
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2023)Volume 14, Issue 3
Introduction: Transcutaneous Laryngeal Ultrasonography (TLUSG) can be used as an alternative to direct laryngoscopy.
Objective: To compare TLUSG and direct laryngoscopy in accessing the vocal cord mobility of elective thyroidectomy patients in the immediate postoperative period.
Methods: A total of 40 patients were enrolled in the study. All of them underwent indirect laryngoscopy and TLUSG pre-operatively. Patients with known vocal cord pathologies were excluded. All Patients underwent both TLUSG and Direct Laryngoscopy (DL) at extubation and indirect and TLUSG at discharge. During the examinations the movement of vocal cords was graded. Grade I: both vocal cords had normal movement; grade II: greater than or equal to one vocal cord had decreased movement; and grade III ≥ one vocal cord had no movement. To assess accuracy, TLUSG findings were correlated with direct laryngoscopy findings. Hemodynamic parameters and patients’ comfort were assessed during both the procedures. Paired t test, and Chi-square test were used as applicable to analyse data.
Results: No patient had preoperative Vocal Cord Palsy (VCP), and 3(7.5%) had unilateral postoperative VCP of which only 2(5%) were detected by direct laryngoscopy. The overall postoperative VCP rate in the immediate postoperative period was 7.5%. TLUSG failed to assess VCs in 3 (7.5%) postoperatively at extubation. But, could assess all the patients 100% when it was done at discharge. Out of the three vocal cord palsy as diagnosed at extubation one (2.5%) was resolved, 2(5%) were picked up by TLUSG of which only one (5%) was detected by indirect laryngoscopy. Sensitivity and specificity of TLUSG at extubation was 97.42%, 66%, respectively and at discharge was 97.2%, 100% respectively. Hemodynamic parameters and patients reactivity score was better while performing TLUSG .
Conclusion: TLUSG is an upcoming diagnostic modality which is cheap, non-invasive and comfortable to the patient and can assess the vocal cord function in the post thyroidectomy patients accurately.
Direct laryngoscopy; Recurrent laryngeal nerve; TLUSG; Vocal cords
As per analysis from various studies 42 million people are affected by any one of the thyroid disorders [1]. Infection, hemorrhage, hypoparathyroidism hoarseness of voice, nerve injury, and airway obstruction are known complications of thyroid surgery. The right and left Recurrent Laryngeal Nerve (RLN) that supply all the intrinsic muscles of the larynx except the cricothyroid are at risk of being injured during the dissection of the thyroid gland. The anatomy of the RLN is highly flexible, leading to a high risk for of damage. Identifying RLN during the surgery and is crucial to prevent any unwanted damage to the laryngeal nerves [2]. The prevalence of symptomatic vocal cord palsy preoperatively ranges from 1%-6% and asymptomatic vocal cord palsy ranges from 0%-11%. Based on study by Chandrashekhar et al. the sensitivity and specificity of the voice symptoms in identifying the vocal cord symptoms is as low as 33% and 83% respectively [3,4]. Documenting any palsy of the unilateral or bilateral vocal cords before and after the surgery is important to avoid medicolegal issues [5]. Traditionally the assessment of vocal cord mobility perioperatively was being done using indirect and direct laryngoscopes. Multiple modalities have been designed to assess the movement of vocal cords and thereby detect a palsy like fibre optic bronchoscope [7] ,digital palpation of twitch response at RLN excitation, and Electro-Myogramph (EMG) of laryngeal musculature. Use of endotracheal tube equipped with electrodes, Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Ultrasonography [4,5,8] . Over the last century, the dynamics of vocal cord testing have shifted from invasive to non- invasive procedures. The wide analysis of literature portrays various methods that can be used in the perioperative setting by anesthesiologists as well as surgeons to evaluate the functionality of the recurrent laryngeal nerve by examining the vocal cord mobility.
