Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Review - (2020)Volume 10, Issue 2
Coccydynia is a localized pain in the coccyx, is associated with functional or organic alterations of this area, which will generate problems in the movement of bone structure accompanied by chronic inflammation. The diagnostic method of choice will be the dynamic radiological examination. The basis of management is conservative treatment and if treatment fails it should be staggered to surgical treatment (coccygectomy).In this review, we will make an approach from the anatomy to have a clearer approach to the pathology and practical considerations at the time of treatment.
Coccygodyni; Coccydynia; Coccyalgia; Pain therapy; Coccygectomy; Functional radiographs; Dislocation; Hypermobility; Instability
The coccyx term derives from the Greek word Kokkyx, for its resemblance between the peak of the cuckoo bird and bone [1].The pain in the coccyx called coccydynia, was first described by Simpson in 1952. Later, Delamonica in 1966, described coccydynia as pain at the level of the coccyx and in the structures that are 5 cmfrom this bone. The causes of this symptom are very varied, finding with in those we find trauma, a chronic inflammatory process, tumors, among others [1,2].
Since coccydynia is a typical symptom in the female population, which usually occurs between the third and fourth decade of life, this clinical picture makes it an important subject for consultation, since women by nature have the sacrum shorter, wider and less marked than in the male sex. The ischialtuberosities are more separated and the coccyx is more mobile. All this makes the female coccyx more vulnerable to trauma than the male [1].
This condition has given rise to numerous works for having long been a mystery as to the causes, but thanks to the dynamic radiography (described in 1992) one can better understand the possible causes of this condition, the particular symptoms, and address rational treatment (Figures 1 and 2) [2].
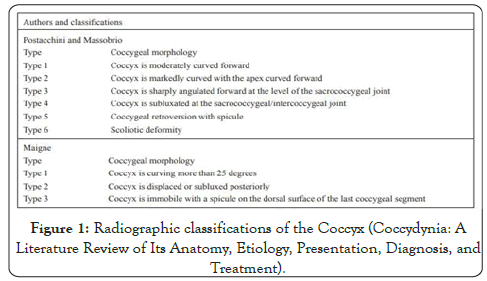
Figure 1.Radiographic classifications of the Coccyx (Coccydynia: A Literature Review of Its Anatomy, Etiology, Presentation, Diagnosis,and Treatment).
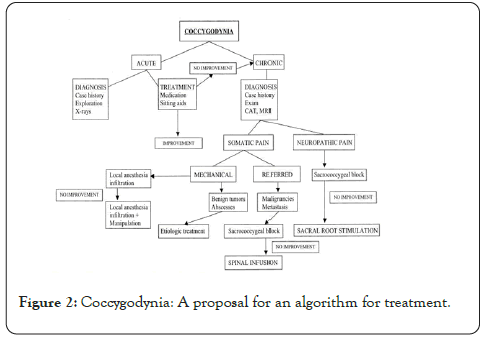
Figure 2.Coccygodynia: A proposal for an algorithm for treatment.
In serious disorders, clinical medical treatment is important to resolve this condition without having to resort to surgery, which is the last resort, the same that should be avoided as much as possible. However, not all pain that is referred to this region is produced by coccyx trauma, but there are multiple causes such as: infections of the perianal region, tumors, hernias, dysplasias, etc. A psychogenic component may also be present in many cases [3].
• Know about coccydynia and its possible causes in order to prevent and treatthem appropriately.
• Determine which is the age group most affected by this pathology.
• Identify the different behaviors and parameters established to arrive at the mechanisms used in the consultations of patients with this condition.
• Recognize the diagnostic methods used in this condition in order to treat it intime, acknowledging that many of the complications of some pathologies are due to the delay in their treatment.
• Identify the various methods and forms that exist for the treatment of coccydynia, and that many of them are conservative and others are interventionist measures.
