Journal of Sleep Disorders & Therapy
Open Access
ISSN: 2167-0277
ISSN: 2167-0277
Research Article - (2023)Volume 12, Issue 10
Background: Cognitive Behavioural Therapy for Insomnia (CBT-I) is the first line treatment of insomnia. However, there is limited research in the Arab countries that has assessed its efficacy with Arabic speakers, particularly in targeting sleep habits, behaviours, and thoughts related to Arab culture. The aim of this work is to review the empirical studies that assessed the effectiveness of CBT-I in Arab countries and address the research and clinical practice limitations.
Methods: A systematic review was conducted following the PRISMA guidelines. The Ovid interface was utilized to search the Midline and PsycINFO databases from January to the end of March 2023. Google Scholar was further used for retrieval of other relevant searches. Appropriate search terms were used to gather studies that examined the efficacy of CBT-I in Arabic countries. The Quality Criteria Checklist (QCC) was utilized to examine quality.
Results: Seven eligible studies were identified, four in Egypt, two in Lebanon, and one in Saudi Arabia. All studies utilized the pre-post assessment design and included several assessment tools to assess the severity of insomnia, comorbidity and the effect of CBT-I. CBT-I in the studies consisted of, sleep hygiene and education, Stimulus Control therapy (SC), Sleep Restriction Therapy (SRT), cognitive therapy, and relaxation training. All studies have assessed the effectiveness of CBT-I in treating patients with insomnia. All studies were rated as positive according to the QCC.
Conclusion: This review has found that CBT-I was an effective treatment for treating insomnia and reducing the severity of insomnia symptoms.
Insomnia; Cognitive Behavioural Therapy for Insomnia (CBT-I); Arab; Insomnia
The International Classification of Sleep Disorders (ICSD-3) has identified insomnia as a sleep disorder with three main criteria: Difficulty initiating sleep, difficulty maintaining sleep, and waking up earlier than desired. In addition, daytime symptoms such as mood disturbance, irritability, fatigue, daytime sleepiness, memory and attention impairment, excessive concern about sleep, and energy reduction may also be present. These symptoms must persist for at least three months and at least three times per week with a significant impact on an individual’s daily functioning [1]. Insomnia complications include work absenteeism, social withdrawal, and driving accidents [2]. Additionally, severe insomnia can lead to mood disturbances, psychological effects, and physical problems [3].
Cognitive Behavioural Therapy for Insomnia (CBT-I) is considered the first line treatment for insomnia. However, there are limited studies on CBT-I in Arab countries due to the small number of specialists trained in CBT-I in clinical practice. Additionally, there is a need to adapt CBT-I to different cultures, taking into consideration different day and night sleep routines. For instance, in Muslim cultures, people may wake up to pray around 3 am and eat late at night due to fasting during and beyond the holy month of Ramadan. Hence, sleep patterns may be disrupted, potentially leading to insomnia. Therefore, it is necessary to consider cultural factors and accordingly adapt CBT-I effectively to address insomnia in these diverse cultural and populations contexts. The aim of this work is to review the studies that assessed the effectiveness of CBT-I in Arab countries and address the research gaps and clinical practice limitations in the Arab world.
This systematic review was conducted following the guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [4].
Search strategy
The Ovid Interface was utilized to search the electronic databases Medline and PsycINFO during the period from January 2023 to the end of March 2023. Preliminary research was conducted using Google Scholar to add other relevant data to the search. Google Scholar’s initial search was limited to studies on CBT-I in Arab countries from 2000 to 2023. The following search terms were used for the search: “Cognitive Behavioural Therapy”, “Cognitive behaviour therapy”, “Cognitive behavioural therapies”, or “CBT” and, “Insomnia”, “Sleep”, or “Sleep Quality”. The search was conducted using both free text and subject headings when applicable. Then search terms appropriate to the Arab countries were added to the search to limit the results to valid studies, such as “Arab Country,”, Arab Countries”, Arabic Speaking countries”, “Egypt”, “Libya”, “Tunis”, “Algeria”, “Morocco”, “Mauritania”, “Sudan”, “Djibouti”, “Somalia”, “Comoros island”, “Yemen”, “Oman”, “United Arab Emirates”, “Qatar”, “Saudi Arabia” or “GULF countries”, “Bahrain”, “Kuwait”, “Syria”, “Lebanon”, “Palestine”, “Jordan”. Synonyms and related terms were used to expand the search range to include all relevant papers. Additionally, a wildcard function “*” was employed to search for multiple suffixes of a single term. To ensure the discovery of any additional relevant literature, the reference lists of the primary articles were screened, but no additional papers were found.
