Reproductive System & Sexual Disorders: Current Research
Open Access
ISSN: 2161-038X
ISSN: 2161-038X
Research Article - (2022)Volume 11, Issue 4
Background: Postdate pregnancies are associated with increased risk of fetal and maternal morbidity and mortality. The Cerebro Placental Ratio (CPR) is emerging as an important non-invasive tool to assess fetal wellbeing and predict adverse outcome in high risk pregnancies. The aim of this report was to evaluate the value of Doppler CPR in predicting adverse pregnancy outcome in the setting.
Methods: This was a prospective study of 97 pregnant women from 40 weeks of gestation. Fetal Doppler evaluation of the Pulsatility Index (PI) of the Umbilical Artery (UA) and Middle Cerebral Artery (MCA) were done and the CPR calculated as MCA-PI/UA-PI. The women were followed up until delivery the following data collected: The Apgar score, birth weight and information about SCBU admission.
Results: The women were aged 19-41 years (mean 30.22 ± 4.8 years) and the pregnancies were at 40-41+3 weeks. The mean UA-PI, MCA-PI and CPR were 0.83 ± 0.16, 1.15 ± 0.19 and 1.42 ± 0.31, respectively. Abnormal UA-PI, MCA-PI and CPR were associated with an increased risk of adverse perinatal outcome (relative risk of 4.72, 7.08 and 9.78 respectively). Abnormal UA-PI was associated with fetal distress, abnormal MCA-PI was associated with fetal distress, low Apgar score at 1 minute and special care baby unit admission, and abnormal CPR was associated with fetal distress and low Apgar score at 1 minute.
Conclusion: CPR is a good predictor of adverse perinatal outcome in postdate pregnancy and is recommended as an adjunct in evaluation of fetal wellbeing in this setting and similar settings.
Postdate pregnancy; Cerebroplacental ratio; Perinatal outcome
CPR: Cerebroplacental Ratio; PI: Pulsatility Index; UA: Umbilical Artery; MCA: Middle Cerebral Artery; EDD: Expected Date of Delivery; LMP: Last Menstrual Period; CTG: Cardiotocography; MAS: Meconium Aspiration Syndrome; SCBU: Special Care Baby Unit; SPSS: Statistical Package for the Social Sciences
A postdate pregnancy is one that has exceeded the Expected Date of Delivery (EDD) of 40 weeks or 280 days from the first day of Last Menstrual Period (LMP) [1,2]. These are high risk pregnancies with substantial fetal and maternal risks. The incidence of postdate pregnancy in Nigeria have been reported at 3% - 13% of total deliveries [2-6]. These pregnancies require appropriate surveillance for early diagnosis as well as prediction morbidity and mortality.
Doppler ultrasound, a non-invasive method of fetal surveillance allows for assessment of the blood flow velocity waveform of maternal and fetal blood vessels including the Uterine Artery (UtA), Middle Cerebral Artery (MCA) and Umbilical Artery (UA) [7,8]. The fetalplacental circulation can also be assessed [9-11]. The fetal Cerebro Placental Ratio (CPR) is the ratio of the fetal MCA Pulsatility Index (PI) to UA PI. CPR has been noted to be a better predictor of adverse perinatal outcomes compared to other conventional anthropometric models [12].
In Nigeria, the role of Doppler CPR to predict perinatal outcomes has not been adequately evaluated. The aim of this study was to assess the value of CPR in predicting adverse fetal outcome in postdate pregnancies. The working hypothesis was that CPR predicts adverse perinatal outcome in postdate pregnancies.
The study was conducted at the Department of Obstetrics and Gynaecology, University of Abuja Teaching Hospital, Abuja, Nigeria, a 350-bed tertiary health facility. In this facility, modified biophysical profile is used to monitor postdate pregnancy. The major limitation is cardiotocography was not done due to unavailability of a functioning machine. With the availability of a modern ultrasound machine with a Doppler facility, a Doppler scan may be worthwhile in management of the postdate pregnancies.
