Journal of Applied Pharmacy
Open Access
ISSN: 1920-4159
ISSN: 1920-4159
Review Article - (2024)Volume 16, Issue 3
Much of the world is mired in a pandemic caused by the spread of COVID-19. Healthcare facilities and research laboratories are intensely interested in developing processes and protocols to safely reopen in situations where adequate social distancing may not be possible. In a large, experimental chemistry and materials science research laboratory, graduate students, post-docs, undergrads, staff scientists and administrative personnel work very closely together. Social distancing is a challenge when much of the work involves complex machinery, specialized analytical devices, limited space and collaborative bench work that is hard to physically separate. A similar dynamic exists in medical offices, hospitals and Ambulatory Surgery Centers (ASCs). As we have searched for strategies in addition to social distancing that would enable a safe and gradual re-opening, it is clear that Personal Protective Equipment (PPE) has a primary role. Chemists in particular are very familiar with PPE as they are required to wear lab coats, safety glasses and gloves in synthetic labs. Other types of PPE are routinely used when dealing with potentially noxious reaction processes. Physicians, due to close, sustained contact with patients are now routinely donning PPE in situations where it was never previously required. But what is to be done when every person and every process could potentially expose our ourselves and our staff to transmission risk of COVID -19? As we have recently learned, asymptomatic individuals could be actively infected with high viral loads in the nose and mouth with the potential to transmit infectious virus particles through aerosols, droplets and other dispersive elements.
COVID-19; Aerosols; Protective equipment; Ambulatory surgery centers
It is now clear that although PPE is important, it is not enough. In fact, what we have found is that chemical antisepsis seems to have a critical role. Povidone-Iodine (PVP-I), at concentrations low enough to be safely administered to the sites of high viral shedding in the mouth and nose, is emerging as a potentially useful nasal and oral antiseptic. There is ample support for the rapid antiviral efficacy and for the safety of PVP-I at concentrations below about 2.0%. Most PVP-I solutions commercially available in the US are in the 5%-10% concentration range, though newer products such as halodine nasal antiseptic and halodine oral rinse (Halodine LLC, Spring house, PA) are specifically being manufactured and offered at low concentrations [1].
Reports of the efficacy and safety of PVP-I at low concentrations have led many physicians and clinicians to advocate for the simple dilution of commercially available 10% PVP-I solutions with water or saline to produce PVP-I in the 0.25%-1.5% concentration range. There is growing consensus that PVP-I in concentrations below 2.0% is a powerful adjunct to PPE, but the use of commercially available 10% PVP-I is unsafe for routine daily intranasal and intraoral use. The strategy of simple dilution poses some risks based on chemical differences and equilibrium changes that could occur when diluting 10% commercial PVP-I to 0.5% “homemade” PVP-I in a doctor’s office, hospital or other clinical or pharmacy setting. Summarized below are some of the issues that should be considered when diluting commercial 10% PVP-I to lower concentrations for use with PPE as adjunct viral protection strategies.
The main question we sought to understand is, “What if I waterdown conventional 10% PVP-I to make ‘dilute’ PVP-I? Isn’t that the same thing?” The short answer here is, “No, a 10% PVP-I solution diluted down to 1% or 0.5% is not the same as a PVP-I solution manufactured at 1% or 0.5% [2]. There are some complicated reasons related to the instability that pH and ion concentration introduce into aqueous equilibrium iodine chemistry. There are also some uncomplicated reasons that are related to the unspecified inactive ingredients and variation in available iodine allowed by the US Pharmacopeia (USP) analytical standards which govern commercial PVP-I drug products. According to the USP standards, which are recognized by the FDA, a “10% PVP-I solution” can mean a lot of different things with many different chemical compositions and many different properties. Most importantly, commercial 10% PVP-I is almost never actually 10% PVP-I. The USP standard requires that a “topical povidone-iodine solution” is defined by the analytical range of the labeled iodine content. A 35% variation of measured iodine can still be labeled as “10% povidone-iodine solution.” The USP definition of “10% povidone-iodine solution” allows the solution to deliver anywhere between 85% and 120% of the labeled iodine concentration.