Inclusion and exclusion criteria
Studies were considered eligible for inclusion in this review if they involved participants who met the diagnostic criteria for insomnia, including both primary and secondary insomnia. The diagnosis of insomnia preferably followed the guidelines outlined in the International Classification of Sleep Disorders (ICSD-3). The studies were required to implement CBT-I, utilizing a range of techniques such as sleep hygiene, psychoeducation about sleep and insomnia, sleep restriction techniques, stimulus control, relaxation exercises, and cognitive therapy. The inclusion criteria also specified that the studies should include four to eight psychotherapy sessions, although longer programs with weekly sessions were also acceptable. These therapy sessions were to be conducted either individually with a clinical psychologist trained in CBT-I, in a group therapy format, or via a virtual setting.
Furthermore, the studies were expected to use insomnia scales for clinical diagnosis and measure the effect of CBT-I treatment at least once in pre-and post-assessment. The studies needed to include control groups or make a comparison between pre- and post-treatment. Studies that combined medication for comorbidity disorders with CBT-I were also considered. The selected literature was required to be peer-reviewed, conducted with human participants, and published in English. There were no specific criteria regarding age, gender, or setting for inclusion in this study.
Studies were excluded from this systematic review if they did not employ valid measurements for the diagnosis and treatment of insomnia or if they utilized interventions other than CBT-I. Additionally, studies that focused on applying cognitive behavioural therapy for disorders other than insomnia were excluded. Studies that involved self-guided application and the use of self-help materials were also excluded. Furthermore, studies that solely assessed the impact of sleep hygiene and sleep education, without incorporating additional CBT-I techniques, were excluded from this systematic review. More details on inclusion and exclusion criteria are presented in the form of a PICOS in Table 1.
| Inclusion | Exclusion | |
|---|---|---|
| Sample | Age groups above 18 years old | Children under the age of 18 |
| All genders | Participants not from Arab countries | |
| Participants from the Arab countries | ||
| Treatment | CBT-I consists of sleep restriction stimulus control | Studies include sleep hygiene and |
| relaxation exercises, cognitive therapy, sleep hygiene | Sleep education only without CBT-I. | |
| and education. | ||
| Short-term and long-term program | ||
| In-person, online, and group format | ||
| Comparison | Pre-test compared with post-test. | No comparator |
| Outcomes | Any positive or negative health-based or sleep outcome | No measurement of the effect of |
| Objective health-based or sleep outcome measure | CBT-I on sleep outcomes | |
| Subjective outcomes through quantitative analysis | ||
| Improvement or worsening in insomnia symptoms, | ||
| E28 and sleep parameters | ||
| Study design | RCT | Case-control study |
| Controlled trial | Literature review | |
| Quasi-experimental design | Systematic review | |
| Pilot study |
Table 1: PICOS for inclusion and exclusion criteria
Data extraction and assessment of studies
Eligible studies based on the previously described inclusion and exclusion criteria; they were then subject to analysis in this systematic review. Further data were extracted from each study, including the study design, patients, treatment components, measurements and outcomes, and relevance to the research question. This is represented in Table 2.
