
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 5
Background: Earlier electroconvulsive therapy was performed without any muscle relaxant so the patient required physical restraining during the seizure and experienced severe muscle pain after the procedure. To prevent myalgia and musculoskeletal complications (eg: Bone fractures or dislocations), muscle relaxants are often administered during ECT procedures. ECT with Anaesthesia and Muscle Relaxants is called Modified ECT. The type of anaesthetic agent may have a significant impact on efficacy of the treatment. The aim is to provide a short duration of unconsciousness and adequate muscle relaxation with rapid and complete return of cognitive function. Propofol has shorter induction time and rapid and smooth recovery while Etomidate has longer seizure duration and stable haemodynamics. In this study we compare Etomidate and Propofol for motor seizure duration and haemodynamic stability during electroconvulsive therapy.
Objective: A type of prospective Double blind Randomised controlled trial carried out at tertiary care unit during 2020- 2021 with 60 adult patients, after taking approval of Institutional Ethical Committee(Ref no. IEC/Certi/03/01/2021) and written informed consent in their own language according to institutional protocols and explaining the cause, pathology and consequences of the process.
Materials and methods: In this Prospective, Randomized controlled study on 60 patients of 18 to 65 years and either sex after matched inclusion criteria with American society of Anaesthesiologists class I, II and III, who were undergo modified electroconvulsive therapy Patients are divided in to two groups, Group P (n=30) and group E (n=30) in which electroconvulsive therapy was carried out using Propofol 1.5 mg/kg and Etomidate 0.2 mg/kg respectively. Motor seizure duration and haemodynamic Parameters were measured at different time interval. Statistical analysis was done by using SPSS Statistical Software version 24.0. Mean and standard deviation were calculated. Unpaired ‘t’ test were applied between Group P and Group E. p value of <0.05 is considered statistically Significant and p value<0.001 was considered statistically highly significant.
Results: Mean Motor seizure duration was longer with Etomidate (42.73 ± 9.19) as compared to Propofol (32.36 ± 6.01) and the difference was statistically highly significant (P<0.001) there was less changes in haemodynamic parameters with etomidate as compared with propofol.
Conclusion: Etomidate has longer seizure duration and stable haemodynamics compared to propofol during modified electroconvulsive therapy. It can be useful when seizures are too short and sub therapeutic inspite of maximum stimuli.
Electroconvulsive therapy; Motor seizure; Etomidate; Propofol
Electroconvulsive Therapy (ECT) first described in 1938, performed without anaesthesia for almost 30 years. During ECT, an electrical current is applied transcutaneously to the brain via two electrodes positioned either bilaterally or unilaterally to induce a generalized seizure with characteristic EEG changes in which bilateral is preferred. Too short (<10 s) or too long (>120 s) seizure duration may affect clinical efficacy but studies suggest that the amount of current delivered is more important than length of seizure. ECT is performed twice weekly. (On average, 3-4 weeks) [1]. Its indications include Acute, life threatening depression, Drug resistant depression, Acute catatonia, Mania and contraindicated in myocardial infarction (<3 months), cerebrovascular accident (<1 month ) Raised intracranial pressure, Pheochromocytoma, highrisk pregnancies, etc [2], numerous psychological, psychoanalytical and biological theories to explain the therapeutic effect of ECT. Among neurotropic factors BDNF has role in mediating the effects of ECT. BDNF is a nerve growth factor classified under neurotrophin class, mediates neuronal growth, proliferation, repair and survival. ECT is useful for normalization of neuroendocrine dysfunction in depression. Expression of genes, functional connectivity, neurochemicals, permeability of blood-brain-barrier, alteration in immune system has been suggested to be responsible for the therapeutic effects of ECT [3].
After the Institutional Ethics Committee's approval and written informed consent of patient in their own vernacular language, This Prospective Randomized, double-blind study was conducted on 60 patients of 18 to 65 years of age, either sex, ASA grade I,II and III who were posted for modified electroconvulsive therapy. Patients having Severe hepatic and/or renal insufficiency, Brain organic disease, Cardiac insufficiency, Sick sinus syndrome, Bradycardia, Atrioventricular block of degree II and III, Neuromuscular disorders, Patient refusal, ASA grade 4, 5 at Age <18 year or >65 year are excluded. Written informed consent was obtained from all patients in preoperative area.
