International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Commentary - (2020)Volume 8, Issue 7
Ankle stabilization procedures represent an established surgical option for patients suffering from chronic ankle instability (CAI) not responding to conservative treatment [1]. Recent times have witnessed the development of a new arthroscopic approach, mirroring what already occurred in the shoulder and knee joints, where original open stabilization techniques have progressively been replaced by all arthroscopic solutions (Figure 1) [2].
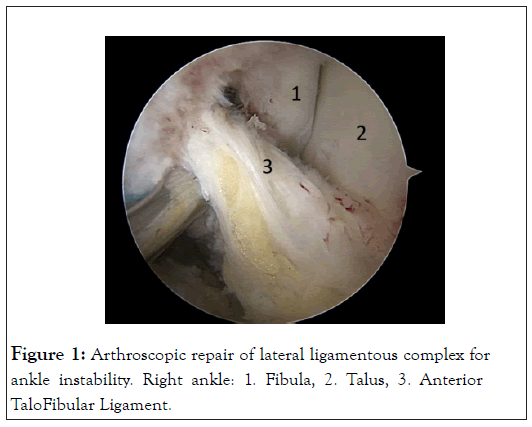
Figure 1: Arthroscopic repair of lateral ligamentous complex for ankle instability. Right ankle: 1. Fibula, 2. Talus, 3. Anterior TaloFibular Ligament.
Successful results are similarly reported in association with both the most recent and previous techniques [3]. Yet, a careful analysis of the published data encourages further reflections about the current ability to evaluate the clinical relevance of the most recent advancements. When it comes to evaluate the effectiveness of any medical intervention and the acceptance of new techniques in the clinical practice the choice of the proper outcome tool is mandatory. It is a matter of selecting “the right tool for the job”, which requires consideration of who and what is being measured, and why.
It has long been recognized that the direct patient’s perspective on their experiences with treatment, through the use of the patient-reported outcome tools (PROs), is the most important evidence to evaluate the effectiveness of a clinical intervention. As simple as it is, value should always be defined around the customer.
The PROs are considered appropriate in assessing orthopedic outcomes if they are psychometrically sound, meaning that the tools have shown to be valid, reliable and able to detect posttreatment changes in the specific population affected by the disease of interest [4].
With this premises in mind Spennacchio et al. have systematically analyzed the literature published from to 2004 to 2018 to furnish a comprehensive overview of the evaluation modalities chosen by the researchers dealing with the surgical treatment of ankle instability [5]. In the authors’ mind such an analysis would be the first step to define the critical points in the current CAI evaluation ability, at the same suggesting area worthy of future investigation.
The results of the review confirm indeed that researchers’ choice are not always accordant with the available evidence. The AOFAS ankle/hindfoot scale [6] resulted the most frequently reported outcome score across the 104 included studies. The AOFAS is a clinician-based score never been evaluated for validity and reliability to assess ankle instability. Little emphasis on joint stability make it possible to rate the maximum score even in the event of a postoperative persistent subjective feeling of instability [7]. It could then be argued that AOFAS outcome data may suggest greater success than justified. In an official statement in 2018 the American Orthopedic Foot and Ankle Society reiterated that the AOFAS scale has insufficient psychometric properties to justify its use in clinical research [8]. However, the statistical frequency of use of the scale in clinical practice seems to represent a strong support, since the most recent consensus statements keep on recommending its use to evaluate CAI surgical treatment [9].
As a matter of fact, only a minor part of the literature dealing with CAI surgical treatment describes the postoperative results through outcome scales with some proofs of validity in the specific CAI population, namely the Karlsson score, the Foot and Ankle Ability Measure (FAAM) and the Foot and Ankle Outcome Score (FAOS) [10,11]. Nevertheless, the FAAM and FAOS original development as generic foot and ankle scales questions their specificity for symptoms of ankle instability that may be the main cause of disability in the unique CAI population.
Another evident concerning point highlighted by the review relates to the preoperative diagnostic criteria leading to an ankle stabilization procedure. Researchers define ankle instability in a varied manner, using different combinations of patient’s history, subjective symptoms, physical examination signs and imaging evaluations. It could be argued that the common point across the studies dealing with CAI surgical treatment is the stabilization procedure rather than the treated disease, with negative impact on the external validity of the reported findings and a reliable comparison across studies. The need for a standardized patient’s selection is particularly topical considering emerging theories about the ankle micro instability [12], or the recent renewed interest toward the clinical role of the medial ligamentous complex of the ankle [13]. An agreed definition of these diagnostic hypothesis within the heterogenous CAI population would be extremely important to increase the reliability of the evidence supporting both their clinical relevance and the proposed treatment.
Already In 2014, the International Ankle Consortium endorsed several criteria to define a more homogeneous cohorts of patients suffering from ankle instability [14]. The experts agreed that the clinical diagnosis of CAI should be confirmed with a validated discriminative ankle instability questionnaire in controlled research, recommending at that time the use of the Cumberland Ankle Instability Tool (CAIT) [15]. However, these recommendations seem to be disregarded by the researchers’ community, as witnessed by the scarce if not absent use of validated scales to define the preoperative ankle status in the literature dealing with CAI treatment.
An increased interest in ankle instability and its arthroscopic approach has been observed in the last few years, which allowed to describe new pathologic entities with the exciting potential to increase the quality of the clinical practice [12]. For this to become real it is of utmost importance to improve our ability to evaluate the effectiveness of the proposed therapeutic algorithm. Standardized diagnosis, the evidence-based selection of the evaluation modalities, and additional knowledge on the clinimetric properties of PROs represent necessary steps to afford further insight of ankle instability, and provide our patients with the best possible practice.
Citation: Spennacchio P (2020) Chronic Ankle Instability Treatment: Is the Current Outcome Evaluation Appropriate? Int J Phys Med Rehabil.8:576.
Received: 13-Oct-2020 Accepted: 27-Oct-2020 Published: 03-Nov-2020 , DOI: 10.35248/2329-9096.20.8.576
Copyright: © 2020 Spennacchio P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.