine with 2 ug/ml fentanyl at the rate 7 ml/h intraoperatively. The pulse rate, blood pressure, SpO2, and EtCO2 were monitored intraoperatively. Infusion was stopped at closure which was approximately 30-45 min before reversal. All patients were reversed with 0.01 mg/kg glycopyrrolate and 0.06 mg/kg neostigmine. The infusion again was started after 30 min of extubation once patient reached the ward. The baxter elastomeric infusion pump had 5 ml/hr, 7 ml/hr and 12 ml/hr rates of infusion. The hemodynamic parameters like SpO2, heart rate, systolic blood pressure, diastolic blood pressure, MAP, VAS was recorded at interval of 3 hrs till 48 hrs. Initially the rate was set to 7 ml/hr and adjusted based on hemodynamic parameters and VAS. The infusion was stopped if there was hypotension even with lowest infusion rate (5 ml/hr) and bolus of 500 ml crystalloid was given and other modalities of analgesia like paracetamol and tramadol were given intermittently.
Statistical methods
Hemodynamic parameters at different time periods and VAS were considered as primary and secondary outcome variables. Study group was considered as primary explanatory variable. All Quantitative variables were checked for normal distribution within each category of explanatory variable by using visual inspection of histograms and normality Q-Q plots. Shapiro- wilk test was also conducted to assess normal distribution. Shapiro wilk test p value of >0.05 was considered as normal distribution.
For normally distributed Quantitative parameters the mean values were compared between study groups using Independent sample t-test (2 groups). For non-normally distributed Quantitative parameters, Medians and Interquartile range (IQR) were compared between study groups using Mann-Whitney u test (2 groups). Categorical outcomes were compared between study groups using Chi square test /Fisher's Exact test (If the overall sample size was <20 or if the expected number in any one of the cells is <5, Fisher's exact test was used). P value <0.05 was considered statistically significant. IBM SPSS version 22 was used for statistical analysis.
A total of 60 people included in the final analysis. Among the study population, 30 (50.00%) had 0.0625% bupivacaine with 2 μg fentanyl and remaining 30 (50.00%) participants had 0.125% bupivacaine with 2 μg fentanyl (Table 1). Among study population, 26(43.3%) of them had diagnosis of Carcinoma Ovary and 23(38.3%) had diagnosis of Fibroid Uterus followed by 4(6%) had diagnosis of Carcinoma Endometrium (Table 2). Among Study Population, 26(43.3%) underwent Cytoreduction surgery, 23(38.3%) underwent (Total Abdominal Hysterectomy with Bilateral Salpingoophorectomy) TAH BSO surgery followed by 4(6%) of them underwent TAH BSO Frozen surgery (Table 3). Among study population, 16(26.6%) of them had insertion at Lumbar1-2 and 44 (73.4%) of them had insertion at Lumbar 2-3 (Table 4). There is no statistically significant difference between two groups in parameter Pulse Rate, Respiration rate, Diastolic Blood Pressure (P>0.05) (Table 5). There is no statistical difference between two groups at starting period, 3 hrs, 6 hrs, 9 hrs, 12 hrs, 15 hrs, 18 hrs, 21 hrs, 24 hrs and 48 hrs (p>0.05) of infusion (Table 6). There is no statistical difference between two groups at starting period, 3 hrs, 9 hrs, 12 hrs, 15 hrs, 21 hrs, 24 hrs and 48 hrs (p>0.05). There is statistical difference between two groups at 6 hrs and 18 hrs.
| Study group | Frequency | Percentage |
|---|---|---|
| Group 1 (0.0625% bupivacaine with 2 mcg fentanyl) | 30 | 50% |
| Group 2 (0.125% bupivacaine with 2 mcg fentanyl) | 30 | 50% |
Table 1: Descriptive analysis of study Groups (N=60).
| Name of the diagnosis | Frequency (%) (N=60) |
|---|---|
| Ano-rectal carcinoma | 2 (3.3%) |
| Carcinoma-descending colon | 1 (1.6%) |
| Carcinoma ovary | 26(43.3%) |
| Carcinoma-vulva | 1 (1.6%) |
| Fibroid uterus | 23 (38.3%) |
| Vault prolapse | 3 (5%) |
| Carcinoma endometrium | 4 (6%) |
Table 2: Descriptive analysis for types of diagnosis in study population (N=60).
