Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research - (2020)Volume 9, Issue 4
Objective: To investigate the influence of the MRI-guided high-intensity focused ultrasound ablation (HIFU) of uterine fibroids on the endometrial receptivity in patients planning pregnancy.
Material and Methods: A prospective comparative controlled study of 95 reproductive age women planning a pregnancy with symptomatic uterine fibroids was conducted. 32 patients receiving HIFU treatment and 35 women receiving surgical treatment under laparoscopic myomectomy were examined. A control group was existing 28 healthy fertile women, examined voluntarily. The endometrium obtained with pipelle biopsia on days 20-22 of the menstrual cycle was examined by immunohistochemistry before and three months after the treatment. Statistical analysis of the results was carried out using SPSS 22.0.
Results: It was established that the focusing ultrasound rays passing through the endometrium do not cause changes in the maturation rate and do not affect the state of intercellular contacts. At the same time, a significant increase in the frequency of asynchronous maturation of pinopodia was found to be 50.00% (16) versus 14.28% (4); p=0.021 and the number of heteromorphic secretory cells 53.33% (8) versus 5.88% (1); p=0.002 in implantation endometrium.
Conclusions: The study did not reveal any significant negative effects of focused ultrasonic waves during FUSMRI ablation of uterine fibroids on endometrial receptivity in women of reproductive age. MRg HIFU ablation of uterine fibroids might be considered as an alternative treatment in patients of reproductive age with uterine fibroids planning a pregnancy.
Content: A prospective comparative controlled study of 95 women planning a pregnancy with symptomatic uterine fibroids, who received treatment by HIFU ablation and laparoscopic myomectomy.
Uterine fibroids; MRI-guided HIFU ablation; Laparoscopic myomectomy; Endometrium; Pinopodia
Uterine fibroids are the most common benign pelvic tumor in women of reproductive age. According to various authors the frequency of uterine fibroids in women older than 30 years varies from 20 to 60%, and is detected in 80% of women according to pathological studies [1,2]. Uterine fibroids affect the quality of life of women. Symptomatic course of uterine fibroids, manifested by menorrhagia, pelvic pain, frequent urination, infertility, occurs in 20-25% of cases. The peak incidence of uterine myoma is in the late reproductive age of 35-45 years [2,3].
Uterine fibroids and infertility are combined in 1-2.4% of cases. The etiological role of uterine fibroids in impaired fertility and infertility is ambiguous, a number of researchers have established that from 5 to 10% of female infertility problems can be directly explained by the presence of fibroids [4,5].
Many different studies show, that the sub mucous form of uterine fibroids significantly reduces the probability of pregnancy not only in the population, but also when using resources of assisted reproductive technologies, while there are discussions among scientists regarding the negative impact of intramural uterine fibroids on reproductive function [6].
Results on changes in the endometrial receptivity in patients with uterine myoma after conservative regression treatment using MRI-guided high-intensity focused ultrasound ablation (HIFU) of uterine fibroids are few and contradictory.
Pinopodia are considered the most important structural marker of endometrial receptivity, the number of which is an important predictor of implantation. It has been established that in women with a moderate or insignificant number of pinopodia in the endometrium during the period of the “implantation window”, the probability of pregnancy is significantly reduced or impossible [7].
Various diseases and pathological conditions of the endometrium can lead to a disruption of the formation and changes in the morphofunctional properties of pinopodia and, as a result, to a violation of the receptivity of the endometrium [8].
Literature data on the effect of the HIFU ablation of uterine fibroids on the morphofunctional and ultrastructural characteristics of the endometrium in patients of reproductive age compared with surgical methods for the treatment of uterine fibroids (laparoscopic myomectomy) are few and very contradictory.
In the literature does not cover the data in the context of a comparative analysis of the effect of focused ultrasound energy on the endometrium depending on the location of uterine fibroids along the anterior or posterior wall, which suggests a transient or surface effect of ultrasonic waves on tissues.
To investigate the influence of the MRI-guided high-intensity focused ultrasound ablation (HIFU) of uterine fibroids on the endometrial receptivity in patients planning pregnancy.
A prospective comparative cohort study was conducted that included 95 women of reproductive age planning a pregnancy. The main group included 32 women with symptomatic uterine fibroids, who received treatment using HIFU ablation. The comparison group included of 35 women with a symptomatic uterine fibroids, who received surgical treatment in the amount of laparoscopic myomectomy.
The control group consisted of 28 healthy fertile women’s who did not have a history of miscarriage, had a history of urgent delivery through the natural birth canal without deviating from the physiological course of pregnancy and the birth certificate, ending in the birth of healthy children.
In order to conduct a comparative analysis of the direct penetrating and indirect effects of the energy of ultrasonic waves on the endometrium, patients of the main group treated using HIFU ablation were divided into two additional groups.
Subgroup A- 15 patients with localization of the dominant myoma node along the posterior wall of the uterus, where focused ultrasound energy has a direct penetrating effect; Subgroup B- 17 patients with localization of the dominant myoma node along the front wall of the uterus, where focused ultrasound energy has a surface indirect effect on the tissue.
Criteria for inclusion in the study at the screening stage:
1. Reproductive age (18-45 years)
2. The presence of symptomatic uterine fibroids (complaints of menorrhagia, pain, infertility, dysfunction of the pelvic organs)
3. Localization of fibroids: interstitial, interstitial-subserous, interstitial with centripital growth (type 2-5 node according to FIGO classification (2011)
4. Sizes of knots from 4 to 9 cm
5. The ovulatory cycle
6. Informed voluntary consent of the patient or her legal representative to participate in the study.
Criteria for uterine fibroids, optimal for MR-guided HIFU ablation:
1. The sizes of myoma nodes from 4 to 9 cm
2. The number of nodes less than three
3. Interstitial component no less 30%
4. MR-type of signal-hypo-intense according to T2-VI: histotype typical uterine fibroids
5. Accessibility of all departments of the site for the procedure
Surgical treatment was performed by laparoscopic access under endotracheal anesthesia, using equipment and instruments of Karl Storz (Germany). The suturing of the bed of the myoma was performed using the technique of layer-by-layer suturing with separate sutures of absorbable material. Myoma nodes were removed from the abdominal cavity by morcellation in the Endobag system (Germany).
In the observation groups before treatment and 3 months after the MRI-guided HIFU ablation of uterine fibroids or laparoscopic myomectomy, a study of the endometrium obtained by pipellebiopsia was performed on days 20-22 of the menstrual cycle during the period of the alleged “implantation window”.
Endometrial biopsies were examined using light (survey) microscopy. Materials of endometrial biopsy specimens for histological examination were fixed in 10% neutral formalin, embedded in paraffin, sections were made 5 μm thick and stained with hematoxylin and eosin. Microscopic examination was performed on a Carl Zeiss Primo Star microscope.
By histological examination it was evaluated the structure of the endometrium (the state of the stroma, glandular apparatus, the correspondence of the endometrium to the phase of the menstrual cycle, the development of the vessels of the endometrial stroma).