The primary objective of our study was to compare the Transcutaneous Laryngeal Ultrasonography (TLUSG) and direct laryngoscopy in accessing the vocal cord mobility of thyroidectomy patients in the immediate postoperative period. The secondary object was to assess the hemodynamic changes and patient comfort while examining the vocal cords was the secondary purpose.
This prospective study was conducted after obtaining ethics and research committee approval (48) and informed consent was taken from all the subjects enrolled from otorhinolaryngology department of tertiary care teaching hospital for a period of one year. The trial was registered before patient enrollment with clinical trial registry- India (ctrl.nic.in) vide registration number (REF/2021/10/048301). Patients who were undergoing elective thyroidectomies in the age group of 18-65 years, of either sex or belonging to American society of anesthesiologist physical status grade (ASA PS) I and ll were included in Figure 1. All the Patients under went indirect laryngoscopy in outpatient basis to document the vocal cords motility prior to surgery. Patients with pre-existing palsy were not included in the study. Patients belonging to the ASA PS III and IV, patients with extensive malignancies, Mallampati grade III, IV and presence of neurological disease affecting vocal cord function preoperative voice abnormalities, patients with hepatic, renal or cardiopulmonary abnormalities, seizures, patients with limited neck motility , Patients with surgical history in neck region, were also excluded.
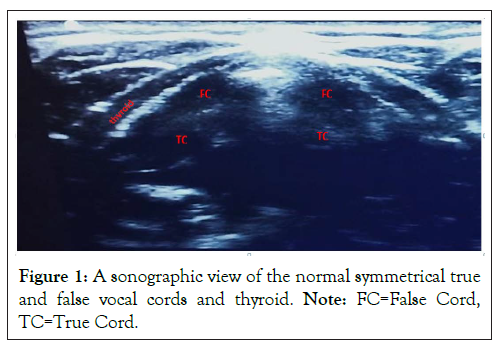
Figure 1: A sonographic view of the normal symmetrical true and false vocal cords and thyroid. Note: FC=False Cord, TC=True Cord.
The participants in this study underwent routine pre anesthesia checkup. The complete explanation of study design was done and written informed consent was obtained. Patients were explained Transcutaneous Laryngeal Ultrasonography (TLUSG) and the maneuvers they would be asked to perform in detail. The patients were made to lie in the supine position. Routine monitors were attached and baseline readings of Heart Rate (HR), Systolic Blood Pressure (SBP), diastolic blood pressure (DBP), Mean Arterial Pressure (MAP), End-Tidal Carbon Dioxide (EtCO2) was noted. A preliminary USG scan was performed by an experienced anaesthesiologist who is trained in TLUSG, and who has performed a minimum of 40 TLUSG under supervision. This anesthesiologist was not included in the further study. Under all aseptic precautions and after applying adequate ultrasound gel, a linear USG transducer of 6-13Hz was placed perpendicular to the trachea to identify the normal structures present in the neck like the carotids, Juglar veins, arytenoids. Then, the transducer was kept horizontally in the center of the neck and thyroid cartilage and scanned caudo-cranially till both Vocal Cords (VC)s were visualized. Sonographic landmarks of vocal cords, namely False Cords (FC) and Arytenoids (AR), were identified for the assessment of vocal cord mobility (Figure 1).
All the subjects were told to do three maneuvers 1) quiet normal respiration 2) phonation with ‘‘a’’ sound 3) Valsalva .During the Valsalva maneuver, the patient was asked to take a deep breath and then hold the breath and bear down. Normally, VCs are approximated symmetrically in the midline during the Valsalva maneuver. After that, patients were asked to relax and VCs would relax. Symmetrical adduction and abduction of both VCs confirmed the motility of the vocal cords was graded from I to III. All patients were induced and maintained as per standard anesthesia Protocols. All the necessary hemodynamic parametric monitoring modalities were connected. Towards the end of the surgery 15 minutes before the last sutures, sevoflurane was tuned off, injection: fentanyl 50 mcg was given intravenously and residual neuromuscular blockade was reversed by a mixture inj neostigmine 2.5 mg, and injection glycopyrrolate 0.4 mg. The airway reflexes were assessed and extubation criteria were checked (arousable, absence of tachypnea, no coughing on tube). Laryngoscopy was then performed during extubation and vocal cords were visualized and mobility of vocal cords was assessed by vocal cord visualization and mobility grade as follows (21): peripheral capillary oxygen saturation (SpO2) and electrocardiography. 1A=Full glottis visualized with normal abduction of cords 2A=Partial.
