
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Review Article - (2021)Volume 12, Issue 1
Background and aim: Standard monitoring for tissue perfusion includes mixed venous saturation (CvSO2), blood lactate. Cerebral oximetry (CrSO2) non-invasively observes trends in cerebral saturation and it can be used as adjuvant to standard monitoring. The aim of the study is to evaluate septic shock mortality and patient outcome.
Methods: In this study 40 patients were entailed with septic shock at ICU for study period of 10 months. CrSO2 was monitored using “MASIMO O3 Regional Oximetry”. Patients were monitored with CrSO2, CvSO2, blood lactate, mean arterial pressure (MAP), arterial oxygen saturation (SaO2) 6 hourly for 72 hours. Patients with history of cerebrovascular diseases and neurological deficits were excluded from study. IBM SPSS Statistics, Version 24.0. software was used and independent t test, paired t test, Pearson coefficient (r) etc. parameter values were analyzed.
Results: There is significant negative correlation after six hours from admission was noticed between CrSO2 and lactic acid (r=-0.749 to -0.956). Significant positive correlation was noticed between CrSO2 and CvSO2 (r=0.904 to 0.993). In addition, significant positive correlation was also found between CrSO2 and mean arterial pressure (r=0.957 to 0.993) and SaO2 (r=0.864 to 0.988). Significant difference was also detected between the value of CrSO2 in the survivors (29 patients) and the non-survivors (11 patients) after 72 hours from admission.
Conclusion: CrSO2 could be parameters in patients with shock and it could have a prognostic value in mortality prediction and clinical outcome.
Cerebral oximetry; CrSO2; Septic shock
Septic shock, one type of circulatory shock is a common indication for intensive care unit (ICU) admission. It is defined as state of tissue hypoperfusion [1]. The Global tissue perfusion assessment is one of the main modes of management of hemodynamically challenged ICU admitted patients. There are multiple clinical and laboratory tests those are commonly used to measure the adequacy of global tissue perfusion in this very critical setting. This includes vital signs monitoring, certain clinical examination to assess the perfusion of different organs like monitoring the level of consciousness as a tool to predict the brain tissue perfusion (Figure 1) and urine output monitoring as a surrogate to the kidney perfusion. There are important laboratory data are routinely measured in the setting of shock as the blood lactate and serum bicarbonate level to reflect a state of hypoperfusion and anaerobic metabolism. Unfortunately, these clinical and laboratory monitoring of hypoperfusion carries their own limitations, they might be correlated and subjective based on the clinical findings, and these might be affected by the baseline clinical condition of patients and underlying comorbidities (e.g. chronic kidney disease, diabetes etc.) and some of the commonly used monitors are found to be invasive, intermittent, or reflect very late results of the same. Blood lactate level is a biochemical marker commonly used to assess tissue hypoxia secondary to impaired oxygen delivery during shock management and it has been included as one of the main criteria in the resuscitation bundle of the Surviving Sepsis Campaign, and it is also regarded as an important prognostic value as higher incidence of morbidity and mortality has been proven to be associated with higher level of lactate [2]. However, monitoring of blood lactate is limited, because it is invasive and intermittent and acute deterioration of the patient clinical condition can be missed until the next measurement. In addition, it has needed frequent blood samples, so it is associated with significant blood loss and higher risk of infection [3].
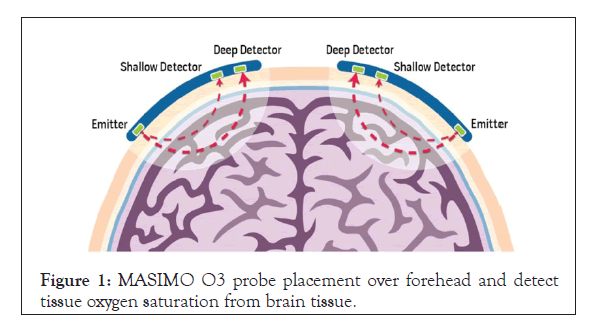
Figure 1: MASIMO O3 probe placement over forehead and detecttissue oxygen saturation from brain tissue.