This was a prospective observational study of women with uncomplicated postdate pregnancies at gestational age of 40-41+3 weeks, from August 2018-Febuary 2019. Women with singletons live fetus in cephalic presentation and accurate dating were included in the study. Women with the following were excluded; obstetric or medical complication(s)-IUGR, diabetes mellitus, hypertensive diseases in pregnancy, sickles cell disease, poor dating, multiple pregnancy, and breech presentation. A calculated sample size of 100 using: A calculated sample size of 100 (using n=z2 pq/d2, where n is sample size, z is standard normal deviation (a constant) where n is sample size, z is standard normal deviation (a constant) which is 1.96 at 95% confidence interval at 95% confidence interval, p is percentage of study population with abnormal CPR from a previous study, q is 1-p and d is margin of error of 5%, and attrition of 10%) was used. An informed consent was obtained from each woman before inclusion in the study.
At the time of the study, there was no facility for fetal blood sampling and measurement of blood gases to confirm fetal distress. Use of CardioTocography (CTG) was not possible due to a faulty CTG machine.
Study protocol
After obtaining consent from the participants, the ultrasound was carried out using the General Electric Healthcare VolusonTM P8 (2016 model) with Doppler unit and convex linear transducer 3.5 MHz. A basic scan was first conducted in B-Mode using the 3.5 MHz curvilinear transducer to determine the viability, number, lie and presentation of the fetus as well as the placentation and liquor volume. A fetal biometry was carried out.
Using the same transducer and mode, a free loop of umbilical cord was located. The umbilical artery was identified using colour Doppler interrogation. Pulsed Doppler with a gate size of 2 mm was applied at an angle of insolation ≤ 30°. The Pulsatility Index (PI) was automatically generated by the machine and value recorded when uniform consecutive waveforms were generated in the absence of fetal movement and breathing.
Middle Cerebral Artery (MCA) Axial section of the brain, including the thalami and septum cavum pellucidi was obtained and magnified on B-Mode. Traducer was moved to the base of the skull until the circle of Willis was identified. The MCA was identified with colour Doppler. The scanning plane was adjusted to obtain an insonation angle close to 0° but <15° at the level of the proximal portion of the MCA close to its origin from the circle of Willis with a sample volume of 2-3 mm. Care was taken not to exert pressure on the fetal head because this alters the flow velocity waveforms from the MCA. The automatically generated Pulsatility Index (PI) was recorded when uniform consecutive waveforms were generated in the absence of fetal movement and breathing. The right and left MCA pulsatility index was measured, and the mean recorded. The Pulsatility Index (PI) and the cerebroplacental ratio were calculated using the formula:
Cerebroplacental Ratio (CPR)=Middle Cerebral Artery-PI/Umbilical Artery-PI
The Doppler evaluation was done once by the researcher and the consultant radiologist. Patients were followed up till delivery and relevant data collected. Cutoff values for normal and abnormal UA PI, MCAPI and CPR were generated using the 10th and 90th percentile. The study population was divided into two groups based on normal and abnormal Doppler parameters.
Adverse perinatal outcome was defined as the presence of one or more of the following: Fetal distress, Apgar score <7 at 1 and 5 min, Meconium Aspiration Syndrome (MAS) and admission into Special Care Baby Unit (SCBU).
Data analysis
Data was entered into a personal computer and analysis was done using the IBM Statistical Package for the Social Sciences (SPSS) version 23 software. A percentile plot of the Doppler variables was carried out and the UA PI was considered abnormal when the values were >90th percentile while the MCA PI and CPR were considered abnormal when the values were <10th percentile. Chi square was used for categorical variables and where the criterion for X2-test was not met, Fisher’s Exact Test was used.
Primary outcome measures were fetal distress and birth asphyxia. Secondary outcome measures were: MAS, admission into SCBU, CS for fetal distress, PPH. MAS were diagnosed as visual observation of greenish discoloration of the liquor with respiratory difficulties. Fetal distress was defined as ominous FHR changes (tachycardia or bradycardia) that led to caesarean section or instrumental delivery.
Ethical approval
Approval for the conduct of the study was obtained from the Health Research and Ethics Committee of University of Abuja Teaching Hospital. The approval number was UATH/HREC/2018/06/001.
Demographics
Of the 100 women recruited into the study, 3 were lost to follow and have been excluded from analysis. The demographics are summarized in Table 1.
| Variable | No. (%) |
|---|---|
| Maternal age (years) | 30.22 ± 4.8 |
| Maternal height (m) | 1.65 ± 0.1 |
| Maternal weight (kg) | 80.27 ± 13.3 |
| Parity | |
| 0 | 22 (22.7) |
| 01-Apr | 74 (76.3) |
| >4 | 1(1.0) |
| Gestational age | |
| 40-40+6 weeks | 80 (82.4) |
| 41-41+3weeks | 17 (17.5) |
| Educational status | |
| No formal education | 1(1.0) |
| Primary | 1(1.0) |
| Secondary | 19(19.6) |
| Tertiary | 76(78.4) |
| Mode of delivery | |
| Spontaneous vagina | 78 (80.4) |
| Caesarean section | 19 (19.6) |
Note: Maternal age, height and weight are expressed as mean ± SD, Parity, gestational age and mode of delivery are expressed as n (%).