| Name of the surgery | Frequency (%) (N=60) |
|---|---|
| APR | 1 (1.6%) |
| Cytoreduction | 26 (43.3%) |
| Lap. LAR | 2 (3.3%) |
| PFR | 3 (5%) |
| TAH BSO | 23 (38.3%) |
| TAH BSO frozen | 4 (6%) |
| Vulvectomy BLPLND | 1 (1.6%) |
Table 3: Descriptive analysis for types of surgery in study population (N=60).
| Parameter | Frequency (%) (N=60) |
|---|---|
| L1-2 | 16 (26.6) |
| L2-3 | 44 (73.4) |
Table 4: Descriptive analysis for Site of epidural insertion in study population (N=60).
| Baseline parameter | Study group | P-value | |
|---|---|---|---|
| Group 1 (N=30) (Mean ± SD) |
Group 2 (N=30) (Mean ± SD) |
||
| Pulse rate | 87.56 ± 11.55 | 87.23 ± 9.95 | 0.9 |
| SPO2 | 97.6 ± 2.07 | 96.9 ± 2.53 | 0.06 |
| Respiration rate | 13.83 ± 1.39 | 14.03 ± 1.60 | 0.6 |
| Systolic blood pressure | 129.03 ± 14.4 | 126.66 ± 14.8 | 0.4 |
| Diastolic blood pressure | 84.00 ± 7.3 | 82.93 ± 10.6 | 0.65 |
Table 5: Comparison of mean of baseline parameter between study groups (N=60).
| Time period | Study group | P-value | |
|---|---|---|---|
| Group 1 (N=30) (Mean ± SD) |
Group 2 (N=30) (Mean ± SD) |
||
| Starting | 129.66 ± 14.05 | 135.56 ± 13.71 | 0.1 |
| 3 hours | 125.13 ± 14.55 | 129.83 ± 18.02 | 0.27 |
| 6 hours | 118.36 ± 14.92 | 121.83 ± 18.98 | 0.43 |
| 9 hours | 117.25 ± 15.81 | 113.73 ± 17.74 | 0.43 |
| 12 hours | 114.43 ± 14.40 | 108.83 ± 21.43 | 0.24 |
| 15 hours | 110.63 ± 11.94 | 106.96 ± 18.21 | 0.3 |
| 18 hours | 114.73 ± 15.89 | 108.21 ± 19.02 | 0.16 |
| 21 hours | 113.9 ± 16.10 | 111.31 ± 18.95 | 0.59 |
| 24 hours | 117.2 ± 14.45 | 117.62 ± 19.16 | 0.92 |
| 48 hours | 120.86 ± 17.08 | 117.25 ± 19.87 | 0.46 |
Table 6: Comparison of mean systolic blood pressure between study groups at different time period (N=60).
Infusion was stopped if MAP was less than 60 mm Hg and fluid bolus of 500 ml was given to maintain MAP above 60 mm Hg. Hence after 9 hrs the infusion was stopped for Group 2 and VAS score was assessed with the remaining participants under consideration (Table 7). There is no statistical difference between two groups at starting, 3 hrs, 6 hrs and 9 hrs before the onset of hypoatension and leaving out any participant in view of considered hypotension criteria (Table 8). There is also no statistical difference between two groups at 12 hrs and 15 hrs (P>0.05) (Table 9). There is no statistical difference between two groups at different hrs in parameter of SpO2, (p>0.05). There is statistical difference between two groups from 9 hrs to 48 hrs in parameter systolic blood pressure, diastolic blood pressure (p<0.05). Significant variation in hemodynamics was noted between the patients in whom the infusion was stopped (Table 10). The comparison of VAS was also done between the patients who continued with infusion of Bupivacaine 0.125% with 2% fentanyl and left out patients in whom the infusion was stopped. There is statistical difference between two groups at 12 hrs, 15 hrs, 18 hrs and 24 hrs (P</=0.05) (Table 11).