General structure of the coccyx
The coccyx is located slightly above the anus. Like the sacrum, it is wedge-shaped and presents anterior or pelvic and posterior faces, two lateral edges, base and vertex. It usually consists of four segments (vertebrae), sometimes five and sometimes three, which are atrophied and do not have a vertebral arch. The first has short transverse processes that join with the sacrum, and two horns or horns of the coccyx that articulate with those from the sacrum. The fusion of the first segment with the sacrum is frequently partial and sometimes total. The second segment, which has rudimentary antlers, can be moved over the first, and this movement is preserved even when the first is fused with the sacrum, which is an important feature for the part. The third and fourth segments are rudimentary. The joint between the second and the third is sometimes mobile; that of the third and fourth is only occasionally [4,5]
There are almost vertical coccyxes that correspond to rather flat sacres, and horizontal coccyxes that correspond to very curved sacros; sometimes there are coccyx in "hook", thus, they are directed upwards, but they do not represent for us any pathological character. In fact, the less angle there is between the sacrum and the coccyx, the more protected the coccyx is from trauma as it is "sheltered" by the pelvis [2].
Joints
According to Gray, the sacrococcygeal joints are small, very thin intervertebral discs made of fibrocartilage; and the intercoccygeal joints can be synovial or disc. Nine coccyxes were examined in fresh cadavers of the elderly, where the sacrococcygeal joint was found to be disc in one case, synovial in four cases and intermediate in the remaining four. The joint consisted of a disc with a more or less important opening parallel to the cymbals and surrounded by annular fibers or synovial fibers. This intermediate state was not found in the intercoccygeal joints. It is unknown if this distribution would be in younger individuals, which makes one wonder if this opening progresses during life under the effect of mechanicalstress;evolving the disc progressively, in the same person, towards a synovial joint. Synovial joints allow greater mobility than discs. There is a fourth type in the form of complete ossification of the sacrococcygeal joint. Studying two different populations, the frequency of the ossifications was respectively 22% and 68% of the cases. In some of our patients, the coccyx was completely ossified.
Mobility
The physiological movements of the coccyx are those of flexion and extension. Active flexion (forward movement) is coupled with contraction of the levatorani and external sphincter. Extension (backward movement) is associated with relaxation of these muscles and increased intra-abdominal pressure that appears during defecation and delivery. It is always a passive movement. When there is movement, its direction is primarily determined by "incidence." The incidence of the coccyx has been described as the angle that the coccyx makes with the seat when it comes into contact with it when sitting down. If the incidence is small, the coccyx tends to appear parallel to the seat. It is then pushed forward and up (flexed) by the same seat. If the incidence is high, it tends to be perpendicular to the seat. It is then pushed back, in extension, by increased intrapelvic pressure. The incidence is linked to the shape of the coccyx and the sagittal pelvic rotation. Small incidence coccyxes are long, curved coccyxes (more than two vertebrae). In contrast, straight and short coccyxes have a high incidence. The shape of the coccyx is described in four types, from the straightest (type I) to the most curved (hook coccyx, type IV) according to the classification by PostacchinietMassobrio, or by measuring the intercoccygeal angle intersecting the axis of the coccyx and S4. The closer the latter approaches 180°, the straighter the coccyx; the closer it gets to 90°, the more curved. Incidence is linked to another angle: sagittal pelvic rotation. This angle measures the rotation of the pelvis during the passage from standing to sitting. This rotation is accompanied by a decrease in lumbar lordosis. When the angle of rotation is large (up to 60°), the incidence is small. In general, these are individuals whose body mass index (BMI*) is normal or low. When it is small (less than 30°), the incidence is high. In general, they are subjects with high BMI (>27). The volume of your pelvis can be considered to limit natural rotational movements.
Other factors may limit this rotation, in particular the loss of mobility of the lumbosacral hinge (discopathy, sequela of discectomy, arthrodesis) or simply due to a high seat. Ligamentous hypermobility or a low seat increases it. These factors may influence the triggering of coccygeal pain. The absence of movement during sitting can be attributed to ossification of the coccyx joints or the presence of disc-type joints. The man’s coccyx in general is less mobile than the woman’s [6].