Brain dysfunction due to brain tissue hypoxia is a known multisystem organ dysfunction that is commonly seen in shock. Fast timely resuscitation with appropriate management of shock should be made by obtaining global and regional perfusion parameters. Cerebral regional oxygen saturation (CrSO2) could be one of these parameters [4,5].
The relationship between different monitors of global hypoperfusion and the CrSO2 as a possible reliable monitor in patients with shock has not been widely described [6]. The aim of this study is to check the validity of CrSO2 as a parameter of perfusion in patients with shock and to determine the prognostic value of CrSO2 in the prediction of survival.
The study was conducted over 10 months from June 2018 to April 2019 initially on 56 adult patients after the approval of the Medical College Ethics committee and an informed written consent from patients. Inclusion criteria were age above 18 years, and diagnosed with circulatory septic shock, whereas patients with history of cerebrovascular diseases, computed tomography diagnosed brain pathology like haemorrhage infraction are excluded. Patients with acute neurological symptoms like hemiparesis, monopoiesis, convulsion, etc. and Patients who had a difference more than 10% between the 2 probes of MASIMO O3 Regional Oximetry (Masimo Corporation, Irvine, CA) (Figure 2) due to possible unilateral focal pathology are also excluded. Sixteen patients were excluded whereas 40 patients fulfilled the inclusion criteria and required to be admitted to the Critical Care Unit at Medical College Kolkata, West Bengal, India.
Figure 2: MASIMO O3 module.
It is a prospective open-labelled, single-centre pilot study. All patients were treated as per the latest guidelines and were monitored as per the usual recommended protocols [2]. In addition, their CrSO2 were monitored noninvasively and continuously using Near infrared spectroscopy (NIRS) with MASIMO O3 Regional Oximetry (Masimo Corporation, Irvine, CA). Two probes were attached to the forehead bilaterally.
Demographic data (age, sex, comorbidities, and diagnosis), hemodynamic parameters (mean arterial pressure [MAP], heart rate), serial lactic acid measurements at admission and 6 hour intervals, blood gases (arterial and central venous [at admission and 6 hour interval for recording and as often as required]), and CrSO2 (at admission and 6 hour interval) and arterial oxygen saturation (SaO2) recorded 6 hour interval.
Statistical analysis was done to check the correlation between CrSO2 and other parameters of perfusion. Data were fed to the computer and analysed using IBM SPSS Statistics for Windows 10, Version 24.0. Armonk, NY: IBM Corp. software package [7]. Qualitative data were described using number and percentage. Quantitative data were mean and standard deviation (SD) for normally distributed data, whereas median, minimum, and maximum were used for abnormally distributed data. For normally distributed data, independent t test was used to compare between survival and non-survival, also paired t test is used to analyse 2 paired data (CrSO2 and arterial oxygen saturation [SaO2]). Pearson coefficient was used to correlate between 2 quantitative variables. The significant test results were quoted as 2-tailed probabilities. The judgement done at 5% level for significance of the obtained results.
Considering power of 80% (Z value 0f 0.842) at 0.05 level of significance (α=0.05) taking Z value 1.96 from Z table at type 1 error of 5%, we have required 38 patients. The study was conducted initially on 56 patients assuming few dropouts; 16 patients were excluded from the study. Forty patients were included in the study, 20 (50%) of them were males and 20 (50%) were females. The mean age for the patients was 73.0 ± 10.97. The overall mortality was 27.5% as 11 of the 40 patients died.
Out of 56 patients 16 patients were excluded (3 patients had history of cerebrovascular stroke, and 2 patients had recent cerebral infarction confirmed radiologically, whereas 2 patients had cerebral haemorrhage, 5 patients had convulsions and paresis and 4 patients had more than 10% difference in CrSO2 between the 2 sides)
All patients in the study were diagnosed with septic shock with different source of sepsis; all were mechanically ventilated due to their shock status. Vasopressor choice was norepinephrine, which was titrated individually for each patient. Dobutamine was also used as cardiac involvement is verified by bedside echocardiography in Figure 3.