Table 1: Socio-demographic characteristics of 97 women included in the study.
The commonest indication for caesarean section was fetal distress (42.1%). Twenty-two women (22.68%) had induction of labour, of which 18(81.8%) had a normal fetal outcome while 4(18.2%) had an adverse outcome (p=0.23). Ten (10.3%) of all the babies delivered had an adverse perinatal outcome while 87(89.7%) had a normal outcome. The composite adverse fetal outcome include: eight cases of fetal distress and four cases of four cases of one minute Apgar score less than 1.
Two (2.06%) of the women had postpartum haemorrhage and 3(3.09%) had second degree perineal tears which were repaired. There was no maternal mortality.
Umbilical artery pulsativity index
The mean UA PI was 0.83 ± 0.16 (range 0.47-1.18). Twelve fetuses had an abnormal UA PI and 85 had a normal UA PI. Four (33.3%) fetuses with abnormal UA PI developed fetal distress resulting in caesarean section compared to 4 (4.7%) with normal UAPI (p 0.001, relative risk >7). There was no significant difference in the Apgar scores at 1 and 5-minute, admission into SCBU or meconium aspiration syndrome between fetuses with abnormal and normal UAPI. Fetuses with abnormal UAPI had a significantly higher total adverse perinatal outcome (p 0.005, relative risk >4) (Table 2).
| Characteristic | Normal pulsatility index | Abnormal pulsatility index | p Value | Relative risk (95% CI) |
|---|---|---|---|---|
| (n = 85) | (n = 12) | |||
| No. (%) | No. (%) | |||
| UA PI (normal<1.03; abnormal ≥ 1.03) | ||||
| Fetal distress | 4 (4.7) | 4 (33.3) | 0.001 | 7.08 (2.01–14.98) |
| APGAR score <7 at 1 minute | 13 (15.3) | 3 (25.0) | 0.4 | 1.63 (0.48–3.81) |
| APGAR score <7 at 5 minutes | 1 (1.2) | 1 (8.3) | 0.1 | 7.08 (0.45–51.79) |
| SCBU admission | 3 (3.5) | 1 (9.1) | 0.39 | 2.58 (0.27–14.55) |
| Meconium aspiration | 1 (1.19) | 0 | 0.72 | |
| Perinatal outcome | ||||
| Adverse outcome | 6 (7.1) | 4 (33.3) | 0.005 | 4.72 (1.47–9.67) |
| Normal outcome | 79 (92.9) | 8 (66.7) | ||
| MCA PI (normal <0.90; abnormal ≥ 0.90) | ||||
| Fetal distress | 4 (4.7) | 4 (33.3) | 0.001 | 7.08 (2.01–14.98) |
| APGAR score <7 at 1 minute | 10 (11.8) | 6 (50.0) | 0.001 | 4.25 (1.81–6.69) |
| APGAR score <7 at 5 minutes | 1 (1.2) | 1 (8.3) | 0.1 | 7.08 (0.45–51.79) |
| SCBU admission | 2 (2.4) | 2 (16.7) | 0.02 | 7.00 (1.04–25.72) |
| Meconium aspiration | 0 | 1 (8.3) | 0.008 | |
| Perinatal outcome | ||||
| Adverse outcome | 5 (5.9) | 5 (41.7) | <0.001 | 7.08 (2.42–12.83) |
| Normal outcome | 80 (94.1) | 7(8.3) | ||
| CPR (normal <1.02; abnormal ≥ 1.02) | n=88 | n=9 | ||
| No. (%) | No. (%) | |||
| Fetal distress | 4 (6.8) | 4 (22.2) | <0.001 | 9.78 (2.92–17.75) |
| APGAR score <7 at 1 minute | 12 (13.6) | 4 (44.4) | 0.02 | 3.26 (1.16–5.67) |
| APGAR score <7 at 5 minutes | 1(1.14) | 1(11.1) | 0.05 | 9.78 (0.62–60.44) |
| SCBU admission | 3 (3.4) | 1 (12.5) | 0.22 | 3.67 (0.38–17.88) |
| Meconium aspiration | 0 | 1 (12.5) | 0.001 | |
| Perinatal outcome | ||||
| Adverse outcome | 5 (5.7) | 5 (55.6) | 0.001 | 9.78 (3.56–15.14) |
| Normal outcome | 83 (94.3) | 4 (44.4) | ||
Table 2: Relationship between UA PI, MCA PI, and perinatal outcome in 97 postdate pregnancies.
