
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2022)Volume 13, Issue 9
Carotid body tumours are rare benign tumours with a reported incidence of 1-2 per 1,00,000; arising at the bifurcation of the carotid artery. The carotid body is responsible for sensing the partial pressure of oxygen and carbon dioxide in the blood; and hence, it is vital for controlling of ventilation during hypoxia, hypercapnia, and acidosis. Surgical excision is the preferred treatment modality for this condition. The authors present a case report of a 30-yearold patient who underwent excision of a left-sided carotid body tumour and discuss anaesthetic management.
Carotid body; Excision; Hypotensive anaesthesia
Carotid Body tumour is a rare benign tumour which is a nonchromaffin paraganglioma arising from the chemoreceptor cells at the bifurcation of the carotid artery in the neck [1]. The carotid body tumor is the most common paraganglioma in the head and neck, and the most frequent combination of multiple tumors is bilateral carotid body tumors. Despite being benign, the tumour can create problems due to mechanical pressure on the neighboring neuro-vascular structures like the Internal Carotid artery, Vagus nerve, Hypoglossal nerve and Superior laryngeal nerve. Surgical excision of tumour is the preferred choice of treatment with a high risk of peri-operative morbidity and mortality while posing serious challenges to the anaesthetist. The anaesthetist must be available for surgical excision of tumour to ensure safe, yet complete removal of Carotid Body tumour.
A 30-year-old female presented to the Surgery OPD of the author’s institution with a slow growing, lump over the left side of the neck for over a period of 4 years with a history of difficulty in deglutition and hoarseness of voice [2]. Computerized Tomography (CT) angiogram confirmed the diagnosis of a highly vascular carotid body tumour measuringoperative anaesthetic concerns included difficulty in intubation, massive blood loss and elective post-operative mechanical ventilation (Figure 1).5*4*5 cm for which an elective excision procedure was planned after subjecting her to trans-catheter embolisation.
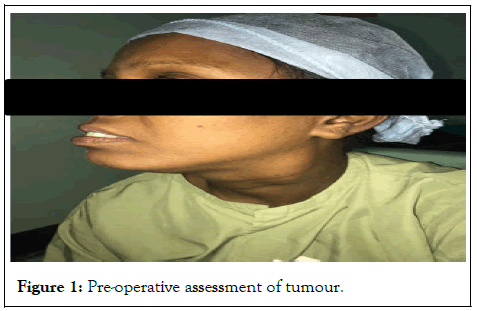
Figure 1: Pre-operative assessment of tumour.
Pre-operatively a day before the elective surgery, informed highrisk consent was taken [3]. The patient and relatives were well informed and counselled about the complications along with various peri-operative concerns. Anticipated post-operative ICU with ventilator support was reserved for the patient (Figure 2).
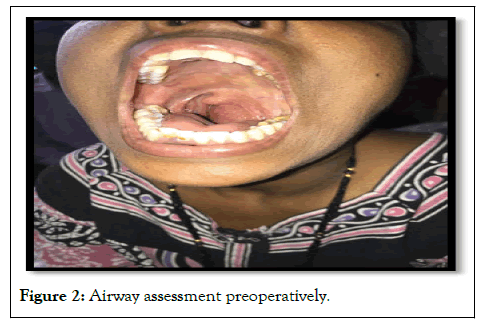
Figure 2: Airway assessment preoperatively.