| Time period | Study group | P-value | |
|---|---|---|---|
| Group 1 (N=30) (Mean ± SD) |
Group 2 (N=30) (Mean ± SD) |
||
| Starting | 84.06 ± 7.38 | 82.86 ± 10.18 | 0.6 |
| 3 hours | 75.13 ± 7.97 | 75.20 ± 7.46 | 0.9 |
| 6 hours | 73.23 ± 4.28 | 77.60 ± 8.37 | 0.01 |
| 9 hours | 74.36 ± 6.22 | 70.36 ± 6.96 | 0.02 |
| 12 hours | 68.76 ± 5.54 | 70.53 ± 9.30 | 0.37 |
| 15 hours | 73.4 ± 6.66 | 73.5 ± 8.30 | 0.9 |
| 18 hours | 75.66 ± 11.80 | 67.85 ± 6.50 | 0.02 |
| 21 hours | 71.5 ± 6.86 | 71.5 ± 6.60 | 0.9 |
| 24 hours | 70.83 ± 6.63 | 73.18 ± 8.19 | 0.24 |
| 48 hours | 72.10 ± 4.98 | 70.92 ± 5.88 | 0.42 |
Table 7: Comparison of mean diastolic blood pressure between study groups at different time period (N=60).
| VAS @ time period | Study group | Man Whitney U test P-value |
|
|---|---|---|---|
| Group 1 (N=30) Median (IQR) |
Group 2 (N=30) Median (IQR) |
||
| Starting | 4 (4 to 4) | 4 (4 to 5) | 0.069 |
| 3 hours | 4 (3 to 4) | 4 (3 to 4) | 0.782 |
| 6 hours | 4 (3 to 4) | 3 (3 to 3) | 0.237 |
| 9 hours | 3 (3 to 3) | 3 (3 to 3) | 0.317 |
Table 8: Comparison of VAS between study groups at different time period (N=60).
| VAS @ time period | Study group | Man Whitney U test P-value |
|
|---|---|---|---|
| Group 1 (N=30) Median (IQR) |
Group 2 (N=21) Median (IQR) |
||
| 12 hours | 3 (3 to 3) | 3 (3 to 3) | 0.655 |
| 15 hours | 3 (3 to 3) | 3 (3 to 3) | 0.655 |
Table 9: Comparison of VAS between study groups at different time period (N=51).
| Parameter at 9 hours | Study group | P-value | |
|---|---|---|---|
| Continued (N=25) (Mean ± SD) |
Stopped (N=5) (Mean ± SD) |
||
| Systolic blood pressure | 117.65 ± 15.68 | 92.20 ± 5.02 | 0.001 |
| Diastolic blood pressure | 73.70 ± 5.72 | 60.00 ± 2.00 | 0.001 |
| SpO2 | 97.07 ± 0.66 | 97.20 ± 0.44 | 0.677 |
| Parameter at 12 hours | Continued (N=24) (Mean ± SD) |
Stopped (N=6) (Mean ± SD) |
|
| Systolic blood pressure | 113.83 ± 17.94 | 93.33 ± 6.02 | 0.008 |
| Diastolic blood pressure | 70.01 ± 7.98 | 66.33 ± 2.33 | 0.029 |
| SpO2 | 96.24 ± 1.62 | 97.33 ± 1.21 | 0.116 |
| Parameter at 15 hours | Continued (N=21) (Mean ± SD) |
Stopped (N=9) (Mean ± SD) |
|
| Systolic blood pressure | 111.04 ± 15.02 | 94.75 ± 8.48 | 0.004 |
| Diastolic blood pressure | 73.94 ± 6.69 | 67.25 ± 6.13 | 0.01 |
| SpO2 | 96.56 ± 0.94 | 94.50 ± 3.62 | 0.001 |
| Parameter at 18 hours | Continued (N=21) (Mean ± SD) |
Stopped (N=9) (Mean ± SD) |
|
| Systolic blood pressure | 113.80 ± 17.52 | 95.43 ± 6.70 | 0.008 |
| Diastolic blood pressure | 72.66 ± 10.71 | 66.28 ± 3.72 | 0.126 |
| SpO2 | 96.80 ± 1.41 | 97.42 ± 0.97 | 0.264 |
| Parameter at 21 hours | Continued (N=18) (Mean ± SD) |
Stopped (N=12) (Mean ± SD) |
|
| Systolic blood pressure | 116.92 ± 15.75 | 92.40 ± 8.63 | 0.001 |
| Diastolic blood pressure | 72.43 ± 7.36 | 67.00 ± 7.95 | 0.041 |
| SpO2 | 96.54 ± 1.96 | 96.30 ± 2.21 | 0.731 |
| Parameter at 24 hours | Continued (N=18) (Mean ± SD) |
Stopped (N=12) (Mean ± SD) |
|
| Systolic blood pressure | 120.17± 16.77 | 103.11 ± 3.29 | 0.004 |
| Diastolic blood pressure | 72.91 ± 7.21 | 68.00 ± 6.83 | 0.064 |
| SpO2 | 97.02 ± 1.81 | 96.22 ± 2.22 | 0.247 |
| Parameter at 48 hours | Continued (N=18) (Mean ± SD) |
Stopped (N=12) (Mean ± SD) |
|
| Systolic blood pressure | 122.33 ± 18.33 | 102.22 ± 2.72 | 0.002 |
| Diastolic blood pressure | 72.31 ± 4.92 | 67.44 ± 6.36 | 0.012 |
| SpO2 | 97.41 ± 1.41 | 96.33 ± 2.29 | 0.063 |
Table 10: Comparison of SPO2, Blood pressure at 9 hours to 48 hours between study groups of 0.125% Bupivacaine with 2% fentanyl and left out participants at different time period (N=60).