Middle cerebral artery pultativity index
The mean MCA PI was 1.15 ± 0.19 (range 0.66-1.18). Twelve fetuses had an abnormal MCA PI and 85 had a normal MCA PI. These were the same fetuses that had abnormal UA PI. Fetuses with abnormal MCA PI had significantly increased risk of developing fetal distress resulting in caesarean section, Apgar score <7 at the 1st minute and admission into SCBU (p 0.001, 0.001 and 0.02 respectively, relative risk >7, 7 and >4 respectively). There was no significant difference in the Apgar scores at 5 minutes between fetuses with abnormal and normal MCA PI. There was a statistically significant difference between the two groups in the total adverse perinatal outcome (P<0.001) with a relative risk >7 (Table 2).
Cerebroplacental Ratio (CPR)
The mean CPR was 1.42 ± 0.31 (0.8-2.4). Nine (9.3%) fetuses had an abnormal CPR and 88 (90.7%) normal CPR. Fetuses with abnormal CPR were found to be at a significantly increased risk of developing fetal distress resulting in caesarean section and an Apgar score <7 at the 1st minute (p <0.001 and 0.002 respectively, and relative risk >9 and >3 respectively). There was no significant difference in the Apgar scores at 5-minute, admission into SCBU or meconium aspiration syndrome between fetuses with abnormal and normal CPR. There was significantly more total adverse perinatal outcome in fetuses with abnormal CPR (p<0.001, relative risk >9) (Table 2 and Figure 1). There were no stillbirths or early neonatal deaths in any group.
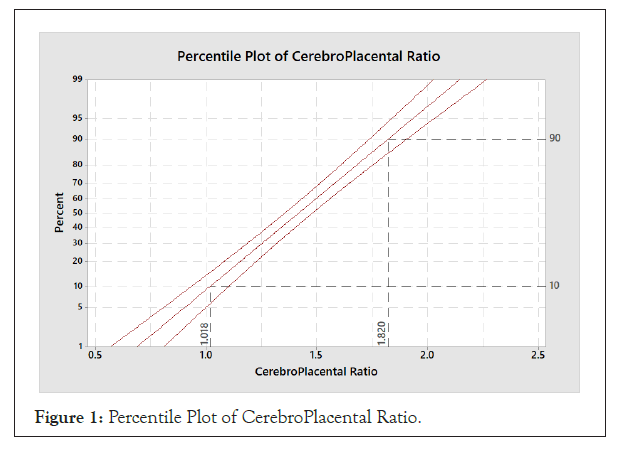
Figure 1: Percentile Plot of CerebroPlacental Ratio.
The sensitivity, specificity, positive predictive value and negative predictive value were estimated for the UA PI, MCA PI and CPR. The area under the curve (AUC) for CPR and MCA PI were statistically significant with a P value of 0.02 and 0.03 respectively when compare to normal.
Although there is insufficient evidence to recommend a management strategy for pregnancies beyond 40 weeks, management options include, expectant management with antepartum testing, induction of labour and caesarean section when indicated [13,14]. Initiation of fetal surveillance at 41 weeks is considered a reasonable option and improvements in antepartum fetal surveillance methods has led to a reduction in perinatal morbidity and mortality [5,13]. The options of fetal surveillance include, fetal kick charts, Biophysical Profile (BPP), Modified BPP, Amniotic Fluid Volume (AFV), Non Stress Test (NST), contraction stress test, Doppler studies and a combination of these modalities [14-16].
In the present report, fetal distress was the most common indication for caesarean sections the 19 (19.6%) participants who had procedure. The mean UA PI, MCA PI and CPR were 0.83, 1.15 and 1.42, respectively. These values fell within the reference ranges in another report at gestational ages of between 41-41+3 weeks [17]. Important information was obtained with regards to the relationship between indices for adverse perinatal outcomes and, UA-PI, MCA-PI, and CPR.