The patient was wheeled into the operative room and standard monitors (non-invasive blood pressure, electrocardiograph and arterial oxygen saturation (SPO2) monitors were attached and all vital parameters were recorded. In the preoperative room, the patient was administered nebulisation with duolin, along with glycopyrrolate intravenously. The patient was made to gargle with a viscous solution of lignocaine solution (2% preparation). Otrivin (Xylometazoline) drops were instilled in both the nostrils, an oral spray of lignocaine into the oral cavity was used along with a transtracheal block. Further, midazolam 1 mg and fentanyl 50 mcg were administered and a slow-controlled intravenous infusion of dexmedetomidine 30 mcg/100 ml was started. The appropriate-sized tube was loaded over fibre-optic scope, and the scope passed through the oral cavity [4]. On visualising the vocal cords, lox 2% spray was used, further progressing the scope. On crossing the vocal cords, the tracheal rings were seen, further rail-roading the endotracheal tube. The endotracheal tube placement was also confirmed by End-Tidal CO2 measurement and four-point auscultation. The patient was eventually induced with propofol and paralysed using muscle relaxant vecuronium. A subclavian central venous line with a triple lumen catheter and an arterial line were secured for continuous hemodynamic monitoring (Figure 3).
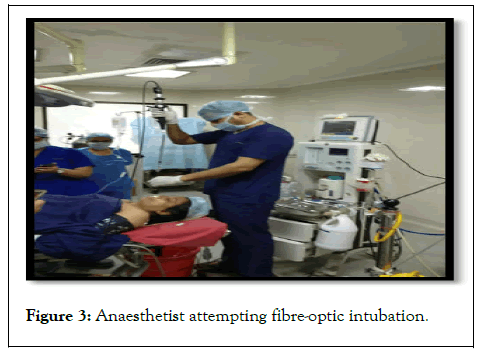
Figure 3: Anaesthetist attempting fibre-optic intubation.
General anaesthesia was maintained with oxygen/air (FiO2:100%) Isoflurane (1-1.5%) with vecuronium used as the muscle relaxant. The total Duration of Surgery was 3 hours with a total blood loss of 400 ml. vital parameters were stable except for 2 episodes of bradycardia and hypotension during the handling of the tumour. Post-surgery, the patient was extubated, with neuromuscular reversal drugs using Neostigmine and Glycopyrrolate and transferred to surgical ICU for post-operative management and observation (Figure 4).
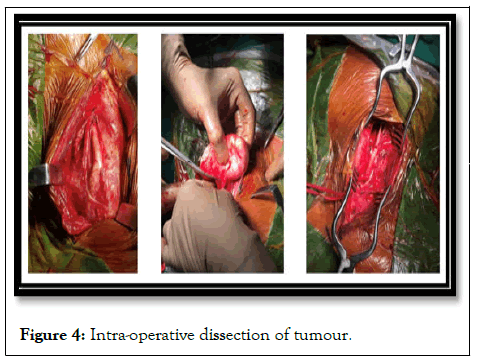
Figure 4: Intra-operative dissection of tumour.
The carotid body, first described by von Haller, it is a highly specialized chemoreceptor organ situated at the bifurcation of the Common carotid artery, which detects changes in arterial oxygen tension (Figure 5).
Figure 5: Post-operative scar.
According to Shamblin classification, carotid body tumours are classified into 3 types based on the severity of internal carotid artery involvement [5]. Type 1 have the least invasion into the internal carotid artery and can be easily removed. In Type 2, which is more common, the internal carotid artery is partially involved and surgical removal is challenging. Type 3, on the other hand, requires removal of the carotid artery as there is a complete invasion of the carotid artery by the tumour.
When literature is reviewed, mostly preference for general anaesthesia for Carotid Body Tumor surgery is noted. However, in some cases cited in the literature, local and regional anaesthesia was applied. In a series consisting of 4 cases reported by Toktas et al. local anaesthesia had been used, and no surgical complication was noted [5,6]. Cervical plexus block is a preferred anaesthetic method for carotid artery surgery with the complication arising from bleeding from the hyper-vascular tumour mass during attempts at block, as the tumour is located at the bifurcation of the carotid artery [7,8]. Needle or open biopsy is contraindicated in these tumours because of the risk of bleeding from the tumour [9]. The dangerous surges in BP occurring during induction of anaesthesia and surgical manipulation during excision of functional paragangliomas can be prevented by the administration of alpha-blockers preoperatively and beta-blockers intra-operatively. Moderate cooling of the patient (31°C) is recommended to prevent cerebral hypoxia [10]. Thiopentone (3-5 mg/kg/hr) infusion can be used to decrease the cerebral metabolic oxygen demand if the carotid artery has to be clamped. Involvement of cranial nerves (IX, X, XI) by tumour invasion preoperatively, nerve injury intra-operatively, or tissue oedema causing nerve palsy postoperatively may predispose to airway obstruction or aspiration.
