
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research - (2022)Volume 13, Issue 4
Background: In the era of rapid extubation following cardiac surgery, providing adequate analgesia in perioperative period is utmost important. The aim of the study is to evaluate the effect of low dose Intra Thecal Morphine (ITM) on postoperative analgesia, pulmonary function and postoperative recovery profile.
Methods: Seventy-two patients were randomized to either ITM (n=34) or Intra Venous Morphine (IVM) (n=34) groups. Patients in the ITM group received 350 μg intrathecal morphine followed by general anaesthesia, and IVM group received only general anaesthesia. Comparisons were made between the groups with respect to quality of analgesia and Pulmonary Function (PF) in postoperative period.
Results: In the ITM group, the total consumption of morphine during the first 24 hour was significantly reduced; patients reported less pain scores, and less mechanical ventilation duration. Both groups reported significantly reduced Forced Expiratory Volume in 1 second (FEV1) and Forced Vital Capacity (FVC) post-operatively, however no significant decreases observed between groups.
Conclusion: A single dose ITM administration is safe and more effectively reduces postoperative pain and mechanical ventilation duration in patients undergoing on pump cardiac surgery. However, ITM administration did not significantly affects the pulmonary function compared to IVM in post-operative period.
Intrathecal morphine; Pulmonary function; Cardiac surgery
In cardiac surgery, pain following sternotomy is often severe and is aggravated by deep breathing, coughing and mobilization [1]. Severe pain leads to post-operative pulmonary complications which prevent the patient to take deep breath and the cough which leads to pooling of secretions and alveolar atelectasis [2].
Currently, multimodal strategies for pain control is commonly practiced in post cardiac surgery patients which are mainly based on systemic opioids, combined with non-steroidal anti-inflammatory drugs and paracetamol [3]. Previous studies have demonstrated that intrathecal and epidural anesthesia decreases stress response to surgery, and it has positive effects on analgesia and respiratory functions after cardiac surgery [4]. However, during cardiac surgery the requirement of heparin is very high to achieve target level of Activated Clotting Time (ACT), epidural analgesia can lead to epidural hematoma formation. Intrathecal opioid administration is associated with a reduced risk of epidural haematoma [5]. Adequate analgesia is now possible with the intrathecal administration of a minimal dose of morphine and is associated with minimal systemic adverse effects [6]. Small dose of intrathecal opioids provides adequate analgesia and decreases the adverse effects associated with systemic administration of opioids [7]. However, the impact of ITM on pulmonary function recovery after cardiac surgery has been not much studied so far.
The aim of this study was to evaluate the effects of low dose ITM on morphine consumption, analgesia, pulmonary function and recovery profile following cardiac surgery.
After approval from institute ethics committee and written informed consent, patients between 18 to 75 years of age who were scheduled for elective Coronary Artery Bypass Graft (CABG) surgery or valve surgery under Cardio Pulmonary Bypass (CPB) participated in the study. Patients with abnormal coagulation test, platelet count of less than 1 lacs, any neurological complications (like stroke, delirium), Intra-Aortic Balloon Pump (IABP) after surgery, who could not perform baseline Pulmonary Function Test (PFT), sternum infections or instability and patients with history of previous cardiac surgery were excluded. Blinding the patients was not possible as this would require administration of an intrathecal placebo which has been not approved by ethical committee.
Anesthesia protocol
Pre-operative assessment was done one day prior to surgery in ward as well as baseline PFT was performed. On the day of surgery, patients were assigned to one of two groups according to a computer-generated table of random numbers.
ITM Group: Received intrathecal morphine and general anesthesia.
IVM Group: Received general anesthesia.
In operating room standard monitoring were attached, and left radial artery secured for invasive pressure monitoring and right internal jugular vein were cannulated for central venous pressure measurement and volume administration prior to the induction of anesthesia. Before induction of anesthesia, in the ITM group, lumbar puncture was performed at the L3-4 or L4-5 interspace with a 25-gauge Quincke-tipped spinal needle (Sprotte Standard Needle, Pajunk, Germany) in right lateral position. In the IVM group, lumbar puncture was not performed. Same anesthesiologist performed all lumbar punctures, more than two attempts were not allowed. After obtaining clear Cerebro Spinal Fluid (CSF), 350 μg morphine diluted in 8 mL of sodium chloride were injected into the intrathecal space. Following which all patients were placed into the supine position and general anesthesia was induced using propofol 2 mg/kg, fentanyl 2-4 μg/kg, vecuronium 0.1 mg/kg to facilitate intubation and maintained by isoflurane, fentanyl 1 μg/ kg/h and vecuronium 0.02 mg/kg/h. After achieving ACT of >480 seconds, CPB was started. Surgery was performed under mild hypothermia (34°C to 36°C). Myocardial protection was provided by using intermittent anterograde cold blood cardioplegia.