The obtained endometrial samples were evaluated using scanning electron microscopy. For research in a transmission electron microscope, the endometrium was centrifuged for 30 min at 37°C with a 2.5% solution of glutaraldehyde in 0.1M phosphate buffer (pH 7.2). Glutaraldehyde was added in a ratio of 20:1. Centrifugation was carried out for 15 min at 1000 rpm. The supernatant was removed, 1-2 ml of glutaraldehyde was added to the precipitate. Fixation lasted from 60 minutes to 7 days (Holstein, Roosen-Runge, 1981). Further, the material was washed with phosphate buffer, fixed with 1% osmic acid on phosphate buffer, dehydrated in a series of alcohols (50°-5 min, saturated solution of uranyl acetate in 70° alcohol-12-14 hours, 96° alcohol-1 hour, 100°-1 hour, absolute acetone-30 min). Pouring was carried out in an epon-araldite mixture (Mollenhauer, 1964) after preliminary impregnation in 3 mixtures of epoxy resin and acetone (1:2, 1:1, 2:1) for 1 hour at 20°C. The polymerization was carried out 24 hours at 37°C and 24 hours at 56°C. Ultrathin sections were obtained on an UltraCutl 11 ultra-microtome, stained with lead citrate (Mi Honig, 1961) and studied using a JEM 100S electron microscope. For research using a scanning electron microscope, a part of the material after dehydration was dried at the critical sublimation point of carbon dioxide and examined in a Hitachi-S350 scanning electron microscope, Japan. The presence of pinopodia, the degree of their development in accordance with the phase of the menstrual cycle, the state of secretory cells, the morphology of ciliary cells, and the size of intercellular contacts were evaluated.
Statistical analysis of the results was carried out using the programs SPSS 16.0, SPSS: An IBM Company (USA) and Statistica 10.0, StatSoft (USA). The results of the study were presented as mean ± standard error of the mean (M ± m). The significance of differences in the results was determined using a paired or unpaired student t-test and Wilcoxon's test. Correlation analysis was performed using the Spearman nonparametric correlation criterion. Differences between statistical values were considered statistically significant at a confidence level of p<0.05.
According to the results of the studies, the average age of the group observation patients did not differ significantly and was presented in the main group 39.50 ± 1.33 years, in the comparison group 39.72 ± 1.39 years, in the control group 37.85 ± 1.43 (p>0.05). When analyzing the reproductive function of patients in the observation groups, it should be noted that the incidence of primary infertility was significantly higher in patients in the comparison group 11 (36.66%), versus 2 (7.4%) in the main group (p<0.05), while in the main group of patients, secondary infertility was significantly more likely to occur in 10 patients (37.03%), versus 4 patients (13.33%) in the comparison group; p<0.05.
Major factor in the occurrence of infertility in the observation groups was a combined factor that included a combination of tubalperitoneal and endocrine factors, which is 50.00% in the main group and 53.33% in the comparison group; (p>0.05). During the ultrasound examination, a single uterine myoma node was found in 17 women (65.96%) in the main group and in 11 women (36.67%) in the comparison group; and in 9 women (33.33%) of the main group and in 20 women (66.67%) of the comparison group, multiple uterine fibroids were revealed. There were no significant differences depending on the location of uterine fibroids along the anterior or posterior wall. The average size of the dominant myoma node before treatment ranged from 25.3 mm to 67.0 mm in the main group (average size of the dominant node 46.99 ± 13.25 mm), from 28.0 to 78.33 mm (average size of the dominant node 45.56 ± 14.78 mm) in the comparison group. The average volume of the dominant node averaged 127.39 ± 99.37 cm3 in the main group and 114.33 ± 102.18 cm3 in the comparison group.
Absorption of HIFU by tissues of uterine fibroids in 84.38 % of cases was complete. The non-perfused volume ratio (NPVR) of treated fibroids was 86.4 ± 7.8%.
According to the results of the initial histological examination, the endometrial picture in patients of reproductive age with uterine fibroids on the 20-22 day of the menstrual cycle was represented by tissue with a relatively uniform distribution of mainly convoluted or slightly convoluted glands, with even apical edges and sub nuclear vacuoles, which corresponds to the middle stage of the secretion phase. In some parts of the glands, the apical margin was visualized with signs of secretion. The glands were lined with a multi-row epithelium with normochromic nuclei oriented mainly basally. Many endometrial samples of the main observation groups encountered single structures of the type “gland in gland” (Table 1). In the majority of endometrial samples, patients of the main observation groups suffering from symptomatic uterine fibroids showed a marked focal or diffuse edema of the stroma with small hemorrhages and tangles of thin-walled vessels (Figure 1).
| Features | Main group Patients with uterine fibroids (n=67) |
Control group Fertile healthy women (n=28) |
The significance level of differences, p | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| abs. | % | abs. | % | р | |
| The endometrium corresponds to the cycle phase | 51 | 89.47 | 22 | 81.48 | NS |
| Uniformity of distribution of glands in the endometrium | 39 | 68.42 | 22 | 81.48 | NS |
| Gland in gland | 40 | 70.17 | 0 | 0 | NS |
| Mostly convoluted glands | 49 | 85.96 | 24 | 85.71 | NS |
| Mostly straight glands or slightly convoluted | 10 | 17.54 | 4 | 14.29 | NS |
| Apocrine secretion in the lumen of the glands | 11 | 19.29 | 6 | 21.43 | NS |
| Glands in the middle stage of the proliferation phase | 5 | 8.77 | 2 | 7.40 | NS |
| Glands in the phase of early-middle secretion | 3 | 5.26 | 8 | 29.63 | р=0.003 |
| Glands in the middle secretion phase | 40 | 70.17 | 18 | 66.66 | NS |
| Glands in the phase of middle-late secretion | 4 | 7.01 | 2 | 7.40 | NS |
| Glands in the late secretion phase | 5 | 8.77 | 0 | 0 | NS |
| Focal / diffuse stroma edema | 47 | 82.45 | 1 | 3.57 | р=0.001 |
| Endometrial hyperplasia | 12 | 21.05 | 3 | 10.71 | NS |
| Polyps | 10 | 17.54 | 5 | 18.52 | NS |
| Signs of chronic endometritis | 6 | 10.52 | 2 | 7.40 | NS |
Table 1: Morphological structure of the endometrium in the observation groups before treatment on day 20-22 of the menstrual cycle,%.