| VAS | Study group 0.125% bupivacaine with 2% fentanyl | Man Whitney U test P-value |
|
|---|---|---|---|
| Continued (N=25) Median (IQR) |
Stopped (N=5) Median (IQR) |
||
| 9 hours | 3 (3 To 3) | 3 (3 To 3) | 0.95 |
| Study group | |||
| Continued (N=24) Median (IQR) |
Stopped (N=6) Median (IQR) |
||
| 12 hours | 3 (3 To 3) | 4 (3 To 4) | 0.05 |
| Study group | |||
| Continued (N=21) Median (IQR) |
Stopped (N=9) Median (IQR) |
||
| 15 hours | 3 (3 To 3) | 3 (3 To 3.7) | 0.02 |
| Study group | |||
| Continued (N=21) Median (IQR) |
Stopped (N=9) Median (IQR) |
||
| 18 hours | 3 (3 To 3) | 4 (3 To 5) | 0.05 |
| Study group | |||
| Continued (N=18) | Stopped (N=12) | ||
| Median (IQR) | Median (IQR) | ||
| 21 hours | 3 (3 To 3) | 3 (3 To 4) | 0.52 |
| Study group | |||
| Group 1 (N=18) Median (IQR) |
Group 2 (N=12) Median (IQR) |
||
| 24 hours | 3 (3 To 3) | 5 (3 To 5) | 0.01 |
| 48 hours | 3 (3 To 4) | 4 (3 To 4) | 0.27 |
Table 11: Comparison of VAS from 9 hours to 48 hours between study groups of 0.125% Bupivacaine with 2% fentanyl and left out participants at different time period (N=60).
Cleland was the first to describe the use of an epidural catheter for postoperative analgesia with intermittent doses of local anaesthetic solutions. As this technique was associated with fluctuating levels of analgesia and significant sympathetic blockade, continuous infusion of local anaesthetic was subsequently recommended as an alternative. Placement of epidural also reduces the cortisol level and hence improved postoperative duration [5]. Block of afferent neural input from the site of surgery with epidural analgesia has a beneficial effect in reducing the neuro-hormonal aspect of the surgical stress response, with the potential for a reduction in respiratory, thromboembolic, and cardiovascular events after major surgery [6].
Bupivacaine became popular in the 1980s for epidural blocks because it was better than the previously available long-acting agents in producing adequate antinociception without profound inhibition of motor activity, particularly when dilute solutions are used [7]. Bupivacaine is widely used epidurally for obstetric analgesia and postoperative pain management because it can provide acceptable analgesia with only mild muscle weakness [8].
The volume and concenteration of anesthetic solution probably influences the spread of anesthesia. 0.125% bupivacaine produce adequate postoperative analgesia in many clinical settings with only mild motor deficits [8]. Continuous epidural infusions of bupivacaine as dilute as 0.0625% to 0.1% are useful for labor epidural analgesia, especially when administered in combination with opioids and epinephrine [9]. Bupivacaine 0.25% may be used for more intense analgesia (particularly during combined epidural-general anesthesia cases) with moderate degrees of motor block.