It is a painful syndrome of the coccyx and surrounding area that decreases in a sitting position. In which there will be anatomical variations related to the onset andpersistence factors [1].
Obese people are more likely to have unstable movement of the coccyx due to the lower degree of pelvic rotation (<30 degrees), which leads to more pronounced angles and because of this, their coccyx tends to protrude while sitting.
Age will also be a risk factor because adults are more likely to have spicules, which are excrescences in the dorsal region, characteristics of immobile coccyx [7-22].
Tailbone pain is much less common than pain in the lumbar spine, but there is alack of exact data on its incidence [18]. Coccydynia constitutes less than 1% of non-traumatic consultations of ailments of the spine [16].
The main etiology is traumatic. It can also be caused by tumors, infections, cysts and by idiopathic cause[1].
It has been found mainly in women between 30 and 50 years old due to falls in a sitting position [3].
This pathology has a 5 to 1 relationship between women and men [3].
Except for coccydynia in which trauma is confirmed to be the triggering factor, there seems to be no consensus about the rest, regarding the origin of this condition. Various authors have studied the morphology of the coccyx to be able to establish clear diagnostic criteria.
Based on radiographic images, he develops a classification that explores the important role of tailbone morphology.
Type I: The tailbone is curved with the apex in the caudal direction.
Type II: the tailbone is curved with the apex in the anterior direction.
Type III: The angle formed by the sacrum and coccyx is acute.
Type IV: The coccyx is previously sub-luxated.
According to this classification, types II, III and IV are more likely to suffer coccydynia. Subsequently, Nathan et al. [23] suggested two more morphological types of coccyx, also involved in coccygeal pain.
Type V: Coccygeal retroversion with spicule.
Type VI: Scoliotic coccyx deformity.
In most cases the pain occurs during sitting, so it seems clear that the mechanical cause is involved in coccydynia. Maigne [7] develops a dynamic radiography protocol to establish a criterion valid diagnosis. Based on this, the radiological findings are classified into the following items [13].
Posterior dislocation of the coccyx: corresponds to type I of the classification of Postacchini. It is the quintessential post-traumatic injury. Represents 20% of chronic coccydynia. It can only be seen in the radiological images taken in sitting since the dislocation is reduced when the patient stands up. Appears in the straight tail bones, which move backwards during sitting [13].
Hypermobility
Accounts for 25% of coccydynia cases. It practically affects only women with low or normal BMI, in which sagittal rotation is high and the tailbone is rather curved. It is often associated with impaction of the anterior part of the two bony pieces of the hypermobile junction and/or a minimum Forward dislocation of the distal part, forming a small step appreciable only in the sitting position. To ensure the responsibility of the pain, it is necessary that the most painful point on palpation corresponds with the hypermobile junction and that the injection of a steroid at this point, relieves the patient for at- least a month. Both posterior dislocation and hypermobilityareobjective causes of instability of the coccyx that manifest when the weight of the body is loaded during sitting [23].
Coccygeal spines
It is the cause of 15% of coccydynia cases. It is present from birth,
and usually manifests itself in young patients who have lost weight and with it, its protective perineal fat pad. The pain appears spontaneously in the joint involved. The bony peak of the tip of the coccyx rests strongly on the dermis during sitting and creates inflammation. The coccyxes are long and curved, and a cutaneous pit. The X- ray shows a tailbone without mobility [23].
Anterior dislocation
It is a very rare injury and represents 5.3%. The most distal part of the coccyx that can occur in the curved coccyx is involved. It corresponds to Postacchiniand Massobrio types III and IV [23]
Coccydynia is stabbing or mild but persistent pain in and around the coccyx area. It can range from mild discomfort to sharp pain; each person feels it differently and even for the same person the pain changes over time. The name describes a pattern of symptoms (sitting causes or aggravates pain), so it is actually a group of conditions, which can have different causes and need different treatments [2].The pain can radiate to the lower region of the sacrum and to the perineal area, sometimes it comes with tenesmus.