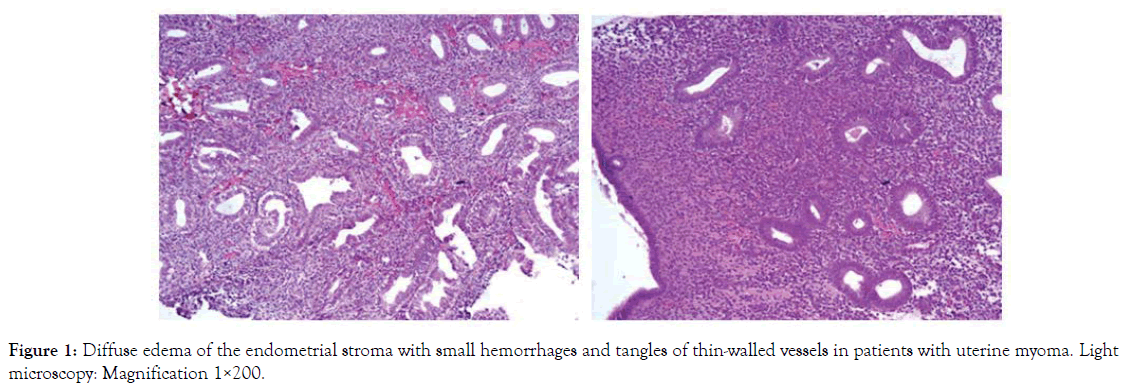
Figure 1. Diffuse edema of the endometrial stroma with small hemorrhages and tangles of thin-walled vessels in patients with uterine myoma. Light microscopy: Magnification 1×200.
In the study of endometrial biopsy samples, it was found that in the majority of the obtained samples, the endometrium corresponded to the middle stage of the secretion phase, 89.47%, in the control group it was 81.48%; p>0.05. At the same time, a relatively uniform distribution of glands in the stroma was noted both in women with uterine fibroids in 68.42% cases, and in patients of the control group-81.48%, p>0.05 (Table 1).
Significantly more often in the endometrium of patients with uterine fibroids, focal or diffuse edema of the stroma was found-82.45%, in the control group-3.57% p=0.001. There were no significant differences in the frequency of occurrence of pathological processes of the endometrium, such as endometrial hyperplasia, endometrial polyp, signs of chronic endometritis, in the study groups, p>0.05 (Table 1).
The study of endometrial samples using scanning electron microscopy (SEM) in the observation groups during the "implantation window" revealed a significantly lower incidence of mature pinopodia in patients with uterine fibroids (Figure 2) in 32.83% of samples in the group with uterine fibroids versus 71.42% in the control group p=0.004 (Table 2, Figure 3).
| Features | Patients with uterine fibroids before treatment (n=67) | Control group (n=28) |
x2 | Significance level, р | |
|---|---|---|---|---|---|
| 1 | The "calm" epithelium | 32.83% | 14.28% | 2.870 | NS |
| 22 | 4 | ||||
| 2 | Secretory cells in the formation stage pinopode | 46.27% | 10.71% | 9.035 | р=0.003 |
| 31 | 3 | ||||
| 3 | Maturing pinopodia | 43.28% | 21.42% | 3.155 | NS |
| 29 | 6 | ||||
| 4 | Mature pinopodia | 32.83% | 71.42% | 8.417 | р=0.004 |
| 22 | 20 | ||||
| 5 | Asynchronous maturation of pinopodia | 23.88% | 14.28% | 0.078 | NS |
| 16 | 4 | ||||
| 6 | Saved intercellular contacts | 37.31% | 7.14% | 7.259 | р=0.008 |
| 25 | 2 | ||||
| 7 | Disconnected intercellular contacts | 62.69% | 86.67% | 7.259 | р=0.008 |
| 42 | 26 | ||||
| 8 | Atypical ciliated cells | 86.57% | 7.14% | 36.679 | р<0.001 |
| 58 | 2 | ||||
| 9 | Secretory granules | 5.97% | 92.85% | 43.087 | р<0.001 |
| 4 | 26 |
Table 2: Ultra structural morphological picture of the endometrium during the "implantation window" in women with uterine fibroids.
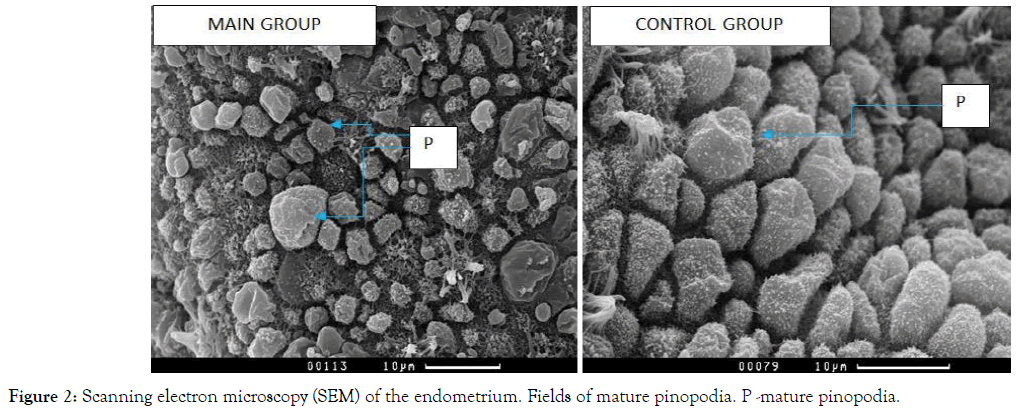
Figure 2. Scanning electron microscopy (SEM) of the endometrium. Fields of mature pinopodia. P -mature pinopodia.
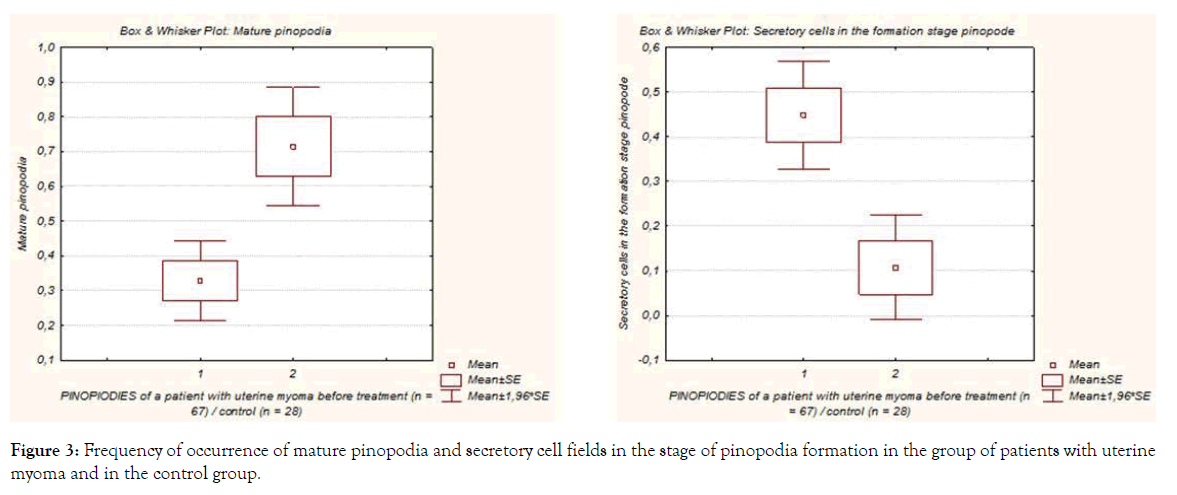
Figure 3. Frequency of occurrence of mature pinopodia and secretory cell fields in the stage of pinopodia formation in the group of patients with uterine myoma and in the control group.
