Journal of Sleep Disorders & Therapy
Open Access
ISSN: 2167-0277
ISSN: 2167-0277
Case Report - (2021)Volume 10, Issue 7
Falls in the elderly is an ongoing problem and is one of the leading causes for trips to the emergency room, hospitalizations, serious injuries, and expensive health care costs. However, many times the relationship between sleep quality and falls oftentimes is overlooked. Here we present a case of a 75-year-old female admitted for sustaining 4-5 falls per day for many years that was ultimately found to be due to chronic sleep deprivation. She was treated with non-invasive positive pressure ventilation (NIPPV) for her complex sleep apnea and hypercarbia. Subsequent follow-up revealed significant decrease in her number of daily falls down to <1 per day. This case further adds to the data showing a link between treating sleep apnea in the elderly and a reduction in falls.
Abbreviations : CT – computed tomography ; CPAP – continuous positive airway pressure ; EPAP – expiratory positive airway pressure ; Lpm – liters per minute ; MSLT – multi-sleep latency test ; NIPPV – non-invasive positive pressure ventilation ; OSA – obstructive sleep apnea ; PFTs – pulmonary function tests ; Pmax – pressure max ; REI – respiratory event index ; REM – rapid eye movement ; SpO2 – oxygen saturation
Obstructive Sleep Apnea; Sleep deprivation
Each year, 3 million older people are treated in emergency departments for fall-related injuries and over 800,000 of these patients end up hospitalized each year [1, 2]. These falls can lead to serious injuries such as broken bones, hip fractures, and traumatic brain injuries leading to expensive health care costs [3]. In 2015 alone, the total medical costs for falls totaled more than $50 billion and substantially contributing to the increased costs of medical care making falls an ever present concern in the elderly3. Recently, many have looked into the relationship between chronic sleep disturbances as a risk factor for falls showing that both chronic sleep deprivation and excessive sleep can result in increased falls [4, 5]. Here, we present a unique case of a patient who has been chronically sleep deprived for years leading to the development of atonia and micro-sleeps that was the source of her ever increasing daily falls.
Report of Case
The patient is a 75-year-old female who was admitted with a history of increased falling to the point where she had fallen a total of 4 times the day prior to admission. She began falling sporadically about 3 years ago while walking and it has progressed over the years to the point where she consistently falls multiple times during the day. She cannot pinpoint any triggering events, she denies any auras preceding the falls, she denies tripping or losing her balance that causes the falls and says she does not feel weak. She describes the events as such: she will be walking along then suddenly falls. She is aware that she is falling yet feels as though she cannot reach out and grab ahold of anything to prevent/stop the fall or help her break her fall. No one has ever witnessed one of her falls, but family frequently finds her lying on the floor. She has never sustained a serious injury such as a broken bone or head bleed as a result of her falls.
She does have an 8 year history of restless legs syndrome treated with ropinirole. She describes the symptoms of her restless legs syndrome as typically beginning around 1400 with tightening in her legs making them feel "rock hard." To improve this feeling, she uses a rolling pin or a hairspray can to massage her legs and stand or walk, although this does not completely eliminate her symptoms
The sensations in her legs persist through the night leading her to will stand up to watch television and her husband to sleep in a separate bed as her leg movement wakens him, but the ropinirole has been helping.
She has a 10 year history of obstructive sleep apnea originally diagnosed via sleep study and treated with continuous positive airway pressure (CPAP), which she wears every night. However, she has not had a recent sleep study nor has her CPAP machine or settings been updated since the time of her original diagnosis. Her sleep hygiene is poor at best. The time at which she goes to bed is variable but generally around 2200 and generally awakens for the day around 0400. She feels constantly fatigued during the day; falls asleep immediately as a passenger in a car, falls asleep after the evening meal and will even fall asleep during conversations. She denies having had problems with daytime hypersomnolence as an adolescent or adulthood until she was diagnosed with obstructive sleep apnea (OSA). She suffered back trauma in a motor vehicle accident in her 20s resulting in chronic and progressive back pain that affects her quality of sleep. She is aware of having COPD and says that she has a nebulizer, a rescue inhaler and umeclidinium bromide/vilanterol inhaler prescribed by her primary care geriatrician. She has chronic hypoxemia and is on 3L home oxygen via nasal cannula.