It is typically caused by a traumatic injury to the tailbone, such as a fall on the buttocks in a sitting position. Another frequent cause in women is the trauma of childbirth that occurs during a difficult delivery, successive sprains, strains or surgical operations. In some patients, the disc between the fifth lumbar vertebra and the first sacral vertebra (L5-S1) can cause referred pain felt in the coccyx. However, many times there is no identifiable cause of coccydynia (idiopathic) [7].
The pain may go away on its own or with treatment, or it may continue for years and even in some cases, it can get worse. It is five times more common in women than in men, probably because the female pelvis leaves the tailbone more exposed. It seems that in most cases, the pain is caused by an unstable coccyx, which causes chronic inflammation. It can also increase with defecation, which is easy to understand, if we think that the rectal ampulla rests directly on the coccyx itself and the lower 1/3 of the sacrum, which means that by increasing the pressure of the walls of the same This directly affects the functional stability of the altered sacrococcygeal joint, especially in cases of evacuative overstraining due to constipation [24-31].
Risk factors for coccydynia are staying in a sitting position for prolonged periods; any activity involving repeated blows to the tailbone, such as riding, riding a motorcycle or bicycle, operating a tractor, an fourth motorcycle (ATV), or a snowmobile; inadequate posture when sitting, and surgical intervention carried out with the individual lying on their back with their knees flexed (lithotomy or sacral dorsal position). Psychological problems, such as hysteria or depression, are believed to be a risk factor for the onset of coccydynia. The incidence is rare; only explains 1% of back pain conditions reported to doctors [8].
• Pain while sitting or getting up:This is the main pain caused by coccydynia. Depending on the design of the chair and its padding, it will be more or less painful. The increased pain and sensitivity caused by having to sit for a long period of time can last for days.
• Acute pain when moving from sitting to standing.
• This symptom is particularly interesting, since Dr. Maigne [32] discovered that all the patients he studied and who presented with this symptom had a partially dislocated or abnormally displaced coccyx when the patient sat down.
• Pain caused by sitting on a soft surface, but not if it is hard.
• This occurs when the joint between the sacrum and the coccyx is unstable, so that the coccyx can be pushed out of place by putting pressure on it when sitting. When you sit on a hard surface, most of your weight rests on the ischia, which are the pelvic bones that we sit on. But when you sit on a soft surface, the padding pushes between these bones, increasing the pressure inside your body and pushing the tailbone out of place.
• Deep pain around the tailbone.
• Finger pressure sensitivity at the tip or sides of the coccyx.
• Pain radiating down the legs.
• How to sit on a moving marble.
• How to sit on a knife.
• Pain when defecating and sometimes after it.
• Pain during intercourse, both in men and women.
• Increased pain before menstruation, this may be due to variations in the level of estradiol.
• If the pain is caused by a blow, other parts of the body may be injured. If the damage includes the sacrum, hips, or legs, it can be very difficult to separate what is causing the most pain. A local infiltration of anesthetic into the tailbone area helps determine how much pain is caused by the tailbone.
If the pain continues for a long time, it is common for secondary symptoms to appear, such as:
• Foot pain, from standing for too long. A particular problem that may appear is plantar fasciitis, which is inflammation of the fibrous tissue that surrounds and connects the muscles. It is a common problem in people who work standing up, especially if they are over 40 or overweight.
• Tiredness, depression, lack of sleep. It is obvious why these symptoms develop when the pain continues.
• Back pain, from sitting forward to decrease pressure on the coccyx. If back pain is caused by bad sitting and did not start earlier than tailbone pain, manual treatments such as physical therapy, osteopathy, and chiropractic are often helpful.
• Other body aches. Pain in one body region can lead to hypersensitivity in another region, due to cross-linking of nerve fibers. In the case of tailbone pain, the entire buttock area can be affected. This, of course, makes sitting even more uncomfortable, and the chairs or positions that were originally valid become uncomfortable.
Because coccygodynia is painful in a sitting position, practicing a sitting profile X-ray compared to a standing X-ray becomes essential if coccydynia is chronic. Violent trauma or significant pain may warrant shorter times.