Patients were equally divided in to two groups, group P patients received intravenous Propofol 1.5 mg/kg and group E patients received intravenous Etomidate 0.2 mg/kg. To follow the double blind nature of study drugs were prepared by anaesthesiologist who was not attending the electroconvulsive therapy and the anaesthesiologist who attended the electroconvulsive therapy and recorded the data was blind to both groups assigned. All patients thoroughly assessed for history, and examined in detail, both general and systemic examination. Venous access obtained with 20 G cannula and intravenous ringer lactate started, basic monitors will be attached like NIBP, pulse oxymetry, ECG and vitals of patient will be recorded. All the patients were premedicated with Inj. ondansetron 80 ug/kg IV, Inj. glycopyrrolate 4 ug/kg IV.
All patients were oxygenated with 100% oxygen before anaesthesia induction. Anaesthesia induction was performed with intravenous 1.5 mg/kg Propofol (Group-P) and intravenous 0.2 mg/kg Etomidate (Group-E). Subsequent to loss of consciousness, 0.7 mg/kg succinylcholine was administered. Assisted ventilation via face mask was performed using 100%oxygen at a flow rate of 8 L/ min for all patients during the ECT procedure. A bite block was used to protect the patients' teeth, lips, and tongue from injury caused by the contraction of facial muscles.
When neuromuscular response was completely blocked, ECT was performed with bitemporal electrodes on forehead. There was an interval of two or three days between each ECT sessions. All the patients were monitored for changes in HR, MAP, RR, SPO2, ECG changes before induction of anesthesia, after induction, after applying ECT at 1, 3, 5, 10 min and then throughout the procedure till shifting of the patient to post anesthesia care unit(PACU). Induction time was recorded as the time from injecting i.v. anesthetic agent till loss of verbal contact. The duration of motor seizure was recorded as the time from the ECT stimulus to the cessation of tonic clonic motor activity. Recovery parameters were noted-1) time to return of spontaneous ventilation was assessed as the time from i.v. administration of anesthetic agent until the presence of the patient's breathing efforts. 2) Duration of recovery was assessed as the time from i.v. administration of anesthetic agent to the time taken to obey commands such as eye-opening. The postoperative assessment was done with emergence agitation score graded as (i) sleeping, (ii) awake and calm, (iii) irritable and crying, (iv) inconsolable crying, and (v) severe restlessness and disorientation. Any side effects such Nausea, Vomiting, Headache, Agitation, Bradycardia, Tachycardia, Hypotension, Respiratory depression, Oxygen desaturation were noted.
Statistical analysis was done by using SPSS Statistical Software version 24.0. Mean and standard deviation were calculated. Unpaired‘t’ test were applied between Group P and Group E. p value of <0.05 was considered statistically Significant and p value<0.001 was considered statistically highly significant (Figure 1).
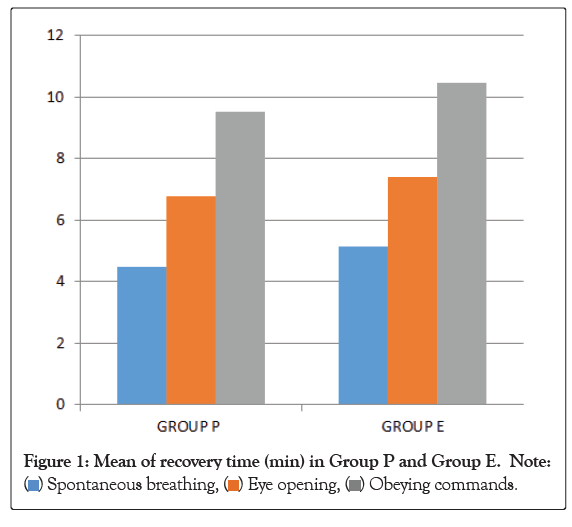
Figure 1: Mean of recovery time (min) in Group P and Group E. Note:
Table 1 shows, demographic data in group P mean age was 39.13 years with SD 12.75, in group E mean age was 34.36 year and SD 9.85 which was statistically insignificant. In group P mean weight was 57.96 kgs with SD 7.59 in group E mean weight was 58.9 kgs and SD 8.37 which was statistically insignificant. In group P 14 was male and 16 were female, in Group E 12 were male and 18 were female.