Bupivacaine at concentrations of 0.5% to 0.75% is associated with a more profound degree of motor block, and surgical anesthesia [10]. It should be emphasized that although high concentrations of local anesthetics may be appropriate for episodic bolus dosing for surgery, these concentrations (i.e., 0.25% for bupivacaine) should not be first choice for continuous epidural infusions [3]. In some patients, increasing the local anesthetic dose or addition of adjuvants such as epinephrine and lipophilic opioids is necessary to achieve adequate block intensity [11]. Bolus injections produce much more cephalocaudad spread than continuous infusions do [1]. When concentrated bupivacaine solutions are used for infusions, they have the potential for excessive local effect with an associated risk for unwanted and very prolonged motor blockade and hemodynamic changes. The common side effects of neuraxial blockade or epidural in this case are Hypotension, Bradycardia [12]. Study also raised concerns of hypotension [13]. This depends upon the concentration of the drug or local anaesthetic used too. A common physiologic effect of epidural and spinal anesthesia is hypotension, primarily due to blockade of the sympathetic nervous system causing arterial and venous vasodilation with subsequent “functional” hypovolemia [7]. Previous studies during experimental hypovolemia have found a capillary refill to occur within 5 min and short-term studies (20-30 min) with and without concomitant fluid administration after lumbar epidural anesthesia [10].
In this study we intend to see the effects of different concentrations of bupivacaine in lumbar epidural analgesia in patients who underwent lower abdominal surgeries. After doing a pilot study we saw a stoppage of infusion of 0.125% of bupivacaine with 2 μg fentanyl in view of hypotension after 8 to 10 hrs and the whole purpose of using this epidural concentration had gone unused. Hence we studied and compared the effect of 0.0625% bupivacaine with 2% fentanyl and 0.125% bupivacaine with 2% fentanyl epidural infusion on haemodynamic parameters in infraumbilical surgeries, with the aim of keeping haemodynamics preserved and to achieve favourable VAS score [8].
A total of 60 patients were studied. Among the study population, 30 (50.00%) had 0.0625% bupivacaine with 2 μg fentanyl and remaining 30 (50.00%) participants had 0.125% bupivacaine with 2 μg fentanyl (Figure 1).
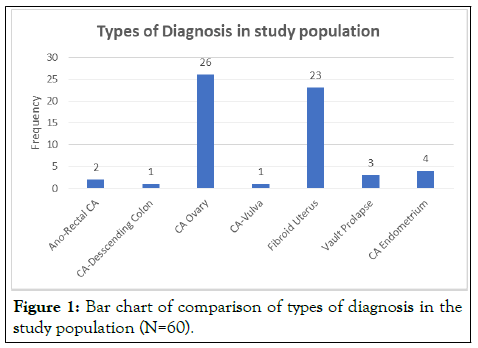
Figure 1: Bar chart of comparison of types of diagnosis in the study population (N=60).
Among Study Population, 26(43.3%) underwent Cytoreduction surgery, 23(38.3%) underwent TAH BSO surgery followed by 4(6%) of them underwent TAH BSO Frozen surgery (Table 5).
When taken into consideration of whole 60 patients there is no statistically significant difference between two groups in parameters of Pulse Rate, Respiration rate, Systolic Blood Pressure (P>0.05). However the Diastolic Blood pressure was statistically significant after 6 hrs, 9 hrs and 18 hrs [14]. The study by Duncan et al. [13,14] Also showed that significant quantity of 62% within 24 hrs had hypotension. But this study mentioned significant difference in VAS of 3.8 against 2.5 in 0.0625% bupivacaine against 0.125% respectively. However this study didn’t use fentanyl in their preparation.
There is no statistical difference in mean epidural infusion volume between two groups at starting period, 3 hrs, 6 hrs, 9 hrs (p>0.05). There is statistical significance difference in mean epidural infusion volume between two groups at 12 hour and 15 hrs, 18 hrs, 21 hrs, 24 hrs 48 hrs (p<0.05). This was due to stoppage of infusion in group 2 after 9 hrs till 21 hrs. At starting in Group 1 the mean of Epidural infusion is 7.93 ± 1.20 and in Group 2, the mean of Epidural infusion value is 5.60 ± 1.40 which showed the epidural run in between 5 to 7 ml/hr and occasionally to 12 ml/hr in Group 1.
There is no statistical difference of VAS between two groups at starting, 3 hrs, 6 hrs and 9 hrs. Further the study entailed comparison of hemodynamic parameters and VAS among the patients in whom the infusion had to be stopped with other patients in whom bupivacaine 0.125% with 2 μg % fentanyl was continued (Figure 2).