Rx is first practiced while standing. For the coccyx to be in a neutral position, it is important that the patient avoid sitting for the 5-10 minutes preceding the Rx. In addition, in certain cases of hypermobility, the coccyx would not have time to regain its usual neutral standing position. The patient then sits in a chair, with the feet supported so that the thighs are horizontal (which mimics normal sitting) and must seek pain. If necessary you can lean back to feel it. If the pain cannot be spontaneously provoked
after a reasonable period of a few minutes, the sitting X-ray is less demonstrative, since it is taken in a no-pain situation. The radiograph should be done in the position where the patient usually has the most pain [32].
Angle mobility
Thus the angle of mobility of the coccyx can be traced, the apex is located in the center of the first mobile disc. In 2/3 of the cases it is a forward movement (flexion). The normal value observed with the control subjects is between 0° and 25°A value higher than 30°in women (25° in men, is abnormal. In 1/3 of the cases, the coccyx moves backwards (in extension), a movement that does not exceed much 15°, it only increases exceptionally. Angle of mobility is the most important. Its measurement must be systematic, except when there is a dislocation that prevents the measurement, making it meaningless. It does not happen as with other angles that are only of biomechanical interest.
Pelvic sagittal rotation
In order to superimpose the two sacres (sitting on the standing one), it is necessary to rotate the plate while sitting a certain number of degrees, which represent the value of the rotation of the pelvis during the passage from standing to sitting (considering sacroiliac mobility as null). In a thin subject, this angle is greater than 40°. In the obese it is less than 30°. Pelvic rotation and incidence are closely related to the body mass index
Posterior luxation of the coccyx
Dislocation is the most surprising injury to the coccyx. It represents around 20% of chronic coccydynia. Apart from some rare cases of permanent dislocation, it only appears when sitting and spontaneously reduces when the patient stands up. This explains why, before our work, it was not individualized. The dislocation appears in the rather straight coccyx, with small pelvic rotation and high incidence. The sacroccocígeos and intercoccígeos discs are equally involved. The displacement of the tailbone is always backwards. The analysis of the control series has shown that it must exceed 20% (according to the measurement analogous to that used for (spondylolisthesis) to be significant. In general the recoil is 50% to 100%, and there is practically no discussion about his responsibility for pain.
Dislocation is the quintessential post-traumatic injury. Poor pelvic rotation and high incidence translate to a rearward tailbone, particularly exposed to injury during a fall. It appears more often in case of weight overload, not because the obese do more damage by falling, but because of their specific way of sitting; as evidenced by the small sagittal pelvic rotation (mean <30°), which means that they have a tendency to drop onto the seat.
In the event of dislocation, coccygeal pain has two characteristics that make it suspicious during the clinical examination: it appears immediately when sitting and is often accompanied by pain when getting up (sometimes it is the only symptom). The intensity of pain is greater than in other causes, so patients come to the consultation earlier.
Hypermobility
In hypermobility, a very strong flexion of the sitting coccyx is characteristic, greater than 30°. It is often associated with an impaction of the anterior part of the two bony pieces of the hypermobile junction and / or a minimal dislocation forward of the distal piece; forming, in the sitting, a small step. It represents 25% of the coccydynia. Typically, hypermobility appears in subjects in whom the sagittal pelvic rotation is high and in whom the coccyx (generally rather curved) appears more horizontally in front of the seat, which translates into an incidence of less than 35°. Hypermobility practically only exists in women. It appears especially in the subject of normal or thin weight, also here due to the way of sitting, with a significant pelvic rotation that pushes the coccyx to appear parallel to the seat and withstand flexion stresses. It is rarely traumatic.
Contrary to dislocation (which is always pathological if the displacement is greater than 20%), moderate hypermobility (around 30°) is not necessarily pathological. They may exist in asymptomatic hypermobile patients. To ensure responsibility forpain, it is necessary that the most painful point on palpation corresponds to the hypermobile junction, and that the injection of a steroid at that point relieve the patient for at least one month.