| Mean demographic data | Group P (Mean ± SD) | Group E (Mean ± SD) | P-Value |
|---|---|---|---|
| Age | 39.13 ± 12.75 | 34.36 ± 9.85 | 0.11 (NS) |
| Weight | 57.96 ± 7.59 | 58.9 ± 8.37 | 0.65 (NS) |
| ASA Grade | |||
| 1 | 7 | 6 | 0.86 (NS) |
| 2 | 11 | 14 | |
| 3 | 12 | 10 | |
| Sex | |||
| Male | 14 | 12 | - |
| Female | 16 | 18 | |
Table 1: Mean demographic data in Group P and Group E. Note: All variables except ASA status and sex are expressed as mean ± SD. *(p-value<0.05 is considered significant, p-value >0.05 is considered Non Significant), (NS-Not Significant, SD-Standard Deviation).
Table 2 shows the mean of seizure duration in group P was 32.36 ± 6.01 and group E was 42.73 ± 9.19. It was found to be statistically highly significant (p<0.001).
| Duration of seizure | Group P Mean ± SD | Group E Mean ± SD | P-Value |
|---|---|---|---|
| 32.36 ± 6.01 | 42.73 ± 9.19 | <0.001 (HS) | |
Table 2: Comparison of motor seizure duration between Group P and Group E in seconds. Note: *(p-value<0.05 is considered significant, p-value <0.001 is considered Highly Significant), (HS=Highly Significant, SD- Standard Deviation).
Table 3 shows the means of peri procedural heart rate were statistically insignificant in group P and group E before induction with p-value >0.05. significant increase in heart rate in group P than group E after induction at, 0 seconds, 1 min, 3 min, 5 min, 10 mins with P value <0.05.
| Comparison of heart rate | Group P Mean ± SD | Group E Mean ± SD | P-Value |
|---|---|---|---|
| Before premedication | 81.73 ± 6.59 | 83.06 ± 6.84 | 0.44 (NS) |
| After induction | 93.53 ± 7.25 | 87.2 ± 6.86 | 0.001 (HS) |
| After ECT (0 Min) | 97.6 ± 7.97 | 90.8 ± 6.97 | 0.0009 (HS) |
| 1 Min | 101.2 ± 8.21 | 93.33 ± 7.47 | 0.0003 (HS) |
| 3 Min | 101.27 ± 9.23 | 94.2 ± 7.35 | 0.0018 (HS) |
| 5 Min | 99.46 ± 9.26 | 93.06 ± 7.23 | 0.0042 (S) |
| 10 Min | 98.13 ± 9.46 | 92.8 ± 7.47 | 0.0186 (S) |
Table 3: Comparison of peri-procedural heart rate status of patient in Group P and Group E. Note: (p value>0.05 is considered Non significant, p value<0.05 is considered significant, p value<0.001 is considered Highly Significant), (NS- Not Significant, S=Significant, HS=Highly Significant, SD- Standard Deviation).
Table 4 shows the means of peri procedural mean of mean arterial blood pressure were statistically insignificant in group P and group E before induction with p value>0.05, significant fall in mean arterial blood pressure after propofol as compared to etomidate.
| Before and after medication | Group P Mean ± SD | Group E Mean ± SD | P-Value |
|---|---|---|---|
| Before premedication | 91.57 ± 7.11 | 93.28 ± 6.70 | 0.34 (NS) |
| After induction | 83.66 ± 6.77 | 90.51 ± 6.41 | 0.0002 (S) |
| After ECT (0 Min) | 92.44 ± 5.32 | 95.26 ± 5.52 | 0.048 (S) |
| 1 Min | 94.37 ± 5.28 | 95.51 ± 5.38 | 0.41 (NS) |
| 3 Min | 89.48 ± 9.89 | 93.44 ± 5.80 | 0.063 (NS) |
| 5 Min | 88.62 ± 5.08 | 92.22 ± 5.94 | 0.014 (S) |
| 10 Min | 86.15 ± 4.77 | 91.15 ± 5.52 | 0.0004 (HS) |
Table 4: Comparison of Peri-procedural mean of mean arterial blood pressure in Group P+ Group E.