| Author | Location | Design | Patients | Assessment tools | Intervention and sitting | Comparison | Outcomes |
|---|---|---|---|---|---|---|---|
Abdelaziz, |
Egypt | Quasi-experimental design | 81 old age patients from 60 age to above | Pittsburgh sleep quality index, epworth sleepiness scale, geriatric anxiety scale and geriatric depression scale, and comorbidities questionnaire. | CBT-I group program for 9 months includes sleep hygiene, stimulus control, sleep restriction and relaxation training | Pre-test vs. post-test | Positive outcomes and improvement in sleep quality have been shown in post-test |
Allah, et al. [5] |
Egypt | Quasi-experimental design | 260 postpartum females | The edinburgh postnatal depression scale, sleep quality scale |
In nine group sessions of CBT-I, all techniques were achieved through videos, power point, discussion and role play | Pre-test vs. Post-test | CBT-I was an effective Treatment in improving sleep quality, daytime symptoms, waking up difficulties, and decreasing postpartum depression |
| Ibrahim, et al. [6] | Egypt | Quasi-experimental design | 75 elderly patients | Structured interview questionnaire, the sleep hygiene awareness and Practice Scale, the Pittsburgh Sleep Quality Index (PSQI) |
8 group sessions of CBT-I include sleep hygiene and education, relaxation training, stimulus control and sleep restriction | Pre-test vs. Post-test | findings showed significant improvements in sleep quality and other sleep parameters |
| Kady, et al. [7] | Egypt | A cross-sectional study with a pre-test and post-test design | 210 elderly persons | Pittsburgh Sleep Quality Index (PSQI) | CBT-I group sessions include sleep hygiene, stimulus control, sleep restriction |
Pre-test vs. Post-test | Results showed that CB-T is an effective and safe treatment for elderly people, and showed significant improvement in sleep quality in post-test |
| Geagea, et al. [8] | Lebanon | A pilot study with pre-post-test design | 19 patients participated in the study; 4 of them didn’t continue follow-up after CBT- |
Insomnia Severity Index (ISI) Dysfunctional Beliefs and Attitudes about Sleep (DBAS) |
4 CBT-I group sessions include sleep hygiene and education, stimulus control, sleep restriction and relaxation training | Pre-test vs. Post-test | CBT-I was effective in treating insomnia for persons who use cannabis regularly |
Amer, et al. [9] |
Lebanon | A pilot study with pre-test and post-test | 20 individuals, 10 of them suffer from insomnia with Inflammatory Bowel Disease (IBD) completed CBT-I sessions and post-assessment. |
Actigraphy, Insomnia Severity Index (ISI), Pittsburgh Sleep Quality Index PSQI, The Sleep Hygiene Awareness and Practice Scale, and sleep diaries |
5 CBT-I sessions delivered individually through Telehealth. | Pre-test vs. Post-test | CBT-I was effective in treating insomnia symptoms, and participants gained knowledge about the relationship between IBD and sleep |
| Salwen-Deremer, et al. [10] | Saudi Arabia | RCT with pre-test post-test |
80 women with menopause and insomnia | Demographic data sleep dairy Pittsburgh Sleep Quality Index, and Insomnia Severity Index |
Six weeks of Internet‐based CBT-I | 1-pretest scores vs. Post-test scores in the CBT-I group 2-CBT-I group scores vs. Control group scores |
Internet- bases CBT-I has a positive effect in improving sleep quality among menopausal women |
Table 2: PICOS of the included studies
Study selection
All studies identified from the Medline and PsycINFO databases were imported into the reference systematic review management software called Rayyan. This is a web tool that has aided us in working on this systematic review by allowing us to efficiently screen studies. The initial database search generated a total of 34 references with 40 additional studies from google scholar. After the removal of duplicate studies using Rayyan’s duplicate detection program, 54 studies were remaining. The titles and abstracts of the 54 remaining studies were first screened through Rayyan for initial assessment of eligibility criteria. Afterwards, 14 studies were retrieved in full text for further analysis of eligibility of the 14 studies, three were excluded as they were not research studies but rather protocols which do not fit within our inclusion criteria. Also, four were excluded as they were studies conducted in countries outside the Arab world. The remaining seven studies were thus deemed eligible for inclusion in this systematic review as they meet all inclusion criteria. The full screening and selection process is represented under the PRISMA diagram for systematic reviews in Figure 1.