Espinas coccygeal
The spine (or spicule) is a palpable bone peak under the skin at the tip of the coccyx. Assaults the dermis while sitting and create inflammation (bursitis). It is the cause of coccydynia in 15% of cases. They are long and curved coccyxes. In almost 80% of cases, a more or less defined skin abnormality occurs: a cutaneous pit. It is rarer to see a pilonidal cyst. This means that the sinus and spicule are mirror lesions, as if there had been a coupling of two embryonic leaves to which it was wrong to separate.
Dynamic X-rays often show a non-motile coccyx that increases the pathogenic nature of these spicules (due to the absence of flexion, the coccyx cannot move away from the skin and strongly supports sitting). Sometimes it is difficult to see the spicule. A 3D reconstruction of the scanner can be done, but the best option is MRI when the Rx are difficult to read [33]. Present from birth, the spike is far from always the cause of pain. It can be found in people who have never had coccyx pain in their life. A condition for it to become painful is a low BMI, that is, a certain thinness that eliminates the protective perineal fat pad.
The coccygodynia due to a spicule in general are not traumatic as it is a purely inflammatory lesion. The onset is very often spontaneous, sometimes after psychic trauma. Another very evocative context is that of coccydynia that appeared after a weight loss of several kilos, for the aforementioned reason. The clinical examination allows suspecting the diagnosis. In addition, the presence of a cutaneous pit, the pain felt at the tip of the coccyx, near the anus. Palpation is decisive, since the sharp relief of the spicule is perfectly noticeable and the familiar pain is easily reproduced with a simple pressure. If there is a pilonodal sinus, it is essential to ensure the absence of purulent substance.
In 1/3 of the cases, no radiological lesion was observed. First of all, you have to ask yourself about the technical quality of the Rx exam. That is: was the pain present during the X-ray of the sitting patient? Dynamic radiographs have been taken in the absence of pain.
If pain was absent, there are two possibilities. There may be an outline of injury such as a "limit" flexion (for example around 25°) or a disrete one. Certain patients only feel pain in a specific seat or in particular circumstances (car travel, which associates vibrations with sitting). If no outline of injury is seen, it is best to repeat the dynamic Rx in good condition.
Dynamic radiographs taken in the presence of pain: If the pain was present and there is no abnormality of mobility, it is impossible to draw conclusions about the origin of the pain. Some of these cases (more than half) respond well to intradiscal steroid injection, which seems to prove the presence of intradiscal inflammation. Other cases may respond to the injection of the steroid into the tip of the coccyx (in the absence of a visible spine). It is probably apical bursitis that appears in coccyx without mobility in which the pain is located at the tip. But the infiltration may have no effect and the etiology of these cases remains unknown.
The absence of any concomitant low back pain must first be verified. If the tailbone appears to be solely responsible, there are different sources of pain that can be argued.
It's about hypotheses. They are plausible but cannot be proven. It may be pain originating in the levatorani. In this case, the rectal examination finds one or more painful points in these muscles, the pressure of which reproduces the spontaneous pain. We don't know why these muscles are a source of pain. Manual treatment will be of choice in these cases. It may also be pain in the insertion of a muscle or ligament at the lateral edge of the sacrum or coccyx. Careful palpation of the lateral edges of the lower end of the sacrum and the first coccygeal piece may show localized, unilateral pain, which could correspond to insertion pain of some fibers of the gluteus maximus or the sacrotuberous ligament. A depressive state or simply the history of a depression, a tendency to spread pain, the not strictly mechanical nature of the pain (that is, that it does not appear more than after a time of sitting, for example after a hour, and that its intensity increases as the day progresses), are elements that guide the etiology. A depressive state, by itself, cannot create a coccydynia, but it can favor its persistence, due to a phenomenon of sensitization or memory of pain. Treatment with amitriptyline may be proposed to the patient [3].
The treatment of coccydynia cannot be addressed until its cause is known; it has been viewed only from the conservative and interventionist points of view.