The characteristic of the endometrium during the supposed "implantation window" in patients with uterine myoma differed significantly higher frequency of occurrence of secretory cell zones in preparation for the formation of pinopodia. The pinopodia themselves lagged significantly behind similar parameters in the control group in terms of their density and height (Figure 2). Thus, there was a certain chronometric lag in the patient with uterine myoma. The secretory cells were domed with thickened microvilli, and the ciliated cells were partially recessed relative to the surface of the secretory cells (Figure 4). Secretory cells in preparation for the formation of pinopodia were found in 31 endometrial samples in patients with myoma (46.27%) versus 3(10.71%) in the control group (p=0.003). The presence of atypical ciliated cells was noted in 58 endometrial samples (86.57%) of women with uterine fibroids, which is significantly higher than in the endometrial samples of the control group-2 (7.14%) (p<0.001) (Figure 4).
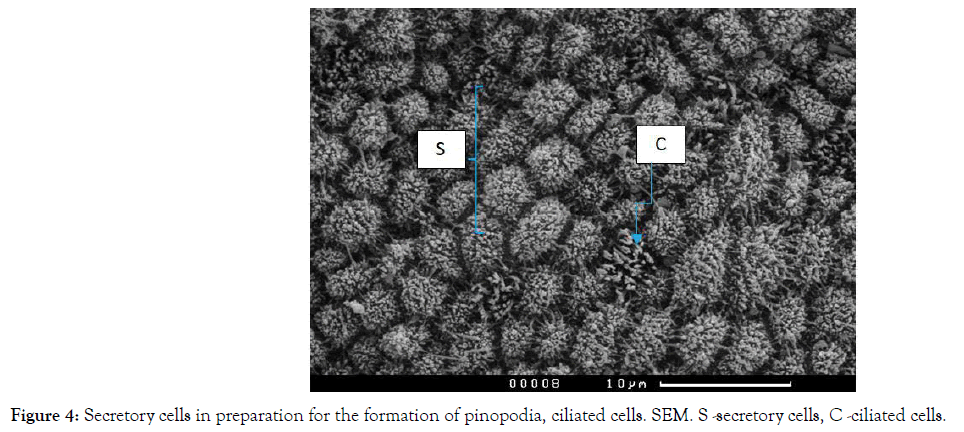
Figure 4. Secretory cells in preparation for the formation of pinopodia, ciliated cells. SEM. S -secretory cells, C -ciliated cells.
The characteristic of endometrial samples during the "implantation window" was significantly lower in the incidence of secretory granules on the cell surface in patients with uterine fibroids than in the control group in 4 cases (5.97%) versus 25 (91.85%) in the control group p<0.001 (Figure 5).
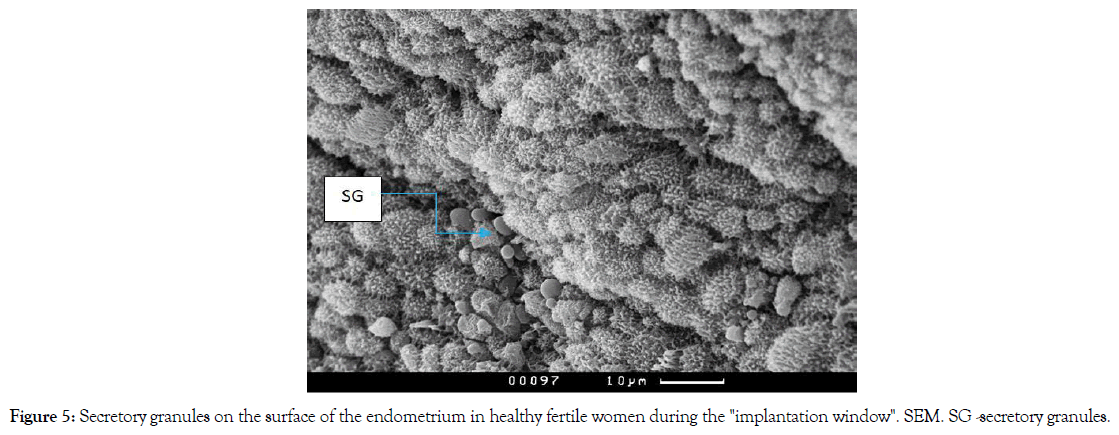
Figure 5. Secretory granules on the surface of the endometrium in healthy fertile women during the "implantation window". SEM. SG -secretory granules.
The frequency of dissociation of intercellular contacts in the samples of the "implantation" endometrium is a necessary condition for successful implantation of the blastocyst and trophoblast invasion. A significantly higher incidence of dissociation of intercellular contacts in the “implantation” endometrium of fertile healthy women was revealed 86.67% versus 62.69% in the comparison group; p=0.008 (Figure 6).
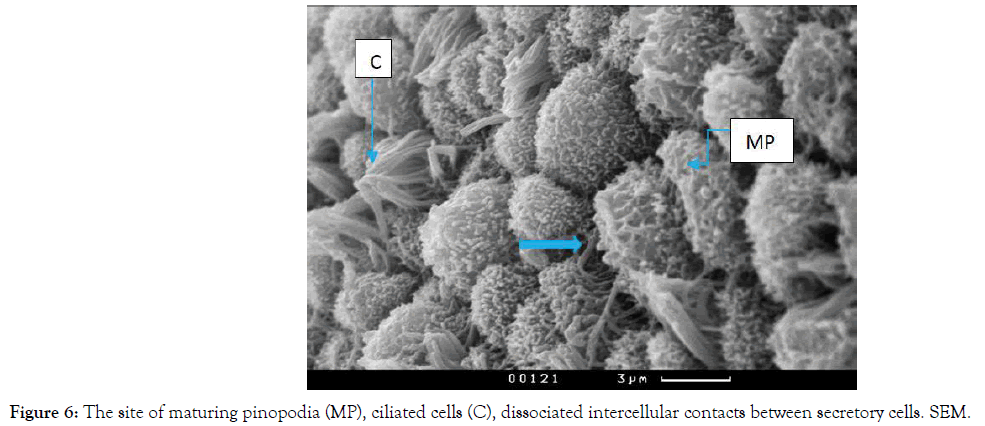
Figure 6. The site of maturing pinopodia (MP), ciliated cells (C), dissociated intercellular contacts between secretory cells. SEM.