Glottis visualized with normal abduction of cords 1B=Full glottis visualized with partial immobility of cords 2B=Partial glottis visualized with partial immobility of cords 1C=Full glottis visualized with complete immobility of cords 2C=Partial glottis visualized with complete immobility of cords.
Patient comfort during the procedure was assessed using patient’s reactivity score as follows: (24)1-No grimace, 2-Grimacing facial expressions, 3-Discomforting head movements, 4-Protective head and limb movements, 5-Cough and gagging.
Hemodynamic parameter like HR, SBP, DBP, MAP and RR were noted just at the extubation and also at 1 minute thereafter at 5 minutes. Then the patient was extubated after adequate extubation criteria were met. After the extubation the patient, the neck was painted with sterile antiseptic solution (betadine) thrice and under strict aseptic precautions after scrubbing gown and gloves neck was scanned with a high- frequency linear probe (frequency: 6-13 Hz). Adhesive transparent dressing filled with ultrasound gel was applied to the linear transducer and a sterile probe cover was used to cover the remaining of transducer to maintain asepsis during scanning. TLUSG was performed the similar way as described above and vocal cord motility was graded again by a different anaesthesiologist who is experienced in TSULG as described above. Both the anaesthesiologists will not be aware of each other’s findings. During the procedure, the heart rate, blood pressure, and oxygen saturation were recorded before the start of TLUSG and thereafter every minute till the scanning is complete. The duration of the procedure and any discomfort were noted. The surgical dressing was kept aseptically afterward. The vocal cord mobility of all the patients was assessed with indirect laryngoscopy and transcutaneous laryngeal ultrasound again at discharge to confirm the previous findings (Figure 2).
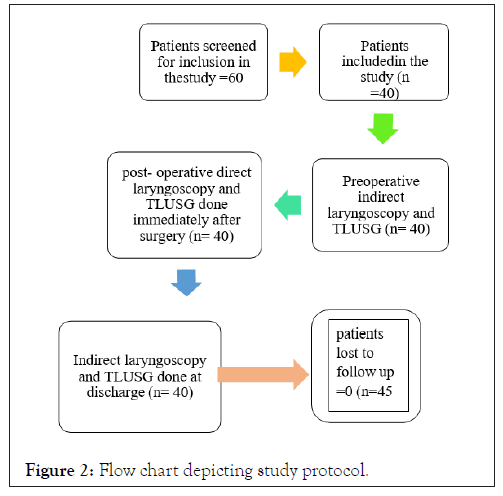
Figure 2: Flow chart depicting study protocol.
Statistical analysis
The study of Wong, et al. [4] observed that the sensitivity and specificity of TLUSG in diagnosing VCP were 93.3%, 97.8% respectively. Taking these values as reference, the minimum required sample size with desired precision of 15%, power of study as 80% and, level of significance of 5% is 32 patients. To reduce the margin of error, the total sample size taken was 40.
The data was analyzed for statistical analysis utilizing Microsoft Excel office 2010 SPSS IBM version 22, IBM SPSS statistics base (SPSS South Asia PVT, Ltd, Bengaluru, India).
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Sensitivity, specificity, Negative Predictive Value and Positive Predictive Value were assessed. Inter-rater kappa agreement was used to find out the strength of agreement between TLUSG and direct laryngoscopy. Chi- square test/Fisher’s exact test was used to compare pre and post-finding of Vocal Cord (VC) function. A p-value of less than 0.05 will be considered as significant.