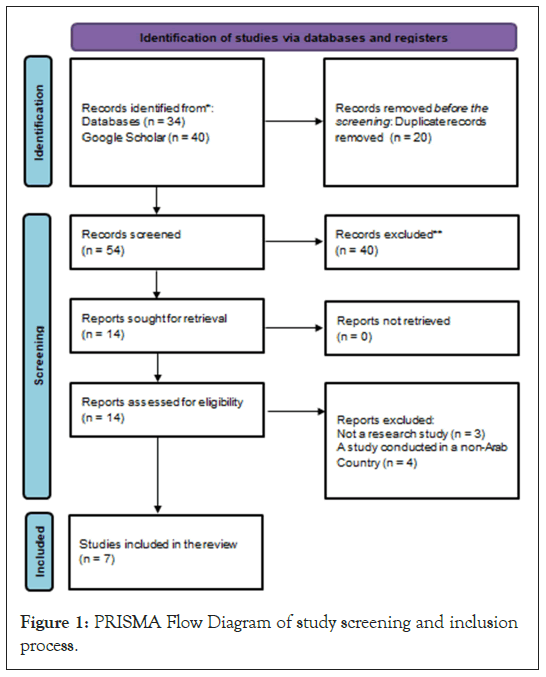
Figure 1: PRISMA Flow Diagram of study screening and inclusion process.
Study characteristics
Table 2 summarises all studies in this review on the efficacy of CBT-I in the Arab world. A total of four studies were conducted in Egypt, two in Lebanon, and one study in Saudi Arabia, and most of them used a quasi-experimental design. Several assessment tools were used for diagnosis and to evaluate the effect of CBT-I in the post-assessment. CBT-I in these studies included sleep hygiene education, stimulus control, sleep restriction, cognitive therapy, and relaxation training. The results suggest that CBT-I has a significant effect in treating patients with insomnia in the Arab world. Significant improvements were observed in sleep quality and quantity, and a decline in insomnia symptoms and comorbid symptoms in different populations, including old age patients, women with postpartum depression, women with menopause, and patients with Inflammatory Bowel Disease (IBD).
Three of the included studies focused on older adults with a total of 370 patients [5-8]. Two studies were limited to female participants only, with one study focusing on menopausal women (n=80), and the other study involving 260 women with postpartum depression [1,9]. One study evaluated the effect of CBT-I in individuals with insomnia related to Inflammatory Bowel Disease (IBD) [10].
Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI) are both well-established and validated assessment tools used to assess sleep quality and insomnia severity, respectively. Other measures that were used in the reviewed studies to evaluate different aspects of sleep quality and habits include the Sleep Quality Scale (SQS) and the sleep hygiene awareness and practice scale. The Dysfunctional Beliefs and Attitudes about Sleep (DBAS) scale is another tool that was used to assess negative beliefs and unrealistic expectations related to sleep, which can contribute to developing and maintaining insomnia.
All of the studies in this review used assessment tools to evaluate insomnia and assess the effectiveness of CBT-I. Pittsburgh sleep quality index was utilized in five studies to evaluate insomnia, while two studies utilized the Insomnia severity index. Sleep Quality Scale (SQS) was used in one study, the sleep hygiene awareness and practice scale was used in one study, and the Dysfunctional Beliefs and Attitudes about Sleep (DBAS) was used in one study to evaluate dysfunctional thoughts related to insomnia and sleep. In addition to these measurement tools, most studies utilized sleep diaries in pre and post-test, and throughout treatment to assess the effect of CBT-I, as well as to monitor improving sleep quality and quantity.
In addition to evaluating clinical insomnia disorder, the main objective of all studies was to examine the efficacy of CBT-I. The CBT-I program involves various techniques, such as sleep hygiene and education, Stimulus Control Therapy (SCT), Sleep Restriction Therapy (SRT), and relaxation exercises. Four studies utilized CBT-I in a group format, while one study conducted CBT-I via the Internet, another through telehealth, and one study conducted the program in an individual setting.