A comparative analysis of ultra-structural picture of the "implantation" endometrium in the dynamics of treatment use of MRI-guided HIFU ablation of uterine fibroids was carried out. In the study of endometrial samples by scanning electron microscopy (SEM) in patients with uterine fibroids by the dynamics of treatment use of MRI-guided HIFU ablation, a significant decrease in the frequency of occurrence of mature pinopodes fields was revealed 68.75% cases, compared with the indicators before treatment in 93.75% cases, p=0.024, due to the increase in the frequency of occurrence of mature pinopodes fields after MRI-guided HIFU ablation and, as a consequence, the absence of significant differences in the frequency of occurrence of mature pinopodes in endometrial samples after treatment of uterine fibroids compared with the control group: after treatment 59.38%, against 71.42% in the control group, p>0.05, which may indicate improvement of ultra-structural predictors of implantation during treatment (Table 3). At the same time, after MRI-guided HIFU ablation in the endometrium, there was a significantly higher frequency of asynchronous maturation of pinopodia observed in 50.00% of observations compared with 14.28% of control group samples, and a significantly higher frequency of heteromorphic secretory cells in 28.13%, versus 0% in the control group (Table 3). There were no significant differences in these indicators in the dynamics of treatment. Since the total prevalence of maturing and mature pinopodia after MRI-guided HIFU ablation did not significantly change, there were no significant differences in the nature of intercellular contacts. The frequency of detection of separated and dense contacts in endometrial samples did not differ statistically significantly (Table 3).
| No. | Features | Units | The main group before HIFU (n=32) |
The main group after HIFU (n=32) |
Control group (n=28) |
OR [Cl 95%] |
x2 / р | Significance level, x2 / р1-2 (McNemar's chi-square test) |
|
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | x2 / р1-3 | x2 / р2-3 | |||||
| 1 | The "calm" epithelium | % | 34.37% | 18.75% | 14.28% | OR1-2= 2.270 [0.719-7.161] OR1-3= 3.143 [0.869-11.367] OR2-3= 1.385 [0.348-5.512] |
0.0840* | 0.7375** | 0.532 |
| абс. | 11 | 6 | 4 | р=0.073 | р=0.644 | р=0.466 | |||
| 2 | Maturing pinopodia | % | 93.75% | 68.75% | 21.42% | OR1-2= 6.818 [1.356-34.275] OR1-3= 55.000 [10.126-298.745] OR2-3= 8.067 [2.499-26.044] |
29.601* | 11.602* | 16.667 |
| абс. | 30 | 22 | 6 | р <0.001 | р <0.001 | р <0.001 | |||
| 3 | Mature pinopodia | % | 31.25% | 59.38% | 71.42% | OR1-2= 0.311 [0.111-0.869] OR1-3= 0.182 [0.060-0.551] OR2-3= 0.585 [0.198-1.724] |
9.643 | 0.954 | 2.314 |
| абс. | 10 | 19 | 20 | р=0.002 | р=0.329 | р=0.129 | |||
| 4 | Asynchronous maturation of pinopodia | % | 62.50% | 50.0% | 14.28% | OR1-2= 1.667 [0.615-4.513] OR1-3= 10.000 [2.787-35.886] OR2-3= 6.000 [1.693-21.262] |
0.0041** | 0.0114** | 0.571 |
| абс. | 20 | 16 | 4 | р<0.001 | р=0.004 | р=0.450 | |||
| 5 | Heteromorphic secretory cells | % | 34.37% | 28.13% | 0% | OR1-2= 1.339 [0.463-3.868] | 11.786 | 9.265 | 0.209* |
| абс. | 11 | 9 | 0 | р<0.001 | р=0.003 | р=0.648 | |||
| 6 | Saved intercellular contacts | % | 37.50% | 21.88% | 7.14% | OR1-2= 2.143 [0.712-6.451] OR1-3= 7.800 [1.565-38.885] OR2-3= 6.640 [0.689-19.233] |
0.00645** | 0.15481** | 1.8718** |
| абс. | 12 | 7 | 2 | р=0.006 | р=0.111 | р=0.172 | |||
| 7 | Disconnected intercellular contacts | % | 62.50% | 78.12% | 86.67% | OR1-2= 0.467 [0.155-1.405] OR1-3= 1.128 [0.026-0.639] OR2-3= 0.275 [0.052-1.452] |
7.693 | 2.542 | 1.871 |
| абс. | 20 | 25 | 26 | р=0.006 | р=0.111 | р=0.172 | |||
| 8 | Atypical ciliated cells | % | 53.13% | 15.63% | 7.14% | OR1-2= 6.120 [1.880-19.919] OR1-3= 14.733 [2.983-72.761] OR2-3= 2.407 [0.428-13.525] |
8.381* | 0.43201** | 4.513** |
| абс. | 17 | 5 | 2 | р=0.034 | р=0.308 | р=0.034 | |||
| 9 | Secretory granules | % | 15.63% | 62.5% | 92.85% | OR1-2= 0.111 [0.034-0.366] OR1-3= 0.014 [0.003-0.080] OR2-3= 0.128 [0.026-0.639] |
35.669* | 52.437 | 5.469* |
| абс. | 5 | 20 | 26 | р<0.001 | р<0.001 | р=0.017 | |||
Table 3: Ultra structural morphological picture of the endometrium during the "implantation window" in women with uterine fibroids before and 3 months after treatment with MRI-guided HIFU ablation of uterine fibroids.
Noteworthy is a significant decrease in the incidence of atypical ciliated cells in endometrial samples of the main group in the dynamics of treatment from 53.13% to 15.63%(5); p=0.026 and a statistically significant increase in the frequency of verification of secretory granules on the cell surface after treatment from 15.63% to 62.5%; p=0.017 due to some increase in the incidence of disconnected intercellular contacts (Table 3).
Three months after laparoscopic myomectomy has improved some indicators of endometrial receptivity. Thus, there was a significant decrease in the frequency of verification of endometrial samples with epithelium of "calm" type without signs of pinopodes maturation and dense intercellular contacts from 34.29% to 20.00%; p=0.005. There were no significant changes in the rate of pinopodes maturation and the structure of their degree of maturity after surgical treatment (Table 4). The frequency of verification of mature and maturing pinopodia in the "implantation" endometrium did not significantly change after surgical treatment and statistically significantly differed from the control values (Table 4). Thus, in patients with uterine fibroids, the number of endometrial samples with maturing pinopodia during the "implantation window" was significantly higher 88.57% than in fertile healthy women 21.42%; p<0.05, and the number of samples showing mature pinopodia 11.43%, on the contrary, significantly lower than the control values 71.42% throughout the observation period, regardless of surgical intervention.