In this prospective observational study 60 consecutive patients were screened to enroll in the study out of which 40 were selected. The technique of anesthesia and induction used in the study was same for all the subjects of the study to keep the variations in the observations minimal there was not difference in the postoperative care during the time frame of the study.
No patient had vocal cord palsy pre-operatively because everyone was screened for it with the indirect laryngoscopy before being included in the study. The preoperative indirect laryngoscopy was done similarly in all the patients in our study by ENT department. The accessibility of indirect laryngoscopy was 100 % in our study and the patients had bilateral symmetrical vocal cords. Preoperative USG could assess 39(97.5%) of the study population. The assessment in the immediate postoperative period and at discharge was 38 (95%) and 40 (100 %) respectively. The assessment of the vocal cords in one patient 1 (2.5%) was not possible. The direct laryngoscopy done at the extubation could assess 37 (92.5%) of the population but provided partial visibility in 26 (63%), with poor patient comfort in 32 (80%) as graded by the Direct visualization score and patient reactivity score On comparing hemodynamic parameters among a significant variation from the baseline was seen during direct laryngoscopy when compared to TLUSG. This data shows that the use of direct laryngoscopy to assess the vocal cord function resulted in significant stress to the patient population as observed with vital signs. At the discharge the patients underwent indirect laryngoscopy which was done to assess if there was any improvement in the function of vocal cords during discharge.. The sensitivity, specificity, positive predictive value, and negative predictive value of TLUSG were 97.42%, 66%, 94.7%, 97% in the immediate postoperative period, and 97.2%, 100%, 100%, 50% at discharge (Tables 1-3).
| Demographic profile of patients in the study | |
|---|---|
| Age (years) | 42.02 ± 15.1 |
| Male:female | 10:30 |
| Height(cms) | 157 ± 18.3 |
| Weight(kg) | 62.9 ± 14.8 |
| BMI (kg/sq.m) | 25.9 ± 7.8 |
Table1: Demographic details of participants in study.
| Comparison of TLUSG | TLUSG | Total | ||
|---|---|---|---|---|
| Grade I | Grade II and III | |||
| Direct | Grade I | 34 (TP) | 1 (FP) | 35 |
| laryngoscopy | Grade II and III | 1 (FN) | 2 (TN) | 3 |
| Total | 35 | 3 | 38 | |
Note: TLUSG=Transcutaneous Laryngeal Ultrasonography Grade I-full or normal symmetrical movement in ≥ 1 vocal cords, Grade II-impaired or reduced movement in ≥1 vocal cords, Grade III-no movement in ≥ 1 vocal cord. Patients were then taken to the operating room.
Table 2: Comparison of TLUSG with direct laryngoscopy for vocal cord assessment in the immediate postoperative period.
| Comparison of vocal cords | TLUSG | Total | ||
|---|---|---|---|---|
| Normal vocal cords | Vocal cord palsy or | |||
| Impairment | ||||
| Laryngoscopy | Normal vocal | 36 (TP) | 0 (FP) | 36 |
| Cords | ||||
| Indirect Laryngoscopy | Vocal cord palsy or | 1(FN) | 1(TN) | 2 |
| Impairment | ||||
| Total | 37 | 1 | 38 | |
Note: TP: True Positive, FP: False Positive, FN: False Negative, TN: True Negative.
Table 3: Comparison of assessment of vocal cords by indirect laryngoscopy and TLUSG at discharge.