“Povidone-iodine topical solution is a solution of povidoneiodine. It contains not less than 85.0 percent and not more than 120.0 percent of the labeled amount of Iodine (I). It may contain a small amount of alcohol.”
Note also that the USP allows a “small amount of alcohol.” This means that any topical PVP-I solution could contain alcohol, even if says “alcohol-free” on the label. If alcohol does appear on the label, as it does in many conventional PVP-I products, the USP allows the amount of alcohol to vary by up to 20% [3]. So just based on the allowed variance in the USP standards, when you try to make a specific concentration of PVP-I starting from conventional 10% PVP-I, it is impossible to make the target concentration. Without the capacity to perform analytical chemistry on the labeled “10% PVP-I” at the time of dilution, and without the ability to subsequently analyze the target dilution, it is impossible to make a specific low-concentration PVP-I.
After the variance allowed in the iodine content, consider the allowed variation in solvent and solute content. It is not required that a “10% povidone-iodine” solution have a specific solvent content or solute content. Think of it like 80 proof vodka, 80 proof whiskey and 80 proof gin: All of these solutions are 40% ethanol but none of them are the same. All one can say about them is, “they all have the same ethanol concentration which is 40%.” This is similar to the situation with commercial 10% PVP-I. It could be purely aqueous, partially aqueous, alcoholic, oxygenated, halogenated, hydrocarbon the only restriction is on the USP limits for residual Volatile-Organic Compounds (VOCs) from the manufacturing process. There are no solute restrictions. The only claim about conventional 10% PVP-I topical solutions that can be made is, “they all have the same PVP-I concentration, which is labeled at 10%, but actually could be anywhere from 8.5% to 12%.”
Commercial PVP-I often contains salts, counterions, detergents, penetration enhancers, preservatives, alkalinizing agents, acidifying agents, surfactants, buffers, additional iodophors, macromolecules, soaps, disintegrants, lubricants and other inactive excipients that may be required dependent on the intended application site or packaging requirements. The effectiveness, utility and toxicity of any excipient will be dependent on concentration and could be worse at higher dilutions. For example, if a 10% PVP-I solution with added surfactant is simply diluted, the concentration of the surfactant would be decreased. The aggregation and self-assembly of any given surfactant is determined by its critical micelle concentration, which is very sensitive to the concentration of the surfactant. Dilution could promote unintended surfactant assembly which could impair mucociliary clearance in the nose or cause unpredictable intolerance when used orally. Just from these qualitative explanations, it is easy to understand that a 10% PVP-I solution diluted down to a lower concentration is not the same as a PVP-I solution manufactured at a lower concentration. When we consider the complicated chemistry of iodine in these solutions, the arguments against dilution become even more compelling.
Commercial PVP-I is sold at high concentration usually 10% because low concentrations are very unstable when packaged in commercial polymer material container systems. Because the conventional PVP-I product concentrations are so high, typically chemical buffers are added to prevent tissue irritation when applied to patients. Buffers are also added to maintain the pH of the commercial solutions in the range required by the USP analytical standards [4]. The Buffering Capacity (β) of a solution is governed by the concentration of the protons and the concentration of the Conjugate Base Of The Buffer (CB), which are governed by the Ka of the acid used in the buffer system:
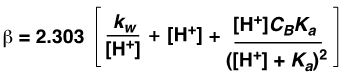
When commercial PVP-I at 10% is diluted with water or saline, it continues to have significant buffering capacity as the formula above clearly indicates. This causes the relative pH of the lowconcentration PVP-I to be maintained at the same elevated level as in the commercial undiluted PVP-I product. Normally, this would not be a problem for a conventional pharmaceutical product. But for PVP-I solutions, this is disastrous. PVP-I stability at low concentration requires an acidic environment. Alkaline or neutral conditions rapidly destabilize the iodine content in dilute solutions [5]. It has been well described for decades in the solution chemistry of PVP-I that buffered solutions of aqueous PVP-I are particularly unstable at low concentrations. The use of buffers in low-concentration PVP-I solutions must be strictly avoided. The instability arises from the aqueous solution equilibrium that is established at lowconcentrations for complexed and non-complexed iodine, iodide and triiodide as shown below.