On initial presentation, she was found to be tachycardic and tachypneic (vitals: 37.1 C 117 HR 24 RR 228/95 BP 78% O2 sat on 2L NC). Her chest x-ray showed no consolidation, pulmonary infiltrates or pleural effusions. Computed tomograophy (CT) scan of the head showed no evidence of infarction or bleed but did demonstrate left maxillary sinusitis. Her initial lab values can be seen in the supplementary material. Her tachycardia and initial tachypnea were deemed physiological responses to her urinary tract infection and she was initiated on antibiotic therapy. Neurology was consulted to aide in the workup of her falls due to her history of seizures and multiple drugs that could cause sedation. After obtaining an electroencephalogram while inpatient, she was deemed not to be having active seizures and were not contributing to her falls. Nerve impingement and central nervous system causes as reasons for her falls was ruled out via magnetic resonance imaging of her spine and brain which only showed mild spinal stenosis. Finally, our team was consulted to help manage this patient’s chronic hypoxia with hypercapnia. As she was not acutely ill, we obtained initial pulmonary function tests (PFTs) to further characterize her lung disease, which showed significant airflow limitation with mild air trapping and severe diffusion impairment. Thus, the final working diagnosis was that she was suffering from longstanding sleep deprivation due to chronic pain and undertreated complex sleep apnea causing her to have micro-sleeps with rapid eye movememt (REM) sleep onset and atonia.
Sleep Studies
Due to the patient’s perceived urgency at finding a source for her falls, a nocturnal sleep study followed by multiple sleep latency test (MSLT) were obtained. The results of those studies are as in (Figure 1) and revealed severe, persistent daytime sleeping some of which contained REM sleep and atonia. During her CPAP titration study, her O2 requirements were titrated to 5 liters per minute (Lpm) with CPAP at 19 cm H2O and she slept for 1 hr 49 min with these settings, which included 57 minutes of REM. Her respiratory event index (REI) was 2 per hour, minimum oxygen saturation (SpO2) was 74% on 5 Lpm of O2, and spent 76 minutes with ≤ 88% SpO2 with O2 at 5 Lpm and CPAP at 13 cm H2O.
She slept 7+ hours obtaining a sleep efficiency of 90% with a sleep latency of <1 minute. REM onset was at 9 minutes, and the arousal + awakening index was 7 events per hour. REM accounted for 33% of total sleep time. MSLT showed severe objective daytime sleepiness with a mean sleep latency of 2 minutes, and 1 sleep-onset REM period observed on nap #3 with sleep latencies ranging from 1.5-5 minutes across 5 nap opportunities.
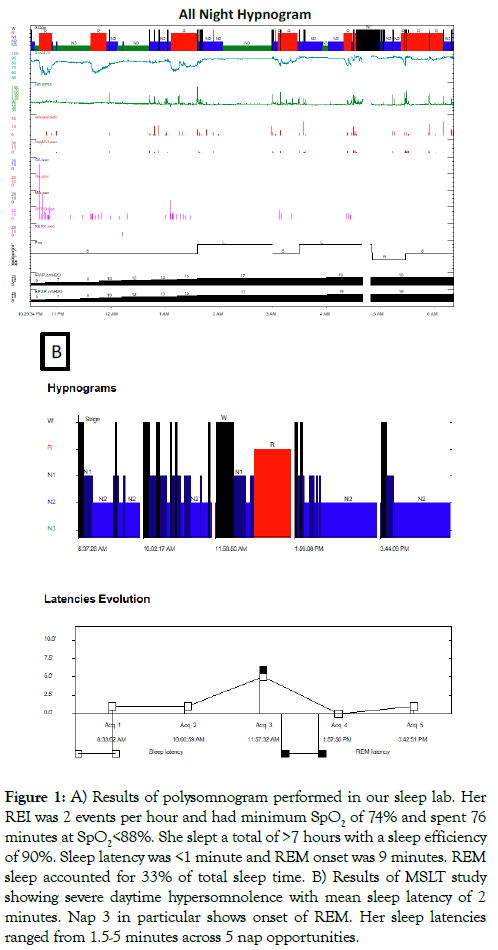
Figure 1: A) Results of polysomnogram performed in our sleep lab. Her REI was 2 events per hour and had minimum SpO2 of 74% and spent 76 minutes at SpO2<88%. She slept a total of >7 hours with a sleep efficiency of 90%. Sleep latency was <1 minute and REM onset was 9 minutes. REM sleep accounted for 33% of total sleep time. B) Results of MSLT study showing severe daytime hypersomnolence with mean sleep latency of 2 minutes. Nap 3 in particular shows onset of REM. Her sleep latencies ranged from 1.5-5 minutes across 5 nap opportunities.