Though deemed a safe surgery it has a multitude of postoperative complications of which vocal cord palsy is the most dreaded one. During the surgery close proximity of RLN to the thyroid gland and anatomical variations creates the possibility of damage. Vocal cord motility is managed by intrinsic laryngeal muscles, which are all supplied by the recurrent laryngeal nerve paralysis of this nerve leads to unilateral or bilateral paralysis of the vocal cords leading to stridor, respiratory distress, voice and phonation abnormalities in the patients which pose issues postoperatively. Preoperative palsy should be diagnosed to safeguard oneself from medicolegal litigation and helps the surgical team along with anaesthesiologist to plan and be prepared for the unwanted consequences. To address these situations a diagnostic modality to assess the movement of vocal cords perioperatively is essential. Several international guidelines for the thyroid surgeries like the American thyroid association, and the Association of endocrine surgeons, advocate testing the recurrent laryngeal nerve function by assessing the vocal cord function pre and post-operatively to prevent complications and for a successful surgery.
TLUSG is minimally invasive and produces little disturbance in normal voice production, does not cause any trauma to airway structures and so can be used as a diagnostic tool of assessing the vocal cord mobility.
In our study USG was used to evaluate the vocal cords in the peri-operative setting because it is a novel diagnostic tool in this area and has shown better patient compliance in other fields of medicine. Major imaging modalities that can be used to assess the vocal cords like CT scan and MRI are not only cumbersome in view of a postsurgical patients’ logistics but also cause unnecessary radiation exposure and adds up to the cost of hospital stay Standard modalities like laryngoscopy, laryngoendoscopy can provide exact status of vocal cords but have disadvantages like poor patient compliance, invasive, costly and lesser scope for repeatability.
In accordance to an observation by Nanda et al. [8] in our research too; the majority of participants were younger than the age of fifty years (80%) this may be due to the high incidence of goiter in the younger generation.
The sensitivity of the indirect laryngoscopy as reported by Yeung et al. is 77.7% [9].This is commonly done in the outpatient department by an experienced oto-laryngeal surgeon. The dilemma of whether to perform a indirect laryngoscopy exists among endocrine surgeons but both modalities serve different purpose [10]. The indirect laryngoscopy not only assesses the vocal cord mobility but helps in identifying other vocal cord disorders by providing the real image of the vocal cords.
Compared to indirect laryngoscopy the preoperative TLUSG could assess only 39 (97.5%) patients. The inaccessibility of one patient was majorly attributed to the large size of the goiter that was presented with extra thyroidal extension. The accessibility of TLUSG in the preoperative period ranged from 50%-100% as per the analysis of various studies. When compared to the preoperative indirect laryngoscopy to the preoperative TLUSG chance of palsy still being present when it is not identified by the TLUSG (negative predictive value) was 24 (60%) [11].
In our study direct laryngoscopy was performed at the extubation after reversal of neuromuscular blockade. The sensitivity and specificity of the direct laryngoscopy is reported to be 55% and 88% [6,12]. As per study Kundra et al. [6] direct laryngoscopy was done on all 40 patients in our study with Macintosh laryngoscope there were 3 vocal cord palsies. All palsies were identified to be grade II in 1(2.5%) subject, while 1(2.5%) was not identified and 1(2.5%) which was graded as grade II by direct laryngoscopy was graded as III with TLUSG. Direct laryngoscopy provided a partial view of the glottis in more than half (60%)of the patient’s leading to the hampering of the diagnosis of the vocal cords along with discomfort to the patient jeopardizing the quality of anaesthesia.
The presence of adverse hemodynamic response to direct laryngoscopy was clearly evident in the results when the vital parameters were compared between the TLUSG and laryngoscopy there was a significant (p<0.05) change in the vital parameters while performing Direct laryngoscopy.