Postoperative management
After completion of surgery patients were shifted to surgical Intensive Care Unit (ICU). In postoperative period, both groups received infusion of propofol 0.5 to 1 mg/kg/hr, until normothermia and hemodynamic stability were attained. For analgesia, injection paracetamol 1 gm was given three times a day in both groups. In IVM group, patients received 20 μg/kg/h morphine infusion during the first 24 hours of ICU stay. After patient became awake and alert, on duty anesthesiologist assessed pain every 4 hours using the Visual Analog Scale (VAS). One day prior to surgery, patients were instructed on how to use the VAS. When VAS was equal or more than 4 in either group, morphine 50 μg/kg was given Intra Venous (IV) as first rescue analgesic. Total dose of intravenous morphine was recorded in first 24 h and 48 h in both groups. The criteria for extubation, patients need to be awake, oriented and stable hemodynamics with minimal inotropic support.
The PFT was performed bedside by a respiratory physiotherapist using clarity spirotech (CMSP-01 model by Clarity Medical) computer-based diagnostic spirometer. Measurements were performed in the sitting position. Three measurements were obtained and the highest value of three technically satisfactory maneuvers was retained for FVC and FEV1 [8]. Postoperative PFT assessments was done on 3, 5 and 7 postoperative day.
Statistical analysis
Analysis was conducted using IBM SPSS STATISTICS (version 22.0). Categorical variables were reported as counts and percentages. Group comparisons were made with the Chi-Square test or Fisher's exact test, as found appropriate. The normality of quantitative data was checked by measures of Kolmogorov Smirnov tests of normality. Continuous data was given as mean ± SD and range as median and interquartile range. As appropriate for non- normally distributed (skewed) data, comparisons were made by Mann-Whitney test for normally distributed data and Student t-test was applied to compare two groups. Change for lung functions were calculated by subtracting the value of each subject T1-T0 i.e., time 1-time 0, percentage changes then its mean/medians were calculated. Mann-Whitney U test was carried to compare 2 groups. P value<0.05 was considered significant.
Considering the previous studies, 40% reduction in morphine consumption following cardiac surgery was reported in the ITM group [9]. At least 25 patients should be calculated to provide appropriate statistical power with α error of 5% and β error of 10%. To detect an expected 40% reduction in morphine consumption following cardiac surgery in the ITM group, 34 patients were enrolled in each group to provide appropriate statistical power analyses.
Over the period of 6 months, we enrolled 72 patients, 4 patients were excluded because of postoperative complications, and 34 patients were enrolled in each group (Figure 1). The baseline and intraoperative characteristics were similar between the groups. There was no statistically significant difference between the two groups in terms of age, sex, weight, preoperative FEV1, pre- operative FVC, aortic cross clamp time, CPB time and duration of surgery (Table 1).
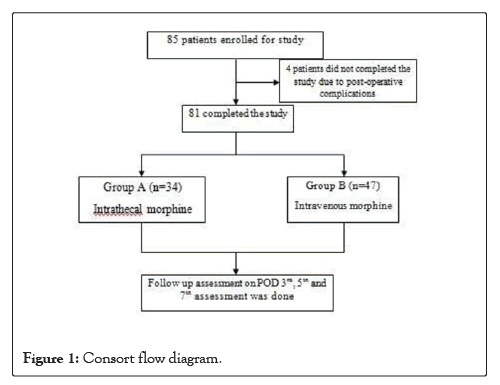
Figure 1: Consort flow diagram.
| Variables | Group A (n=34) | Group B (n=47) | p-value |
|---|---|---|---|
| Male/Female n (% within gender) | 18/16 (52.9/47.1) | 25/22 (53.2/46.8) | 0.983 |
| Age (Years) | 49.38 ± 15.36 | 42.89 ± 14.97 | 0.093 |
| BSA(m2) | 1.72 ± 0.21 | 1.58 ± 0.20 | 0.008 |
| Pre-operative FEVI (ltr) | 1.9 ± 0.80 | 2.03 ± 0.71 | 0.085 |
| Pre-operative FVC (ltr) | 1.98 ± 0.98 | 2.23 ± 0.83 | 0.197 |
| Pre-operative exercises n (%) | 18 (75) | 42 (89.4) | 0.165 |
| AXC time (mins) | 119.12 ± 63.9 | 102.34 ± 49.32 | 0.138 |
| CPB time (mins) | 151.58 ± 70.1 | 144.06 ± 99.51 | 0.277 |
| Duration of Surgery (mins) | 305 ± 92.79 | 282.98 ± 101.53 | 0.384 |
| Duration of Anesthesia (mins) | 358.22 ± 98.84 | 336.62 ± 113.74 | 0.242 |
| Valve surgery/CABG | 21/13 | 31/16 | 0.097 |
Table 1: Baseline and intra-operative characteristics of the patients. Note: BSA: Body Surface Area; CPB: Cardio Pulmonary Bypass; AXC: Aortic Cross Clamp; ICU: Intensive Care Unit; VIS Score: Vasoactive-Ionotropic Score; FEV1: Forced Expiratory Volume in one Second; FVC: Forced Vital Capacity; CABG: Coronary Artery Bypass Graft. P-value <0.05 is significant.