The analysed clinicopathologic findings in 90 cases of carotid body tumours at the Mayo Clinic. Out of 90, 70 patients underwent surgical management, with total excision in 49, including 1 patient with bilateral tumours. The overall surgical mortality rate was 5.7 per cent, usually related to carotid arterial damage or ligation. In addition to this, a classification was suggested for future surgical cases. Group 1 tumours are relatively small and minimally attached to the carotid vessels where surgical excision usually can be carried out without difficulty. Group 2 tumours are usually larger and show moderate arterial attachment. These tumours are amenable to careful surgical removal. Group 3 tumours are usually large and incarcerate the carotids.
In a retrospective study at Antalya Training and Research Hospital, Antalya, Turkey between 2013 and 2016, 10 consecutive patients among 176 patients who underwent surgery for the management of carotid body tumors were analysed. The average intraoperative blood loss was 287 ± 68 ml. Tachycardia and hypertension was observed in 1 patient; bradycardia and hypotension were seen in 4 patients. Infusion for inotropic support was administered to 1 patient. The mean duration of operation was 109 ± 20 minutes. The mean VAS score was 4 ± 1, mean ICU tramadol consumption was 80 ± 25 mg. Duration of stay in ICU and hospital were 2.4 ± 1.1 hours and 3.8 ± 0.7 days, respectively. Mortality and neurological complications were not seen in the postoperative period. The analysed surgical treatment of paragangliomas of the carotid bifurcation. All patients underwent complete tumour resection. In 3 cases, resection of the internal carotid was necessary, where immediate reconstruction was performed. No patients had postoperative strokes. Five patients had postoperative nerve palsies. During the follow-up period of 4 months to 12 years, no patients had local recurrence developed the analysed anaesthetic management of a 38-year-old female, with Shamblin type II Carotid body tumour, thereby emphasising the importance of diagnosis based on clinical history, physical examination and MRI. A biopsy to confirm the diagnosis might turn out to be catastrophic.
Intraoperative techniques to reduce blood loss and arrhythmias must be used, and cerebral protection therapy needs to be considered in the event of brain ischaemia. Utmost vigilance is essential for anaesthetists during the surgical removal of a carotid body tumour to prevention of complications and prompts management for a successful surgical outcome. Preoperative assessment of tumour details and the airway is of utmost importance. Intensive monitoring and hypotensive anaesthesia with a high index of suspicion for possible complications are necessary to prevent them.
We would like to express an acknowledgement to the Department of Cardio-Vascular-Thoracic Surgery (CVTS) for their contribution to this case. We are immensely grateful to the operating surgeon Dr. Sameer Kadam, Head of department CVTS and his surgical team. We have to express our appreciation to the patient for her cooperation and to the hospital with staff members for their contribution to the case.
The authors declare that they have NO affiliations with or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Garg A, Jain G, Joshi A, Ranjan N, Sathe V (2022) Carotid Body Tumour: A 30 Year Old Female; Preoperative Concerns of an Anaesthetist. J Anesth Clin Res. 13: 1082.
Received: 03-Oct-2022, Manuscript No. JACR-22-19716; Editor assigned: 06-Oct-2022, Pre QC No. JACR-22-19716 (PQ); Reviewed: 21-Oct-2022, QC No. JACR-22-19716; Revised: 28-Oct-2022, Manuscript No. JACR-22-19716 (R); Published: 05-Nov-2022 , DOI: 10.35248/2155-6148.22.13.1082
Copyright: © 2022 Garg A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.