In our study, the sensitivity and specificity of TLUSG immediately after surgery were 94.72 % and 66% respectively whereas when used at the discharge it was 97.2% and 100% respectively. Similar to recent studies, this prospective study also found a high success rate in visualizing and assessing the vocal cords with TLUSG [13-16].In our study compared to direct laryngoscopy TLUSG could detect 2 (5%) grade II palsy out of which one was detected by direct laryngoscopy as well. And 1(2.5%)) grade III palsy which was identified as grade II palsy by direct laryngoscope. The discrepancy in grading of this palsy could be as a result of poor visualization with direct laryngoscopy. When TLUSG in the immediate intraoperative period was compared to TLUSG at discharge among 3 patients that had vocal cord palsy in the immediate postoperative period 2 (5%) had confirmed palsy at discharge as assessed by TLUSG and one had the return of normal function. Indirect laryngoscopy could not assess all the patients at discharge, there were a total of 2 (5%) patients whose vocal cords could not be assessed due to excessive gag reflex and lack of cooperation and preoperative findings could not be confirmed. Here TLUSG proved to be efficient in analyzing these vocal cords, none of the 2(5%) in assessable vocal cords with indirect laryngoscopy showed any palsy with TLUSG.
Despite providing better sensitivity and specificity in TLUSG as the diagnostic tool in assessing the vocal cord function postoperatively. The assessability of TLUSG in detecting the vocal cords in the first place remains questionable. In our study, the TLUSG failed in assessing 2 (5%) of vocal cords in the patients that were examined in the immediate postoperative period. In the TLUSG done during the postoperative period at discharge, all the vocal cords were assessable. The assessability rates in our study were 95% preoperatively and 97.5% postoperatively. The TLUSG done on the day of discharge was 100 %. The subjects whose cords were not assessable during the postoperative period were both young males whose BMI was in the overweight and obese category. Previous studies have identified the presence of calcifies thyroid cartilage or the elderly and male gender as risk factors similarly in our study the patients whose vocal cords were not assessable were both males in middle age [17,18]. The use of other methods to improve the visualization like lateral approach, use of gel pad, transducer of different frequency was not done in the study. Kandil et al. have reported that the vocal cord visualization is affected by rise in body mass index [8]. In accordance both the patients in whom vocal cords could not be appreciated were BMI>30 kg/m².
Apart from this the TLUSG also proves to be a valuable tool in providing safe anaesthesia while assessing the vocal cords immediately after surgery by providing better patient satisfaction and safety and avoiding complications like a spasm in the patients postoperatively. TLUSG is a promising modality to test the presence of vocal cord paresis or palsy. By following appropriate steps, the visualization of vocal cords can be achieved. The sensitivity and specificity of TLUSG are portrayed to be better than direct laryngoscopy. The TLUSG stood as a better tool in assessing the vocal cord function in both the immediate postoperative period with a sensitivity of and specificity of 97% and 66% and also in reconfirming the vocal cord function at the time of patient discharge from the hospital with a sensitivity of 97% and a specificity of 100% though there is an unassessability rate in the preoperative period of 2.5 % and 7.5% in the immediate postoperative period TLUSG did not miss even a single subject with the palsy in contrast to direct laryngoscopy (which could not detect a palsy that was identified in the immediate postoperative period), providing zero false negatives in the sample which makes it more specific tool than direct laryngoscopy.
Quantitative measurements like the length of vocal cords, vocal fold displacement velocity, and measuring the thickness of vocal cords after the surgery, use of doppler mode imaging to assess the vocal cords was not done in study leading to purely qualitative measurement of the vocal cords motility rather than providing quantitative indicators.
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed].
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Sri S, Harish S, Jindal P, Singh S (2023) Comparing the Efficacy of Transcutaneous Laryngeal Ultrasonography and Direct Laryngoscopy in Assessing the Function of Vocal Cords in Postoperatively in Thyroidectomy Patients. J Anesth Clin Res. 14.1104.
Received: 14-Mar-2023, Manuscript No. JACR-23-22144; Editor assigned: 17-Mar-2023, Pre QC No. JACR-23-22144 (PQ); Reviewed: 31-Mar-2023, QC No. JACR-23-22144; Revised: 07-Apr-2023, Manuscript No. JACR-23-22144 (R); Published: 14-Apr-2023 , DOI: 10.35248/2155-6148.23.14.1104
Copyright: © 2023 Sri S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.