Quality assessment
The overall quality of the seven studies was assessed using the Academy of Nutrition and Dietetics’ quality rating checklist, and it was determined to be positive (Table 3).
| Author | Validity items | Quality rating | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
Abdelaziz, et al. [1] |
+ | + | + | + | - | + | + | + | - | + | Positive |
Allah, et al. [5] |
+ | + | + | + | - | + | + | + | + | + | Positive |
| Moukhtar Ibrahim, et al. [6] | + | + | + | + | - | + | + | + | - | + | Positive |
| Kady, et al. [7] | + | + | + | - | - | + | + | + | + | + | Positive |
| Geagea, et al. [8] | + | + | + | + | - | + | + | + | + | + | Positive |
Mostafa Amer, et al. [9] |
+ | + | + | + | - | + | + | + | + | + | Positive |
| Salwen-Dermer, et al. [10] | + | + | + | + | - | + | + | + | + | + | Positive |
Note: Studies were rated on 10 items: 1=statement of the research question, 2=subject selection free from bias, 3=comparable study groups, 4=method for withdrawals described 5=blinding used, 6=interventions describe, 7=outcomes stated and measurements valid and reliable, 8=appropriate statistical analysis, 9=appropriate conclusions and limitations described and 10=funding and sponsorship free from bias. A positive rating of items 2, 3, 6, and 7 must be satisfied for an overall positive quality rating. +,= item present. -,=item not present. Na=not applicable. u=unclear.
Table 3: Quality assessment using the quality criteria checklist for primary research of the included studies
All studies scored positive on the first checklist I team indicating that the study has clearly stated the research question with specific intervention(s) or procedure independent variables being identified. All studies also demonstrated a participant selection being free from bias with inclusion/exclusion criteria specified. In addition, all studies have comparable study groups with the method of assigning subjects/patients to groups being clearly described and unbiased.
Most studies described the method of handling withdrawals from the number of participants, however, one did not [7]. Due to the nature of the assessed topic in all studies, none of the studies used blinding to prevent the introduction of bias. Subjects, clinicians/practitioners, and investigators were not blinded to treatment. All seven studies clearly described in detail the intervention, therapeutic regimens/exposure factors, or procedure and any comparisons. Also, all studies clearly defined outcomes and measurements used as being valid and reliable with statistical analysis appropriate for the study design. Out of the seven included studies, five reached conclusions that were supported by their findings with biases and limitations taken into consideration, while two failed to take into consideration limitations [5-6]. Finally, all studies were successful in describing sources of funding and investigators’ affiliations as being free from bias. All included studies were reviewed regardless of their overall quality rating to ensure the provision of generalizable results and suggestions for further research.
This systematic review aims to evaluate the effectiveness of Cognitive Behavioral Therapy for Insomnia (CBT-I) in the Arab world, based on seven empirical studies. The review explores the similarities, differences, and potential implications of implementing CBT-I in diverse cultural and clinical contexts. The growing body of research and clinical practice in CBT-I, coupled with the recommendation from the American Academy of Sleep Medicine that CBT-I is the primary non-pharmacological treatment for insomnia, provides evidence supporting the efficacy of CBT-I for the treatment of insomnia.
Outcomes of reviewed studies
This systematic review aims to assess the effectiveness of CBT-I in treating patients from Arabic countries. The study contributes to the increasing number of research on non-pharmacological approaches to insomnia treatment. It analyzed existing studies to examine the effect of the treatment, study populations, the assessment of insomnia, various patient scopes, various formats in each study, and study results.
All Studies in this systematic review generated several outcomes, and the common outcomes indicate that CBT-I is effective in treating both primary and secondary insomnia by reducing the severity of insomnia from pre-test to post-test. CBT-I also effectively improves sleep quality and other sleep parameters. Moreover, CBT-I modified dysfunctional beliefs about sleep. All studies included in this review demonstrated the efficacy of CBT-I across different groups and treatment formats. Amer, et al. (2022) conducted a study in Egypt with 260 women who were experiencing insomnia associated with postpartum depression. The program consisted of nine group sessions of CBT-I, and the findings showed that CBT-I significantly reduced symptoms of both postpartum depression and insomnia in these women. Abdelaziz, et al. (2021) conducted a study in Saudi Arabia with 80 women with insomnia related to menopause, implementing an internet-based CBT-I program. The study showed that CBT-I effectively improved sleep and decreased insomnia related to menopause.