Patients in ITM group scored less pain on VAS compared to IVM group at 24 hours and 48 hours (p=0.001 and p=0.03 respectively) following cardiac surgery. Also, ITM group has low morphine consumption compared to IVM group at 24 hours and 48 hours after surgery (p<0.05). Recovery profile including mechanical ventilation duration was significantly reduced in the ITM group (10.13 ± 9.59 h vs. 15.42 ± 10.68 h); however, the lengths of ICU and hospital stay were comparable between the groups. Postoperative complications are listed in Table 2. The incidence of postoperative complications were comparable between the groups (p>0.05).
| Percentage change | Group A | Group B | p-Value |
|---|---|---|---|
| Preoperative FVC-POD 3 FVC (Percentage change) | 38.37 ± 28.62 | 43.08 ± 28.22 | 0.385 |
| Preoperative FVC-POD 5 FVC (Percentage change) | 31.7 ± 23.89 | 27.54 ± 43.4 | 0.86 |
| Preoperative FVC-POD 7 FVC (Percentage change) | 22.5 ± 27.24 | 17.18 ± 46.08 | 0.799 |
Table 2: ICU and post-operative characteristics in both groups. Note: FEV1: Forced Expiratory Volume in one Second; POD: Post-Operative Day. P-value <0.05 is significant.
Preoperative lung volumes were within predictive values in both groups, whereas postoperative percentage change in FEV1 at POD3, POD5 and POD7 were significantly reduced in both groups compared to preoperative values (37.10 ± 25.61 vs. 43.05 ± 28.52, 29.38 ± 23.78 vs. 28.35 ± 41.10 and 16.97 ± 29.30 vs. 15.45 ± 38.01 respectively), but the percentage change in lung volume were comparable between the groups (p>0.05) (Table 3). Similarly, percentage change in FVC at POD3, POD5 and POD7 were significantly decreased in both groups compared to preoperative values (38.37 ± 28.62 vs. 43.08 ± 28.22, 31.70 ± 23.89 vs. 27.54 ± 43.40 and ± 22.50 ± 27 ± 24 vs. 17.18 ± 46.08 respectively), although percentage change in volume were comparable between the groups (p>0.05) (Table 4). Reduction in lung volume was highest on day 3 and over the time patient’s pulmonary function gradually improved.
| Percentage change | Group A | Group B | p-Value |
|---|---|---|---|
| Preoperative FVC-POD 3 FVC (Percentage change) | 38.37 ± 28.62 | 43.08 ± 28.22 | 0.385 |
| Preoperative FVC-POD 5 FVC (Percentage change) | 31.7 ± 23.89 | 27.54 ± 43.4 | 0.86 |
| Preoperative FVC-POD 7 FVC (Percentage change) | 22.5 ± 27.24 | 17.18 ± 46.08 | 0.799 |
Table 3: Percentage changes in FVC in both groups. Note: FVC: Forced Vital Capacity; POD: Post-Operative Day. P-value <0.05 is significant.
| Post-operative characteristics | Group A (n=34) | Group B (47) | p-value |
| VAS at 24 hours (0-10) | 3.12 ± 1.40 | 6.23 ± 2.12 | 0.001 |
| VAS at 48 hours (0-10) | 2.21 ± 0.91 | 4.32 ± 1.92 | 0.03 |
| ICU Stay (days) | 6.21 ± 1.22 | 6.04 ± 1.59 | 0.232 |
| Morphine consumption 0 to24 h (mg) | 4.64 ± 3.63 | 32.33 ± 15.82 | 0.001 |
| Morphine consumption 24 to 48 h (mg) | 7.11 ± 5.45 | 12.21 ± 4.22 | 0.045 |
| VIS | 6.58 ± 5.23 | 7.84 ± 7.32 | 0.643 |
| Mechanical ventilation duration h | 15.13 ± 11.59 | 22.42 ± 10.68 | 0.04 |
| Pneumonia | 2 (5.90%) | 3 (6.4%) | 0.505 |
| Pneumothorax | 3(8.8%) | 4 (8.5%) | 0.61 |
| Stroke | 1 (2.94%) | 0 | 0.542 |
| Vomiting | 6 (17.64%) | 7 (14.89%) | 0.652 |
| Mortality | 1 (2.94%) | 2 (5.90%) | 0.943 |
Table 4: ICU and post-operative characteristics in both groups. Note: VAS: Visual Analogue Scale; ICU: Intensive Care Unit. P-value<0.05 is significant.