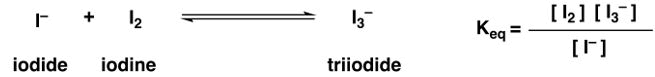
This condition, governed by the Equilibrium Constant (Keq), determines the relative and absolute concentrations of iodine, iodide and triiodide. The equilibrium constant Keq is exquisitely sensitive to temperature, pressure, container system, exposure to light, counterion, buffering capacity, osmolarity and most importantly, pH. To ensure stability, the solution components must be optimized to be in the most stable pH range for low concentrations of PVP-I which creates a favorable equilibrium. If commercial 10% PVP-I is diluted, the solution will maintain significant buffering capacity and will be buffered well outside the stable pH range [6]. Any freshly diluted solutions with residual buffering capacity will drive the unfavorable equilibrium reaction and rapidly result in solutions that are unstable, possibly toxic and rapidly ineffective. For dilution of commercial PVP-I to be safe and effective, upon dilution the residual buffering capacity would need to be immediately neutralized. This would be difficult to achieve without knowing the identity and quantity of the precedent solution’s acid buffer/conjugate base pair. The pH would need to be precisely and accurately measured, corrected with a standardized stock solution, ideally one specific for the buffer employed and then remeasured periodically throughout the day to ensure durable correction. Periodic analysis should also be carried out on freshly diluted PVP-I to monitor effects of temperature, pressure, light exposure, ion drift and container effects.
The pure aqueous solution equilibrium of PVP-I is additionally complicated by dilution if we consider the other equilibria associated with the iodine species in aqueous media [7]. Because water and protons are present in these equilibria reactions, the amount of iodine, iodide and triiodide will be critically dependent on all the factors described above and especially dependent on concentration and pH (Figure 1).
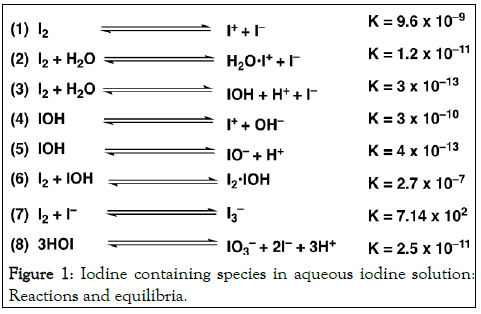
Figure 1: Iodine containing species in aqueous iodine solution: Reactions and equilibria.
The equilibria above are in idealized polymer-free, iodophor-free pure aqueous solutions of iodine. The simple iodine reactions above are further modified by polymer kinetics and polymer dynamics that we know are relevant when aqueous iodine is further complexed with the polyvinylpyrrolidone backbone (the “povidone” of “povidone-iodine”). Considering the reversible reaction with the polymer host leads to the well-known paradoxical concentration-dependent biocidal effects [8]. The figure below displays the chemical structure of the main species in solution when PVP-I is dissolved in water. This is a complex of H+I3– and adjacent residues on the PVP polymer (Figure 2).
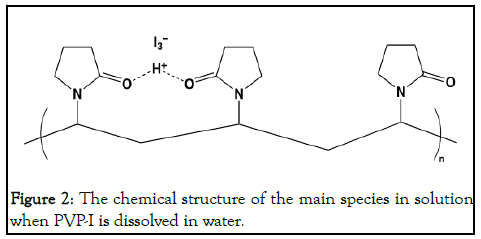
Figure 2: The chemical structure of the main species in solution when PVP-I is dissolved in water.
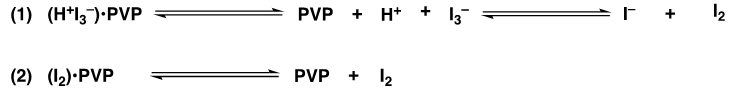
Even the chemical structure above is an oversimplification of the condition at any given concentration of PVP-I in aqueous solution. The equations below detail the two main complexes in PVP-I and their associated equilibria. Equation (1) is for the complex of H+I3- with PVP and equation (2) describes I2 complexed with PVP. When the complexes dissociate in aqueous solution, the iodine species enter the various equilibria with water, protons and other salts in solution. Simple dilution of commercial 10% PVP-I solutions will alter these equilibria in unpredictable ways. Each individual commercial PVP-I “recipe” will cause unique equilibrium changes with idiosyncratic results but predictable instability. When conventional 10% PVP-I is diluted, the buffers alone are enough to destabilize the target solutions, but all of the additives and excipients will also contribute to the disruption of the PVP-I solution equilibria [9].