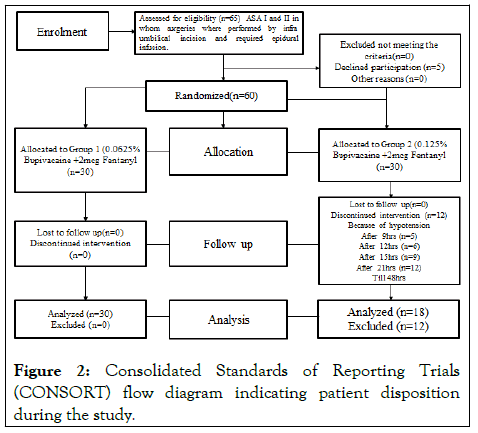
Figure 2: Consolidated Standards of Reporting Trials (CONSORT) flow diagram indicating patient disposition during the study.
The stoppage of epidural infusion in group 2 started after 9 hrs in 5 patients and increased to 9 at 18 hrs and further to 12 after 21 hrs. There is significant statistical difference between the two groups after 9 hrs, 12 hrs, 15 hrs and 48 hrs in parameter of systolic blood pressure, diastolic blood pressure (p<0.05). After 48 hrs, in Group 1 the mean of diastolic blood pressure value is 72.31 ± 4.92 and in Group 2, the mean of diastolic blood pressure value is 67.44 ± 6.36. 48 hrs, in Group 1 the mean of systolic blood pressure value is 122.33 ± 18.33 and in Group 2, the mean of systolic blood pressure value is 102.22 ± 2.72. Study also showed that 50% of participants had hypotension in Bupivacaine group and 26% had hypotension in Ropivacaine group which is significant as compared to 0.0625% of Bupivacaine [15].
However there was no statistically significant difference in VAS. The study also followed the same concentration as in our study and found no significant change in VAS. There were no other side effects like lower limb weakness, nausea vomiting as studied in other studies [8]. That continuous infusion as compared to intermittent boluses provided better pain relief at rest, on movement and provided sustained degree of analgesia. The motor block was more pronounced in higher concentration of bupivacaine like 0.125% and this was also one of the causes for stoppage of infusion of 0.125% Bupivacaine [16]. Four patients in the bupivacaine group developed hypotension, of which two patients required temporary withholding of infusion. This showed that we could achieve satisfiable VAS score in group 1 with 0.0625% of Bupivacaine with 2 μg of fentanyl with preserved haemodynamic parameters. On the contrary there was need to stop the infusion in group 2 in 12 patients in view of hypotension which led to increase in VAS score and discomfort due to pain which rendered the infusion useless.
In view persisting hypotension found with Bupivacaine Epidural analgesia of concentration of 0.125% in several studies and leading to stoppage of infusion. Hence the effect of two different concentrations of Bupivacaine of 0.125% and 0.0625% with opioids of 2 μg/ml was studied on hemodynamic parameters of patient leading to stoppage of infusion in two different groups. The secondary aim was to see whether this will impact the VAS of the patient. The study showed that the infusion of 0.125% bupivacaine with 2 μg fentanyl lead to stoppage of infusion in 12 patients in view of Hypotension and no significant changes in VAS score was noted in two groups of patients. However there was significant change in VAS noted when compared among the patients in whom 0.125% bupivacaine with 2% fentanyl infusion was stopped against the patients in whom it was continued.
NIL
NIL
[Crossref]
Citation: Neik S, John M, Kapil K, Roj T (2022) Comparison between Effect of 0.0625% Bupivacaine With 2% Fentanyl And 0.125% Bupivacaine With 2% Fentanyl Epidural Infusion on Haemodynamic Parameters in Infraumbilical Surgeries. J Anesth Clin Res. 13:1085.
Received: 30-Sep-2022, Manuscript No. JACR-22-19926; Editor assigned: 05-Oct-2022, Pre QC No. JACR-22-19926 (PQ); Reviewed: 21-Oct-2022, QC No. JACR-22-19926; Revised: 28-Oct-2022, Manuscript No. JACR-22-19926 (R); Published: 04-Nov-2022 , DOI: 10.35248/2155-6148.22.13.1085
Copyright: © 2022 Neik S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.