Treatment
Due to her failing previous CPAP therapy, it was decided to start her on non-invasive positive pressure ventilation (NIPPV) therapy for her complex sleep apnea with hypercarbia. We started her on the following settings: Pressure max (Pmax) 28, pressure support max 17, pressure support min 8, expiratory positive airway pressure (EPAP) max 15, EPAPmin 10, VT 350, FIO 3, and rate set to auto. She was instructed to use her NIPPV at night and during the day for all naps. At her first follow-up appointment, she reported that she has been using the NIPPV for approximately 4 hours per night from 11pm – 3am. Data from her Trilogy machine showed that she was averaging 4.75 hours of use per night and she was not using supplemental oxygen. She attributes this short amount of sleep to the alarm going off on her machine and mask leak causing discomfort. At the time of this follow-up, she endorsed improvement of daytime hypersomnolence, and her number of falls each day has decreased from 4-5 falls to an average of 1 fall per day. She describes her most recent fall as such: she was standing then suddenly felt herself becoming weak like she was being paralyzed then fell to the floor without losing consciousness and spontaneously recovered.
On subsequent follow-up 3 months later, she reports her daytime hypersomnolence had resolved, her exercise intolerance had improved, and her oxygenation had improved to the point where she now holds 89-90% oxygenation on room air without supplementation. Importantly, she has not had any more falls at home. During her initial sleep study the patient spent most of the night with oxygen saturations well below 90%. (Figure 2) shows how treatment with the NIPPV improved her nocturnal oxygenation as evidenced through repeat nocturnal oxygenation saturations. The first nocturnal oximetry study was performed about 1 month after NIPPV treatment was initiated and 2 months after her sleep study, and showed a mean nightly oxygenation of 85.98%. One month later, her mean nightly oxygenation had increased to 89.16%, and 2 months later it had increased again to 91.76%.
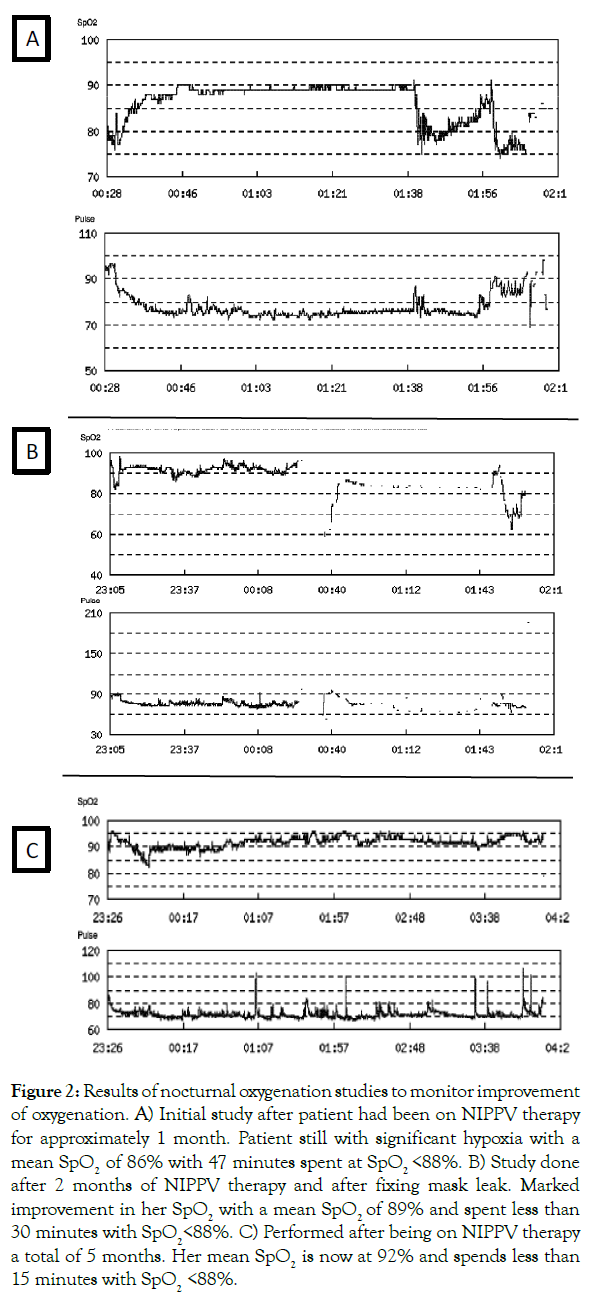
Figure 2: Results of nocturnal oxygenation studies to monitor improvement of oxygenation. A) Initial study after patient had been on NIPPV therapy for approximately 1 month. Patient still with significant hypoxia with a mean SpO2 of 86% with 47 minutes spent at SpO2 <88%. B) Study done after 2 months of NIPPV therapy and after fixing mask leak. Marked improvement in her SpO2 with a mean SpO2 of 89% and spent less than 30 minutes with SpO2<88%. C) Performed after being on NIPPV therapy a total of 5 months. Her mean SpO2 is now at 92% and spends less than 15 minutes with SpO2 <88%.