The cut-off value for an abnormal UA PI generated in the present study was ≥1.03. Fetuses with an abnormal UA PI were shown to be at a significantly increased risk of fetal distress resulting in caesarean section similar to other reports [7,18-20]. An abnormal UA PI also resulted in more than a four-fold increase in the risk of an adverse perinatal outcome. This may support the theory that adverse perinatal outcome in postdate pregnancy is due to placental insufficiency with an increased impedance in the umbilical artery leading to increased resistance and reduced blood flow [19]. However, severe degrees of umbilical Doppler abnormalities such as absent or reversed end diastolic flow are rare findings in postdate pregnancy and are associated with poor outcomes [18]. Other reports found no change in impedance to blood flow in the UA and UA Doppler was not a useful predictor of adverse perinatal outcome [8,21].
Fetuses with an abnormal MCA-PI cut off of ≤ 0.9 were at an increased risk of fetal distress resulting in caesarean section, APGAR score <7 at the 1st minute, admission into SCBU and a more than sevenfold increased risk of adverse perinatal outcome as in other reports [8,14,15,22]. This may support the theory of a Brain Sparing (BS) phenomenon in postdate pregnancies with an adverse outcome. However, other reports have found women with an adverse outcome to have normal MCA-PI [13,16,17]. This has been explained that in uncomplicated postdate pregnancies, the mechanism of fetal compromise is perhaps due to a decrease in flow of nutrients across the placenta and decrease in efficiency of utilization of nutrients by the placenta and the fetus and not uteroplacental insufficiency with a resultant BS effect [13]. In the present report, MCA-PI had a better predictive value for adverse perinatal outcome in postdate pregnancies compared to UA PI as in other reports [14,22].
Using a cut-off value of ≤ 1.02 for abnormal CPR, 9.3% of the study fetuses had an abnormal CPR. An abnormal CPR had a positive correlation with fetal distress resulting in caesarean section, APGAR score <7 at the 1st minute and more than nine-fold increased risk of an adverse perinatal outcome, as in other reports [5,7,18,22,23]. Although the UA-PI and MCA-PI alone did not predict adverse outcome in another report, CPR with a cut off at 1.3 had a high sensitivity and negative predictive value [8]. This supports the use of the CPR even in the presence of an apparently normal UA-PI and MCA-PI to predict adverse perinatal outcome.
Among the three Doppler parameters studied, the CPR had the best discriminatory ability to predict fetuses likely to have an adverse perinatal outcome with a specificity of 95.4% and sensitivity of 50%. MCA-PI closely follows, with the same sensitivity as the CPR (50%) and slightly lesser specificity (92%). MCA-PI was however the only parameter with a significant positive correlation with admission into the SCBU. This is similar to other reports [7,18,23,24]. Although the sensitivity, specificity, positive predictive and negative predictive values for CPR in the present report were lower than previously reported, the difference may be due to the addition of high risk women with postdate pregnancies as in another report, or due differences in cut-off values used and the frequency of Doppler measurements [5,7,17,18,23].
CPR can predict adverse perinatal outcome irrespective of the individual UA-PI and MCA-PI. The high specificity and negative predictive value of CPR provides a good indication of fetal wellbeing and could help in preventing unnecessary interventions. Doppler CPR should be used to complement other antepartum parameters in the surveillance of postdate pregnancy. A systematic review and meta-analysis is needed to further ascertain the role of CPR in routine surveillance of postdate pregnancy.
None
None
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar][All versions] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [All versions] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] (All versions) [PubMed]
Citation: Ale OV, Adewole ND, Suleiman B, Kolade-Yunusa HO (2022) Cerebroplacental Ratio in the Prediction of Adverse Perinatal Outcome in Postdate Pregnancy: A Prospective Study. Reprod Syst Sex Disord.11:318.
Received: 29-Apr-2022, Manuscript No. RSSD-22-17266; Editor assigned: 02-May-2022, Pre QC No. RSSD-22-17266(PQ); Reviewed: 20-May-2022, QC No. RSSD-22-17266; Revised: 30-May-2022, Manuscript No. RSSD-22-17266(R); Published: 08-Jun-2022 , DOI: 10.35248/2161- 038X.22.11.318
Copyright: © 2022 Ale OV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.