| No. | Features | Units | Comparison group before myomectomy (n=35) |
Comparison group after myomectomy (n=35) | Сontrol group (n=28) |
OR [Cl 95%] |
x2 / р | Significance level, x2 / р1-2 (McNemar's chi-square test) |
|
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | x2 / р1-3 | x2 / р2-3 | |||||
| 1 | The "calm" epithelium | % | 34.29% | 20.00% | 14.28% | OR1-2= 2.087 [1.707-6.165] OR1-3= 3.130 [0.881-11.124] OR2-3= 1.500 [0.391-5.752] |
0.087** | 0.741** | 8.008* |
| абс. | 12 | 7 | 4 | р=0.065 | р=0.551 | р=0.005 | |||
| 2 | Maturing pinopodia | % | 94.29% | 88.57% | 21.42% | OR1-2= 2.129 [0.364-12.459] OR1-3= 60.50 [11.177-327.490] OR2-3= 28.417 [7.162-112.741] |
31.992* | 26.229* | 0.4361** |
| абс. | 33 | 31 | 6 | р<0.001 | р<0.001 | р=0.389 | |||
| 3 | Mature pinopodia | % | 25.71% | 11.43% | 71.42% | OR1-2= 2.683 [0.740-9.726] OR1-3= 0.138 [0.045-0.423] OR2-3= 0.052 [0.014-0.194] |
11.891* | 0.000** | 0.2196** |
| абс. | 9 | 4 | 20 | р<0.001 | р<0.001 | р=0.135 | |||
| 4 | Asynchronous maturation of pinopodia | % | 54.29% | 20.00% | 14.28% | OR1-2= 2.010 [1.275-3.168] OR1-3= 7.125 [2.041-24.871] OR2-3= 1.500 [0.391-5.752] |
0.001** | 0.741** | 6.612* |
| абс. | 19 | 7 | 4 | р=0.002 | р=0.551 | р=0.011 | |||
| 5 | Heteromorphic secretory cells | % | 34.29% | 34.43% | 0% | OR1-2=1.138 [0.420-3.089] | 11.859 | 10.662 | 0.021 |
| абс. | 12 | 11 | 0 | р<0.001 | р=0.002 | р=0.885 | |||
| 6 | Saved intercellular contacts | % | 37.14% | 28.57% | 7.14% | OR1-2= 1.477 [0.541-4.032] OR1-3= 7.682 [1.561-37.795] OR2-3= 5.200 [1.035-26.130] |
7.718 | 4.632 | 0.021 |
| абс. | 13 | 10 | 2 | р=0.006 | р=0.032 | р=0.885 | |||
| 7 | Disconnected intercellular contacts | % | 62.86% | 71.43% | 86.67% | OR1-2= 0.677 [0.248-1.847] OR1-3= 0.130 [0.026-0.640] OR2-3= 0.192 [0.038-1.966] |
7.718 | 0.051** | 3.789 |
| абс. | 22 | 25 | 26 | р=0.006 | р=0.132 | р=0.053 | |||
| 8 | Atypical ciliated cells | % | 54.29% | 8.57% | 7.14% | OR1-2= 12.667 [3.259-49.230] OR1-3= 15.438 [3.165-75.291] OR2-3= 1.219 [0.189-7.849] |
0.0001** | 1.000** | 8.224* |
| абс. | 19 | 3 | 2 | р<0.001 | р=0.835 | р=0.005 | |||
| 9 | Secretory granules | % | 14.28% | 51.43% | 92.85% | OR1-2= 0.157 [0.050-0.500] OR1-3= 0.013 [0.002-0.072] OR2-3= 0.081 [0.017-0.397] |
0.0001** | 0.0003** | 2.755* |
| абс. | 5 | 18 | 26 | р<0.001 | р<0.001 | р=0.084 | |||
Table 4: Ultra structural morphological picture of the endometrium during the "implantation window" in women with uterine myoma before and 3 months after laparoscopic myomectomy.
Positive changes in the ultra-structural pattern of the endometrium after laparoscopic myomectomy should be noted a significant decrease in the number of samples with asynchronous type of maturation pinopodes from 54.29% 20.00%; p=0.011, when the samples of endometrial pinopodes are present at different stages of maturation with uneven distribution on the surface epithelium of the glands, which hampers adequate adhesion of the blastocyst. The number of heteromorphic secretory cells did not significantly change after surgical treatment (Table 4).
Surgical treatment in the volume of myomectomy did not affect the state of intercellular contacts in the samples of the "implantation" endometrium.
The number of dense and disconnected contacts after surgery did not significantly change (Table 4), however, there was a tendency to increase the number of endometrial samples with disconnected intercellular contacts to a level statically indistinguishable from the control parameters: 71.43% in the comparison group against 86.67% in the control group; p>0.05.
After laparoscopic myomectomy, the frequency of verification of atypical cilia cells significantly decreased from 54.29% to 8.57%; p=0.005, which does not statistically exceed the control values of 7.14%; p>0.05.
Finally, the degree of secretion in endometrial cells after myomectomy increased due to increased verification on the surface of the epithelium of the "implantation" endometrium of secretory granules from 14.28% to 51.43%, but did not reach, however, the criteria of sufficiency, remaining statistically significantly below the control values of 92.85%; p<0.001.
In the comparative analysis of endometrial ultrastructure during the "implantation window” of patients with uterine myoma after treatment with MRI-guided HIFU ablation and laparoscopic myomectomy, attention is drawn to the significant excess of the frequency of verification of mature pinopodia in endometrial samples of women after MRI-guided HIFU ablation compared with myomectomy: 59.38% versus 11.43%; p<0.001. At the same time, the rate of detection of mature pinopodia in the samples of patients of the main group after treatment by MRI-guided HIFU ablation becomes statistically indistinguishable from the control indicators, respectively 59.38% in the main group against 71.42% in the control group; p>0.05.
It was revealed that the asynchrony of pinopodia maturation was significantly more pronounced in patients after treatment of uterine fibroids by MRI-guided HIFU ablation 50.00% versus 20,00% in the comparison group; p=0.021. This indicator in the main group significantly exceeded the control values of 14.28%; p=0.003, while after treatment with myomectomy, the reliability of differences with the control in the frequency of asynchronous maturation of pinopodia was lost 20.00% versus 14.28%; p>0.05. There were no statistical differences in the incidence of heteromorphic secretory cells in the observation groups, and both of these indicators significantly exceeded the control values (Table 5).