There are osmotic consequences that come with dilution which are important in nasal physiology. Dilution of conventional high-concentration PVP-I solutions, without knowing the precise concentrations of all excipients, will result in solutions that are not isosmotic with nasal fluid. A PVP-I solution with a demonstrated osmolarity of ~300 mOsmol/kg of the dose intended for nasal application would be compatible with the osmotic conditions of the nasal secretions and the extracellular nasal mucosal space and ideal for intranasal use. If conventional 10% PVP-I is simply diluted with water or saline, it would be impossible to match the desired osmolarity without knowing the precise content and concentrations for all the potential additives delineated above. Even assuming there were minimal additives, matching the osmolarity would be almost impossible without some benchtop analytical chemistry available in the proposed setting of use. It would be difficult to adjust the osmolarity of the diluted PVP-I solution in a way that would allow rapid use in a clinical setting [10].
As described above, there is almost never a true “10% PVP-I “solution which means you can never reliably produce a precise target concentration through dilution. Uncertainty in the concentration is probably not critical when employed as a onetime application on intact skin, for example, in preparation for surgery. The imprecision does cause complications when used repeatedly on more sensitive mucosal surfaces. The uncertainty in the labeled PVP-I concentrations is further magnified by the uncertainty in the dilutional volumes. Unless the dilution is performed with volumetric glassware or other calibrated quantifiable addition and mixing vessels, the cascade of uncertainties in concentration, content and volume will lead to less predictable results when finally applied to patients. The only way to ensure the safety of these dilutions would be to analyze them prior to use [11]. Ideally, any target dilutions should be analyzed according to the USP method (USP 29-NF24, p1779). The preferred method for concentration of PVPI involves a thiosulfate reduction shown in the equation below.

The iodine is a golden brown color and when the thiosulfate is added, it reduces the iodine to iodide. As the titration progresses, when the solution becomes a light yellow, a starch solution is added to create a starch-iodine complex that is blue/ black in color. The titration continues until the solution turns colorless. The starch solution degrades quickly and would need to be made fresh prior to the analysis. Done correctly, the titration method requires flasks, burettes and other precision laboratory glassware, materials impractical to maintain in a clinical setting. Notwithstanding the inconvenience and cost of establishing the processes and procedures required to accurately determine the safety and composition of freshly diluted PVP-I solutions, a routine dilution program would require significant staff training or the addition of an additional staff member trained in analytical chemistry [12].
The simple on-site dilution of 10% PVP-I with water or saline solution to produce solutions in the 0.25%-2.0% range should be viewed with caution and undertaken only with the full appreciation of the risks detailed above.
Fortunately, in some laboratories, one would be able to employ diluted commercial solutions with the appropriate subsequent analysis, monitoring and storage conditions though this is inconvenient and impractical. PVP-I solutions manufactured and designed to be safe, stable and physiologically compatible in concentrations between 0.25%-2.5%, are preferred for repeated intraoral and intranasal use as chemical adjuncts to PPE.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Pelletier JS, Amoakohene SK, Nuckolls C (2024) Chemical Considerations Related to the Dilution of Commercial 10% Povidone- Iodine for Use in the COVID-19 Pandemic. J Appl Pharm. 16:419.
Received: 17-Jul-2020, Manuscript No. JAP-24-5418; Editor assigned: 21-Jul-2020, Pre QC No. JAP-24-5418 (PQ); Reviewed: 04-Aug-2020, QC No. JAP-24-5418; Revised: 01-Jun-2024, Manuscript No. JAP-24-5418 (R); Published: 28-Jun-2024 , DOI: 10.35248/1920-4159.24.16.419
Copyright: © 2022 Pelletier JS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.