Conservative Treatmentis achieved through rest, the use of antiinflammatory medications at each time and the application of physical measures aimed at analgesia (thermotherapy, electrotherapy, orthotic protections for sitting at workand in vehicles), as well as manual treatments. These measures can be reinforced by the association of neurostabilizing medication (gabapentin or pregabalin) in those cases where the pain has neuropathic characteristics, or anxiolytic medication in cases with a marked functional component. Patients should also be advised on measures to correct constipation in the event of this circumstance and the recommendation to avoid certain sexual practices that can negatively influence the process, such as anal intercourse [8].
The way of sitting is essential. You have to choose the most comfortable seat, avoid sitting for a long time, knowing how to sit on your buttock or in the front of the seat, on your thighs.
Avoid long car trips. Antalgic drugs are sufficient in acute coccydynia.
Tricyclics are sometimes helpful in idiopathic coccydynia that do not respond to injections or manual treatment; or in case of failure of surgical treatment.
The float can be used in cases of resistant pain; or in a “preventive” way during long journeys by car, always poorly supported. There are emptied cushions, more aesthetic. Sports are not advised, such as cycling and horse riding.
Interventional treatment rests on three major techniques: injection, manipulation, and surgery. Minor techniques (special cushions, seat modifications) provide additional help.
Coccygeal injections
The first is an intra-discal procedure under fluoroscopic control and we specify how to select the disc to be injected.
Intradiscal injection technique
An injection like this can only be done reasonably under fluoroscopic control. The patient stretched out on the left side, flexed hips and knees. The disc to be injected must be identified with two complementary means. The first is dynamic Rx. If there is marked dislocation or hypermobility, there is no doubt. If the hypermobility is moderate, or if the Rx is normal, help with careful palpation of the coccyx, from the lower end of the sacrum to the tip of the coccyx; to identify the most painful area (or the one that under pressure reproduces the patient's pain best). Then we mark it with a metallic object that allows us to verify on the monitor the disk to which it corresponds. By adjusting its position in the midline, exactly in front of the disc, the needle insertion point is identified.
The end of the mark is replaced by a piece of felt, since the skin is disinfected with iodized alcohol. Local anesthesia is performed with a fine subcutaneous needle. A fine 25mm needle is inserted into the center of the disc. In obese patients, a longer needle (50 mm) is required. This placement is not always easy. The needle may trip over small osteophytes or deviate the path if it is lateral to the coccyx. Avoid pushing it too far as the safety space to the posterior rectal wall is 5 mm. The examination ends with the injection of approximately 2 ml of prednisolone acetate. The immediate evolution is practically painless. You may encounter an allergy to iodine, an infection, a puncture of the straight wall.
Tip injection technique
Tip injection is indicated in the presence of, or in the absence of, a spike when the tip is the most sensitive region without abnormalitiesin dynamic X-ray. The technique is the same as that of intradiscal injection. On the contrary, evolution is sometimes painful for a few days.
Injection is often slow to be effective, especially in cases of tip injection. Its effect can be evaluated after three weeks. The effect is generally maintained until the third month, being excellent or good in 75% of cases. After three months, the results may decrease and a flare-up may appear in about 1/3 of the patients.
In case of reappearance, it is logical to propose a second injection. If effective for longer than the first, infiltration treatment has a good chance of curing the patient. In the opposite case (worse result than with the first one), it is better to renounce the infiltrations and to propose another treatment.
The global efficacy of the treatment by infiltrations is 65% of good and excellent results after one year; the dislocations respond slightly but (50% of good results), and the spicules are the ones that give the best results (80%).
Manual treatment
Manual treatment is the oldest treatment for coccydynia. The basic techniques are: massage of the levatorani, mobilization of the coccyx in extension, and stretching of the levatorani. They are practiced rectally, at an average of 3-4 sessions in two weeks. The results of manual treatment vary depending on the cause of coccydynia. Patients with radiological injury (in particular, instability; dislocation or high hypermobility) obtain the worst results (15% to 20% success, hardly more than placebo). Those of coccyx without abnormality of mobility have the best results (around 30% of good results). This is logical. Dislocations andhypermobilities are anatomical lesions that them-selves (especially if the injury is severe) are a source of pain, which reappears soon; since the manipulation only acts on the muscular component (painful tension)(De J, Chaves S [25]).