| No. | Features | Units | The main group after HIFU (n=32) |
Comparison group after myomectomy (n=35) | Сontrol group (n=28) |
OR [Cl 95%] |
x2 / р |
||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | x2 / р1-2 | x2 / р1-3 | x2 / р2-3 | ||||
| 1 | The "calm" epithelium | % | 18.75% | 20.00% | 14.28% | OR1-2= 0.923 [0.274-3.108] OR1-3= 1.385 [0.348-5.512] OR2-3= 1.500 [0.391-5.752] |
0.017 | 0.737** | 0.741** |
| абс. | 6 | 7 | 4 | р=0.898 | р=0.644 | р=0.553 | |||
| 2 | Maturing pinopodia | % | 68.75% | 88.57% | 21.42% | OR1-2= 0.284 [0.079-1.023] OR1-3= 8.067 [2.499-26.044] OR2-3= 28.41 [7.162-112.741] |
0.7053** | 15.595* | 0.0000** |
| абс. | 22 | 31 | 6 | р=0.306 | р<0.001 | р<0.001 | |||
| 3 | Mature pinopodia | % | 59.38% | 11.43% | 71.42% | OR1-2= 11.327 [3.220-39.844] OR1-3= 0.585 [0.198-1.724] OR2-3= 0.052 [0.014-0.194] |
0.0007* | 0.497 | 0.000** |
| абс. | 19 | 4 | 20 | р<0.001 | р=0.481 | р<0.001 | |||
| 4 | Asynchronous maturation of pinopodia | % | 50.00% | 20.00% | 14.28% | OR1-2= 4.000 [1.359-11.778] OR1-3= 6.000 [1.693-21.262] OR2-3= 0.516 [0.136-1.953] |
5.409* | 0.0055** | 0.7409** |
| абс. | 16 | 7 | 4 | р=0.021 | р=0.003 | р=0.551 | |||
| 5 | Heteromorphic secretory cells | % | 28.13% | 34.43% | 0% | OR1-2= 0.854 [0.299-2.411] | 0.001* | 0.0024** | 0.0007** |
| абс. | 9 | 11 | 0 | р=0.978 | р=0.008 | р=0.004 | |||
| 6 | Saved intercellular contacts | % | 21.88% | 28.57% | 7.14% | OR1-2= 0.700 [0.230-2.132] OR1-3= 6.640 [0.689-19.233] OR2-3= 5.200 [0.035-26.130] |
0.121** | 0.1548** | 0.0509** |
| абс. | 7 | 10 | 2 | р=0.728 | р=0.111 | р=0.320 | |||
| 7 | Disconnected intercellular contacts | % | 78.12% | 71.43% | 86.67% | OR1-2= 1.429 [0.469-4.351] OR1-3= 0.275 [0.052-1.452] OR2-3= 0.192 [0.038-0.966] |
0.121** | 0.1548** | 0.0509** |
| абс. | 25 | 25 | 26 | р=0.728 | р=0.111 | р=0.320 | |||
| 8 | Atypical ciliated cells | % | 15.63% | 8.57% | 7.14% | OR1-2= 1.975 [0.432-9.034] OR1-3= 2.407 [0.428-13.525] OR2-3= 1.219 [0.189-7.849] |
0.4321** | 1.000** | 0.4645** |
| абс. | 5 | 3 | 2 | р=0.516 | р=0.835 | р=0.609 | |||
| 9 | Secretory granules | % | 62.5% | 51.43% | 92.85% | OR1-2= 1.574 [0.593-4.175] OR1-3= 0.128 [0.026-0.639] OR2-3= 0.081 [0.017-0.397] |
0.835 | 0.0065** | 0.003** |
| абс. | 20 | 18 | 26 | р=0.361 | р=0.014 | р=0.002 | |||
Table 5: Ultra structural picture of the endometrium during the "implantation window" (LG7+) in women with uterine myoma after various treatments (MRI-guided HIFU ablation and laparoscopic myomectomy), OR, Cl 95%, x2, p.
It was found that the state of intercellular contacts, that is, the frequency of detection of dense contacts and disconnection of intercellular contacts, as well as the state of microenvironment cells does not depend on the type of treatment of uterine fibroids (Table 5).
The severity of endometrial gland secretion also had no significant differences in the main observation groups, which indicates that this indicator does not depend on the method of treatment of uterine fibroids (MRI-guided HIFU ablation or myomectomy). In both main observation groups, this indicator was significantly lower than the control values (Table 5).
In the study of the ultrastructural picture of the endometrium, there were no significant differences in the rates of maturation of pinopodia depending on the type of penetration of ultrasound energy into the uterus. The frequency of occurrence in the samples of "implantation" endometrium mature and maturing pinopode did not differ significantly, however, in patients with node placement at the anterior wall of the uterus at the level of the trends were higher frequency of mature pinopodes 77.78%, but 53.33% in the group of patients with the position of the node on the posterior wall, respectively, the frequency of maturing pinopode in samples of endometrium were as a tendency higher in patients with dorsally location of a node of 73.33% against 52.94% location of the node on the front wall. The frequency of occurrence in endometrial samples of "calm" epithelium without signs of pinopodia maturation did not depend significantly on the location of the node.
Revealed significantly higher frequency of asynchronous maturation pinopodes in patients with node placement at the posterior wall of the uterus 46.67% against 11.76% when the location of the node at the anterior wall; p=0,026, this may be explained by the penetrating effect of focused ultrasound on the endometrium in patients with dorsal node location. The number of heteromorphic secretory cells in endometrial samples in these patients was also significantly higher than in patients with the location of the node on the anterior wall of the uterus, respectively, 53.33% against 5.88%; p=0.002. There were no significant differences in the state of intercellular contacts and microenvironment cells (Table 6). At the same time, attention is drawn to the high frequency of prevalence in both groups of disconnection of intercellular contacts, which is important for successful invasion of trophoblast.
| No. | Features | Units | The main group after MRI-guided HIFU ablation of uterine fibroids (anterior wall) (n=17) |
The main group after MRI-guided HIFU ablation of uterine fibroids (posterior wall) (n=15) |
χ2 | р |
|---|---|---|---|---|---|---|
| 1 | The "calm" epithelium | % | 17.64% | 26.67% | 0.67827** | 0.538 |
| абс. | 3 | 4 | ||||
| 2 | Maturing pinopodia | % | 52.94% | 73.33% | 1.919* | 0.166 |
| абс. | 9 | 11 | ||||
| 3 | Mature pinopodia | % | 77.78% | 53.33% | 0.678* | 0.411 |
| абс. | 14 | 8 | ||||
| 4 | Asynchronous maturation of pinopodia | % | 11.76% | 46.67% | 0.04915** | 0.026 |
| абс. | 2 | 7 | ||||
| 5 | Heteromorphic secretory cells | % | 5.88% | 53.33% | 0.00495** | 0.002 |
| абс. | 1 | 8 | ||||
| 6 | Saved intercellular contacts | % | 29.41% | 26.67% | 0.69886** | 0.539 |
| абс. | 5 | 4 | ||||
| 7 | Disconnected intercellular contacts | % | 70.59% | 80.00% | 0.376 | 0.540 |
| абс. | 12 | 12 | ||||
| 8 | Atypical ciliated cells | % | 17.65% | 26.67% | 0.67827** | 0.539 |
| абс. | 3 | 4 |
Surgical treatment for uterine fibroids takes over 70% of the total number of surgical interventions in gynaecology [1]. Currently, the gold standard for treating uterine fibroids in reproductive age patients planning pregnancy is laparoscopic myomectomy with careful layer-by-layer suturing of the uterus fibroid bed [7-9]. Recovery of reproductive function after myomectomy varies from 5 to 69% of cases according to various authors [1-10].
The findings of the researchers regarding the effect of surgical treatment of uterine fibroids on fertility restoration are different. Some scientists have shown an improvement in the results of infertility treatment after myomectomy, while others have shown that surgical treatment can solve the problem of infertility only in women whose fibroids were the only factor in infertility, in particular, hysteroresectoscopy for sub mucous uterine fibroids. Also, the opinions of scientists were divided on the removal of nodes with intramural localization, which may not affect the effectiveness of infertility treatment [10]. At the same time, many authors agree that performing myomectomy improves pregnancy outcomes and reduces obstetric risks (reducing the frequency of spontaneous miscarriage, premature birth), but the frequency of abdominal deliveries is increasing [8-12].
Currently, there are alternative, non-invasive methods of organpreserving treatment. MRI-guided HIFU ablation is a non-invasive method, uterine fibroids treatment in which ultrasound energy is focused deep inside the tumour under the control of an MRI image, increasing the intra-tumour temperature, causing tumour necrosis [13,14]. To date, the question of the impact of this treatment on reproductive function remains controversial, despite the fact that the world literature describes more than 150 cases of pregnancies after MRI-guided HIFU ablation of uterine fibroids [15].