Chart 1 show the mean of recovery of spontaneous breathing in group P was 4.5 ± 1.13 and group E was 5.13 ± 1.52. The mean of recovery time of eye opening in group P was 6.76 ± 1.27 and group E was 7.4 ± 1.49. The mean of recovery time of obeying commands in group P was 9.53 ± 1.61 and group E was 10.46 ± 2.06. Group P had early recovery than group E but It was found to be statistically insignificant (p>0.05).
The goal of modified ECT is to induce a generalized seizure. Although all anaesthetic agents have anticonvulsant properties because of their effects on the gamma-amino butyric acid receptors and may interfere with outcome of ECT. Thus ECT is very challenging for an anaesthesiologist.
In our study, we found significantly longer seizure duration with etomidate compared to propofol during modified electroconvulsive therapy. The mean of seizure duration with propofol was 32.36 ± 6.01 seconds and etomidate was 42.73 ± 9.19 seconds. Our results are similar with a study conducted by Mir et al. and Canbek et al. in which mean motor seizure duration was significantly longer in Etomidate as compared to Propofol group (P<0.0001) [4] and A study conducted by Avramov et al. of comparative effects of methohexital, Propofol, and Etomidate during electroconvulsive therapy found that the duration of motor seizure was longest after Etomidate and shortest after Propofol (P<0.05) [5].
In our study, induction was smooth with Propofol and after induction, there was a significant fall in MAP and a significant increase in HR in the Propofol group as compared to the Etomidate group (P<0.001). this result were comparable to study done by Jindal et al. found a significant decrease in MAP and a significant increase in HR from baseline to induction in the Propofol group as compared to the Etomidate group [6] and A study done by Zahavi and Dannon found stable haemodynamics with Etomidate as compared to Propofol and thiopental [7].
The propofol group had early and smooth recovery as compared to etomidate but the difference was statistically insignificant (P>0.05). Our results are similar with studies conducted by Seema Jindal et al. in which Propofol has the advantage of having shorter induction time and rapid and smooth recovery as compared to Etomidate [6] and study with Avramov et al. that found the duration of ECT induced seizure is the primary determinant of early recovery rather than the dose of the hypnotic drug, so., comparatively faster recovery observed with Propofol as compared to etomidate in the present study.
The medications used for the treatment of the psychiatric patients cause sedation and may reduce the seizure threshold, the interaction of psychoactive medications with Propofol and Etomidate could not be ruled out and Seizure duration was obsereved by clonic movements using the stopwatch which were a limitation of our study.
Since electroconvulsive therapy is a short procedure and can be completed in 8-10 minutes, the anaesthetic agents used should have a rapid onset, short action and smooth recovery. In this study, we conclude that Etomidate has a longer seizure duration and stable haemodynamics whereas Propofol has shorter induction time and rapid and smooth recovery. So propofol may useful in elderly patients since it provides a more rapid recovery of cognitive function and etomidate is useful when seizures are too short.
Citation: Mansuri Y, Dave J (2022) Comparision of Etomidate and Propofol for Motor Seizure Duration during Modified Electroconvulsive Therapy. J Anesth Clin Res. 13:1063
Received: 03-May-2022, Manuscript No. JACR-22-16740; Editor assigned: 05-May-2022, Pre QC No. JACR-22-16740(PQ); Reviewed: 20-May-2022, QC No. JACR-22-16740; Revised: 27-May-2022, Manuscript No. JACR-22-16740(R); Published: 06-Jun-2022 , DOI: 10.35248/2155-6148.22.13.1063
Copyright: © 2022 Mansuri Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.