Three studies conducted in Egypt on CBT-I in elderly patients in a group context showed that CBT-I is an effective approach in decreasing anxiety and depression symptoms, in addition to reducing insomnia symptoms, which makes it highly recommended for old age patients [5-7]. Geagea, et al. conducted a pilot study in Lebanon, which included 19 patients, but four of them did not continue with the study [8]. The study found a significant improvement in insomnia symptoms, with no insomnia symptoms reported in the post-test. Furthermore, Salwen-Deremer, et al. conducted an individual-based CBT-I study in Lebanon with 20 patients suffering from insomnia with Inflammatory Bowel Disease (IBD). The study showed a significant improvement in improving sleep and reducing unhelpful thoughts associated with sleep and IBD disease activity.
Treatment formats
The systematic review by Mitchell, et al. has compared the effectiveness of various delivery settings of CBT-I. The review found no evidence of superiority for any specific setting of CBT-I [11]. However, the study revealed that group or telehealth settings of CBT-I have larger effects in comparison with self- help settings such as CBT-I and guided bibliotherapy. These results suggested that the mode of communication in delivering CBT-I can significantly affect its efficacy. Also, a study on the treatment of primary insomnia, compared the effectiveness of delivering CBT-I individually and CBT-I in a group setting. The results showed that individual setting was more effective in treating primary insomnia. Bastien, et al. conducted another study comparing the effectiveness of CBT-I in three different treatment settings: Individual, group, and phone consultation [12]. The findings demonstrated that CBT-I delivered in any of these formats improves sleep efficiency. The reviewed studies utilized various settings of CBT-I, such as individual, group, and internet based. Despite these variations, all studies resulted in improvement in the severity of insomnia. Out of the included studies, five conducted CBT-I in a group format and all showed a significant effect in improving insomnia symptoms [5-9]. Two studies delivered internet-based CBT-I and reported improvement in sleep appeared in sleep diaries and post-test [1,10]
Patients’ characteristics
According to a systematic review conducted by Morin, et al. in 1999, no evidence was found to support the existence of an association between gender and intervention results for insomnia [13]. Furthermore, the European guideline for the diagnosis and treatment of insomnia (2017) highlights that cognitive- behavioural therapy for insomnia (CBT-I) is suggested for all age groups. An updated review by Morin, et al. in 2006 revealed that elderly patients with primary insomnia and those experiencing insomnia related to physical disorders benefitted from CBT-I, either alone or combined with medication [14].
Three studies, which involved a total of 370 old age patients, demonstrated the efficacy of cognitive-behavioural therapy for insomnia (CBT-I) [5-7]. Post-test revealed that sleep efficiency and sleep latency significantly improved, and a decrease in insomnia symptoms.
Two studies were conducted with females, one of which involved menopausal females and the other postpartum females [1,9]. Both studies reported a decline in insomnia symptoms associated with menopause symptoms and postpartum depression symptoms, respectively.
CBT-I for patients with other physical or psychological disorders
The review conducted by Morin, et al. in 2006 showed that patients with medical and mental disorders benefited from cognitive-behavioural therapy for insomnia (CBT-I) in treating their insomnia [14]. Similarly, the European guideline for the diagnosis and treatment of insomnia recommends CBT-I as the first- line treatment for chronic insomnia and comorbid disorders [15,16].
This review included one study that assessed the efficacy of CBT-I with patients who had insomnia related to medical disorders. This study was conducted with patients suffering from insomnia with Inflammatory Bowel Disease (IBD) and showed improvements in sleep parameters, such as sleep quality, Total Sleep Time (TST), and efficiency. In addition, two studies examined the effectiveness of CBT-I with menopausal women and postpartum women, respectively. Both studies demonstrated that CBT-I effectively treats secondary insomnia [1-10].
Strengths and limitations
The significant strength of this systematic review is that all the studies included in it utilized valid and reliable assessment tools such as questionnaires and sleep diaries to evaluate insomnia and assess the effectiveness of CBT-I. The findings from these studies showed that CBT-I was effective in decreasing insomnia symptoms and comorbidity symptoms from pre-test to post- test. All the studies in this systematic review had a minimum sample size of 20 patients, with an average of 70 patients and a maximum of 210 patients. The use of large sample sizes is a significant strength of these studies as it increases their validity and accuracy of outcomes. There is one study that had a number of participants less than 20 patients, which was a pilot study by Geagea, et al.