Maconade N. et al. assessed the risk factors for the development of pregnancy complications in women after previously performed MRI-guided HIFU ablation. The rate of spontaneous miscarriages was 26%, which is comparable to that of women without uterine fibroids. The birth of live healthy children was described in 41% of cases, in 11% there was a spontaneous termination of pregnancy, 20% of women were 20 weeks pregnant at the time of termination of the study. The rate of spontaneous labor was 64%. Literature data on the outcomes of pregnancies after MRI-guided HIFU ablation-are few, but show that fertility after this procedure is preserved [16,17].
Researchers have suggested that pinopodia are reliable markers of endometrial susceptibility in the "implantation window" [18,19]. The presence of fully developed, mature pinopodia indicates that the endometrium is ready for implantation [19]. Other probable properties of pinopodia include the processes of reabsorption of macromolecules and fluid from the lumen of the uterus and inhibition of the movement of the cilia, resulting in the attachment of the blastocyst. It is also assumed that the pinopodia are enriched with a network of f-actin cytoskeleton molecules, which are involved in trophoblast adhesion to the endometrial epithelium [19-22]. Researchers have shown that the formation of pinopodia coincides with the loss of dense intercellular contacts of endometrial epithelial cells, which facilitates adhesion and penetration of blastocysts into the endometrium. Studying ultra-structural indicators of endometrial receptivity during the period of the alleged " implantation window” in patients with uterine fibroids in General, a certain chronometric lag in the rates of maturation of the pinopodia and preparation of the endometrium for implantation was found. In most endometrial samples, the secretory cells had a domed shape with preserved thickened microvilli. The loss of microvilli on the surface of the pinopodia characterizes their full maturation and the readiness of the surface epithelium of the endometrium to perceive the blastocyst. Chronometric lag in the maturation of pinopodia in patients with uterine fibroids was naturally accompanied by a delay in the separation of dense intercellular contacts necessary for implantation of blastocysts in the endometrium. The ultrastructural picture of implantation endometrium of patients with uterine myoma was characterized by a high frequency of verification of atypical structure of microenvironment cells. Ciliated cells, as a rule, were partially deepened relative to the surface of the secretory cells and had an atypical flask shape.
In the study of the influence of the energy of focused ultrasonic waves used for ablation of uterine fibroids on ultra-structural markers of endometrial receptivity, a significant increase in the incidence of mature pinopodia fields in samples of implantation endometrium of patients after MRI-guided HIFU ablation was revealed due to a corresponding decrease in the frequency of verification of maturing pinopodia. This may indicate the normalization of the rate of maturation of pinopodia after this type of treatment of uterine fibroids. A higher frequency of detection of mature pinopodia was naturally accompanied by a change in the state of intercellular contacts, namely, a higher frequency of their separation.
One of the important features of the ultra-structural picture of the endometrium revealed during the treatment use of MRIguided HIFU ablation of uterine fibroids is a significant increase in the frequency of asynchronous maturation of pinopodia and heteromorphic structure of secretory cells. This was manifested by uneven fields of pinopodia maturation, in which both mature pinopodia and secretory cells were present in significant numbers at various stages of pinopodia maturation, from the stage of preparation for maturation to a state close to mature structures. The secretory cells themselves in one third of the observations were characterized by heteromorphic structure, had different polygonal shape.
To analyse the effect of focused ultrasound energy on endometrial receptivity, the ultra-structural characteristics of the endometrial surface epithelium during the "implantation window" in patients with a dominant node located on the anterior or posterior wall of the uterus were compared. According to our hypothesis, when the dominant node is located on the anterior wall of the uterus, there is no penetrating direct impact of focused ultrasound rays on the endometrium, the tissue is exposed to scattered reflected rays. When the dominant node is located on the posterior wall of the uterus, ultrasound focused on the node has a direct penetrating effect on the endometrium.
In our study, it was shown that focused ultrasound rays passing through the endometrium do not cause suppression or, conversely, acceleration of pinopodia maturation, there was no change in the rate of pinopodia maturation depending on the type of primary ultrasound passage through the tissue. At the same time, a significant increase in the frequency of asynchronous maturation of pinopodia and the number of heteromorphic secretory cells in the implantation endometrium was found. This may indicate a certain influence of penetrating focused ultrasound on the functional state of individual endometrial cells and inhibition of intercellular interactions under the influence of ultrasonic wave energy.
The detected changes may have important clinical significance. In previous studies, we have shown that the ultra-structural picture of the endometrium with asynchronous type of pinopodia maturation is most characteristic for patients with habitual early pregnancy losses associated with uterine factor of reproductive failures [23]. Therefore, laparoscopic myomectomy may be considered as the first line of treatment for uterine fibroids in patients with habitual miscarriage [24]. At the same time, the literature data on the outcomes of pregnancies that occurred after MRI-guided HIFU ablation of uterine fibroids are few and do not allow to reliably judge the population excess of the frequency of miscarriage after MRI-guided HIFU ablation [25-26]. In patients whose main cause of infertility is a violation of the receptivity of the endometrium due to uterine myoma, the use of MRI-guided HIFU ablation can be considered as a treatment option with the right choice of indications and conditions for its implementation. There are data from studies on the increase in the frequency of pregnancy and the frequency of live births after MRI-guided HIFU ablation in patients whose main cause of reproductive failure was uterine fibroids [23-26].
Summarizing the study, it should be noted that the research methodology aimed at studying the effect of focused ultrasound energy on tissue markers of endometrial receptivity in patients after treatment of uterine fibroids was undoubtedly a strong side of the study. There are very few such works in the world literature. The problem remains relevant in terms of the possible use of HIFU ablation of uterine fibroids as preparation for gestation.
The study limitations are associated with a small sample of patients. Further in-depth studies, accumulation and expansion of the database of clinical data on reproductive outcomes of the use of a non-invasive method of treatment of symptomatic uterine fibroids in patients of reproductive age are needed.
The study did not reveal any significant negative effects of focused ultrasonic waves during FUS-MRI ablation of uterine fibroids on endometrial receptivity in women of reproductive age. MRg HIFU ablation of uterine fibroids might be considered as an alternative treatment in patients of reproductive age with uterine fibroids planning a pregnancy.
The study was supported by grant 19-315-90028 of the Russian Foundation for Basic Research (RFBR) as part of a competition for the best fundamental research projects carried out by young scientists studying in graduate school ("Postgraduates").
Citation: Melkozerova OA, Shchedrina ID, Malgina GB, Mikhelson AA, Chistyakova GN (2020) Changes in Tissue Endometrial Receptivity under the Influence of High Intensity Focused Ultrasound during Ablation of Uterine Fibroids in Patients of Reproductive Age. J Women's Health Care 9:491. doi:10.35248/2167-0420.20.9.491.
Received: 15-May-2020 Accepted: 18-Jun-2020 Published: 25-Jun-2020 , DOI: 10.35248/2167-0420.20.9.491
Copyright: �© 2020 Melkozerova OA, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.