In the present study, the author demonstrated that single dose ITM (350 ug) administration provides good analgesia and significantly reduces the morphine consumption during first 24 hours following cardiac surgery. This analgesic effect is associated with a significant reduction of mechanical ventilation duration in postoperative period. However, inspite of better pain control, no significant improvements in PF were observed.
Inadequate pain control in the postoperative period may result in hemodynamic alterations and increased incidence of pulmonary complications which further leads to increased morbidity, postoperative hospital length of stay and thus cost. Opioids are the primary analgesic used following cardiac surgery. However, opioids are associated with numerous adverse effects including nausea, vomiting, pruritus, constipation and urinary retention. The potential benefits of ITM involve stress response attenuation, intense postoperative analgesia, and thoracic cardiac sympathectomy. In this study, author observed that pain score and opioid consumption was significantly less during first 24 h following cardiac surgery. Roediger et al., [9] in their study administered 500 ug morphine intrathecally, and the author demonstrated that following cardiac surgery the requirement of total intravenous morphine was significantly reduced by 40% and patients encountered lower pain scores during the first 24 hours. Similar finding was demonstrated by Mukherjee et al. in their study they found that intrathecal morphine is enough to provide pain control in patients undergoing minimally invasive cardiac surgery [10]. A recent study by Elgendy et al. showed that the total opioid consumption during the first 24 hours after extubation was significantly reduced by 35% in the ITM group as compared to the control group [11]. In our study we have demonstrated 15% reduction in cumulative morphine consumption in ITM group during first 24 hours after cardiac surgery.
Respiratory system dysfunction is one of the most common complications which encountered in patients undergoing cardiac surgery on CPB. Deep breathing exercises have been shown effective in reducing atelectatic areas and improving pulmonary function in patients undergoing CABG surgery [12]. Impaired coughing, shallow breathing, immobility and bed rest may lead to atelectasis and reduced clearance of pulmonary secretions increasing the risk of atelectasis, pneumonia and respiratory insufficiency [13]. Parenteral opioids itself is associated with dose-dependent adverse drug events including respiratory depression, dizziness/cognitive dysfunction, nausea/vomiting, constipation, and pruritus [14]. Older and sicker patients are at greater risk for opioid related adverse events.
Central neuraxial analgesia with thoracic epidural techniques has been associated with a reduction in the incidence of PPC’s after CABG surgery [15]. However, high levels of blood anticoagulation is mandatory in on pump cardiac surgery, thoracic epidural techniques increase the risk of hematoma formation [16]. Therefore, ITM is quite simple, it has high success rate and safe technique for perioperative pain management in cardiac surgery.
In the present study, inspite of better pain control in postoperative period, no improvement in pulmonary function was observed. Our findings were correlating with study performed by Santos et al. they found a similar decline of the FVC and FEV in patients with ITMA and IVA groups [17]. Similar findings were also observed in two meta-analysis used to evaluate the use of intrathecal morphine in cardiac surgery did not reveal a correlation between the efficacy of pain control and better respiratory outcome [18,19]. Intrathecal morphine was associated with a shorter duration of postoperative mechanical ventilation in our study. Similar finding was also observed by Shroff et al. found a shorter extubation time when using of intrathecal morphine [20].
This study has some limitations. The sample size was small. The patient’s long term follow up was not done. So, assessing long term pulmonary function and complications with a bigger sample size is recommended in the future.
The study demonstrated that single dose ITM administration is safe and very effective for postoperative analgesia following cardiac surgery. It also reduces the extubation time. However, ITM administration did not significantly affects the pulmonary function compared to IVM in early postoperative period.
[Google Scholar][PubMed].
[Google scholar][PubMed].
Citation: Negi SL, Kumar S, Katiyar N, Negi S, Thingnam S, Niyogi SG, Gourav KP (2022) Comparative Evaluation of Intrathecal Morphine vs. Intravenous Morphine on Post-operative Pain and Pulmonary Function in Patients Undergoing On-pump Cardiac Surgery: A Prospective Randomized Study. J Anesth Clin Res. 13:1058.
Received: 13-Apr-2022, Manuscript No. JACR-22-16938; Editor assigned: 15-Apr-2022, Pre QC No. JACR-22-16938 (PQ) ; Reviewed: 25-Apr-2022, QC No. JACR-22-16938; Revised: 05-May-2022, Manuscript No. JACR-22-16938 (R); Published: 13-May-2022 , DOI: 10.35248/2155-6148.22.13.1058
Copyright: © 2022 Negi SL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.