This systematic review has a number of significant limitations. Firstly, the small number of studies that have examined the implementation of CBT-I in Arab countries may impact the generalizability of the findings. Another limitation is the lack of clear and particular eligible criteria related to sample size, demographics, intervention duration, follow-up, and treatment setting. This absence of standardization was due to the clinical diversity across the studies, resulting from the small number of studies using CBT-I in Arab countries. The reduction of similarity and consistency in the studies may have contributed to differences in the true treatment effects, leading to incompatible conclusions regarding the effect of CBT-I. These limitations restrict the level to which the findings of the studies can be compared and the strength of the evidence base.
In a future study, it is essential to consider several aspects that may impact the effectiveness of CBT-I. This will aid in gaining a good understanding of whether participant demographics and program delivery settings, such as face-to-face or through the Internet, influence treatment results. Assessing these factors will provide insights into which patient groups will get benefit from CBT-I and which setting is most appropriate for specific groups. Therefore, it is necessary to target these factors when assessing the effect of CBT-I in future studies.
Implications of findings
Enhancing awareness about the impact of insomnia on our lives is significant in promoting the adoption of sleep hygiene and requesting professional help to treat the condition. This can also motivate people to consider non-pharmacological treatments like CBT-I, rather than depending on sleep medications, which can have negative effects, increasing understanding of sleep and the consequences of suffering from insomnia is likely to enhance both clinical and research aspects. Comprehensive research can aid specialists in addressing unhelpful thoughts about sleep and promoting healthy sleep habits. This can increase awareness about sleep and its treatment in the Arab world and expand research on sleep disorders, facilitating the adaptation and validation of insomnia intervention within Arabic culture.
Future research directions
Furthering research on CBT-I can have significant advantages, including improving clinical practice for patients with insomnia, enhancing the understanding of negative insomnia’s effect on societies, and increasing of using evidence-based intervention options. Given the growing number of individuals who suffer from insomnia, giving more effort into research is important to fully appreciate the implications of suffering from insomnia. Continued study on CBT-I can help enhance a good understanding of the relationship between insomnia and medical and psychological disorders, which can lead to suitable treatment for secondary insomnia. Currently, there is a limited number of studies on the effectiveness of CBT-I as a treatment for insomnia related to other disorders, and more research is needed, especially in Arab Countries. By conducting more research in this area, we can improve medical care for individuals with insomnia and reduce the negative impact that insomnia has on society.
In summary, this systematic review evaluated the effectiveness of CBT-I in treating both primary insomnia and secondary insomnia in the Arab world. This study analyzed seven empirical studies, all of which indicated that CBT was effective in decreasing insomnia symptoms. Additional research with larger samples is required to further understand how to appropriately adapt CBT-I for patients with insomnia in the Arab world, considering the difference in culture and lifestyle. However, the growing awareness of sleep and its importance for physical, and psychological aspects in Arab countries. Additionally, the field of sleep medicine is expanding in Arab countries, with more professionals receiving training to use CBT-I in helping individuals with insomnia. As well as it is crucial to advance research in this area, not just to gain a good understanding of the challenges to implementing CBT-I in the Arab world and enhance treatment outcomes, but also to address unhelpful thoughts about sleep and increasing the use of sleep hygiene. Furthermore, further research can aid in raising awareness of the advantages of requesting professional help for insomnia in Arab countries. Moreover, there is a need to train more therapists in the Arab world to expand the scalability and availability of CBT-I treatment.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: El Basiouny D, Habib HI, Gharib A (2023) Cognitive Behavioural Therapy for Insomnia in the Arab World: A Systematic Review. J Sleep Disord Ther.12:478.
Received: 03-Oct-2023, Manuscript No. JSDT-23-27293; Editor assigned: 05-Oct-2023, Pre QC No. JSDT-23-27293 (PQ); Reviewed: 19-Oct-2023, QC No. JSDT-23-27293; Revised: 26-Oct-2023, Manuscript No. JSDT-23-27293 (R); Published: 03-Nov-2023 , DOI: 10.35248/2167-0277.23.12.478
Copyright: © 2023 El Basiouny D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.