Here, we presented a unique case of a 75 year old female with recurrent falls that we hypothesized were secondary to chronic sleep deprivation causing micro-sleeps that likely involve REM sleep and atonia. Her MSLT showed that she frequently and rapidly goes into REM sleep during naps supporting our hypothesis. We do not feel the patient was suffering from narcolepsy and/or cataplexy as no triggering events prior to her episodes could be found and she never describes a state of sleep paralysis. The REM sleep phase and physiology of atonia that occurs with REM sleep is well established and the rapidity of atonia onset during REM sleep lends a physiologic basis for our observations [10].
Certainly, one could argue that her use of ropinirole as dopamine agonists have been described to induce similar sleep attacks in patients taking ropinirole and in Parkinson’s Disease patients when taking carbidopa-levodopa [6,7]. However, our patient’s dose of ropinirole had been stable for years without any increases that correlated to her increased sleep attacks. Additionally, her ropinirole was continued during her treatment with NIPPV and her frequency of sleep attacks decreased despite her continuing use of ropinirole.
Others have published similar findings showing that chronic sleep deprivation can lead to increased falls by inducing micro-sleeps with atonia [8,9]. Interestingly, Helbig et al showed that in addition to sleep deprivation, excessive sleep in the elderly can also lead to increased falls. Clearly, sleep disturbances in the elderly have adverse effects on their health quality that can lead to increased risk of falls thereby increasing their risk of hospital stays and risk of serious injury. Oftentimes, when these patients are seen in the hospital, we focus on organic causes and forget to ask about sleep hygiene. This could potentially lead to recurrent falls with frequent hospitalizations as the underlying cause remains untreated. Therefore, by simply taking a sleep history on a patient presenting with falls focusing on their sleep/awake patterns and nap behavior could help improve diagnostic accuracy and lead to implementing simple and effective treatment recommendations.
Work was performed at Overland Park Medical Center. This manuscript has been read, edited, and approved by all of the authors listed.
We have no conflicts of interest and this project was not funded by any source. This case was not part of a clinical trial. This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Citation: Nelson JB, Anderson M, Remmers N (2021) Chronic sleep deprivation in a 75-year-old female leading to increased falls and a daytime microsleeps. J Sleep Disord Ther 10:329.
Received: 27-Jun-2021 Accepted: 21-Jul-2021 Published: 28-Jul-2021 , DOI: 10.35248/2167-0277.21.10.329
Copyright: ©2021 Nelson JB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.