Surgical treatment
The removal of the coccyx has long had a bad reputation, despite the good results published in the literature. The coccygeal exeresis is directed exclusively at disabling instabilities, not alleviated by other means. It gives good results in more than 90% of cases.
The improvement appears in the second or third month, sometimes only in six or ten months. In some rare cases it takes one to two years before final cure. This long wait could be attributed to the presence of deferential pains (phantom limb syndrome). The context of workplace accident or medical-legal conflict is pejorative. Even patients with instability but without any response to intradiscal injection are at increased risk for worse results.`
The intervention consists of resecting the unstable portion of the coccyx. In the case of a spicule, it is the distal end that is respected, while the associated pilonidal is removed. The intervention is performed under general anesthesia, with a small incision in the intergluteal fold [33-35]. The posterior aspect of the coccyx is exposedandthedissectionismadeincontactwiththebone. Despiteprecautionsfor pre- and post-operative asepsis and 48-hour prophylactic antibiotic therapy, infection complicates 2% to 3% of interventions.
• Coccigodynia appears in the form of a pain, generally of chronic evolution, which is located at the caudal end of the spinal column, radiating from there to the lower region of the sacrum and to the perineal area, sometimes accompanied by sensation of tenesmus.
• The coccyx, as a mobile element of the spine, bases its functional stability on the sacrococcygeal joint, which supports it to the spine, on two stability ligaments, the posterior sacrococcygeal and the anterior sacrococcygeal.
• Injuries are the main cause of coccydynia, but not the only frequent cause in women is the trauma of childbirth that occurs during a difficult delivery, subsequent sprains, strains or surgical operations.
• The injuries that cause coccydynia are, for the most part, injuries similar to those that affect the peripheral joints, and not psychiatric problems neglected by the patient.`
• The diagnosis is almost always based on the clinical history, especially on the anamnesis to discover a traumatic history, and on palpation examination of the area and its vicinity, where inflammation can sometimes be seen and the extent of the painful area can be delimited.
• In general, the straight and short coccyxes, when subjected to many important str, dislocate due to the absence of natural mobility in extension. Conversely, the elongated and curved coccyxes can flex to absorb tension. It is only after a certain threshold that hypermobility appears, which is nothing more than the exaggeration of a normal phenomenon of flexion. A coccyx devoid of mobility becomes potentially aggressive as it can rub subcutaneous tissues during sitting (if there is a spike). The "good" tailbone is a long, curved, slightly flexible tailbone.
• Complementary studies, such as radiographs, make it possible to check fractures and the disposition of the coccyx in relation to the sacrum. Because coccygodynia is painful in a sitting position, practicing a sitting profile X-ray compared to a standing X-ray becomes essential if coccydynia is chronic. Violent trauma or significant pain may warrant shorter times.
• The treatment of coccydynia cannot be addressed until its cause is known; it has been viewed only from the conservative and interventionist points of view. Conservative Treatment is achieved through rest, the use ofanti-inflammatory medications at each time and the application of physical measures aimed at analgesia (thermotherapy, electrotherapy, orthotic protections for sitting at work and in vehicles), as well as manualtreatments.
• Interventional treatment begins with minimally invasive techniques such as local infiltration techniques with anesthetics and corticosteroids and ends with Surgical Treatment, which consists of partial or total coccygectomy.
Citation: ManotasJA, Pérez SG, Suaréz MJ (2020) Coccydynia: Quick Review. Rheumatology (Sunnyvale).10:261. DOI: 10.35248/2161-1149.20.10.261.
Received: 29-Apr-2020 Accepted: 13-May-2020 Published: 20-May-2020 , DOI: 10.35248/2161-1149.20.10.261
Copyright: © 2020 Manotas JA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.