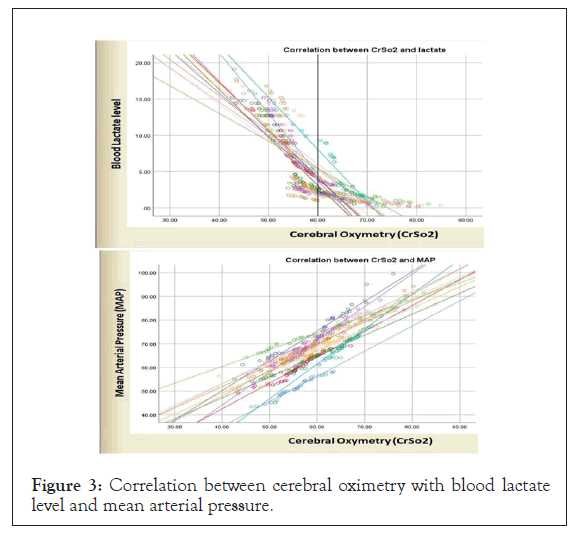
Figure 3: Correlation between cerebral oximetry with blood lactate level and mean arterial pressure.
Figure 4 showed serial measurements of all monitoring parameters over the first 72 hours from admission showing a general trend of incre`1ase in the CrSO2, the central venous saturation (CvSO2), the MAP, whereas there was a trend of decrease in the serum lactic acid level over time.
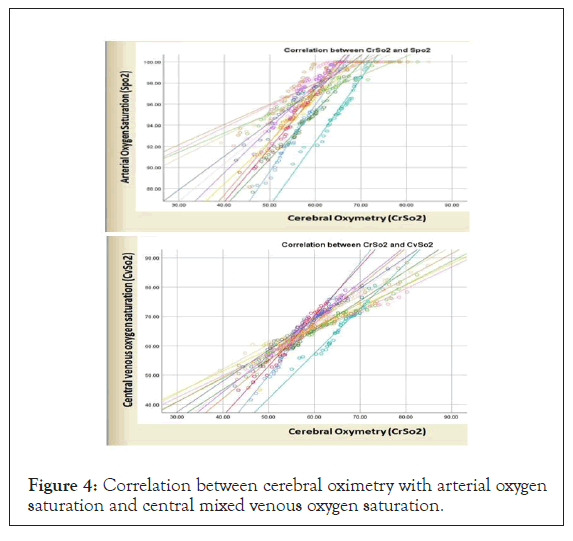
Figure 4: Correlation between cerebral oximetry with arterial oxygen saturation and central mixed venous oxygen saturation.
Figure 4 showed significant negative correlations, which was noticed between CrSO2 and lactic acid 6 hourly from admission. Significant positive correlation was noticed between CrSO2 and CvSO2 six hourly from admission. In addition, significant positive correlation was found between CrSO2 and MAP 6 hourly from admission.
In addition, the correlation between the CrSO2 and the level of serum lactic acid is presented which showed significant negative correlation between the 2 parameters from the beginning of the study and all through up to 72 hours and positive correlation between MAP and the CrSO2 is presented in Figure 3, and also between SaO2, CrSO2 and CvSO2, that is presented in Figure 3. Figure 3 showed significant difference between the value of CrSO2 in the survivors (29 patients) and the non-survivors (11 patients) throughout 72 hours from admission as it was statistically significant (p<0.001) (Table 1).
| Time (hr) | CrSO2 value Survivors (29) | CrSO2 value Non-Survivors (11) | T Test value | p value |
|---|---|---|---|---|
| 0 | 58.10 ± 3.63 | 50.51 ± 2.16 | 6.47 | <0.001 |
| 6 | 58.08 ± 3.12 | 50.37 ± 3.39 | 6.81 | <0.001 |
| 12 | 59.80 ± 3.46 | 50.84 ± 2.84 | 7.64 | <0.001 |
| 18 | 60.01 ± 3.73 | 50.87 ± 3.21 | 7.16 | <0.001 |
| 24 | 62.74 ± 4.45 | 52.20 ± 2.42 | 7.40 | <0.001 |
| 30 | 67.93 ± 2.50 | 60.73 ± 2.95 | 7.73 | <0.001 |
| 36 | 61. 84 ± 5.26 | 52.83 ± 3.42 | 5.25 | <0.001 |
| 42 | 61.51 ± 4.00 | 51.94 ± 2.96 | 7.19 | <0.001 |
| 48 | 66.59 ± 8.20 | 49.59 ± 2.38 | 6.86 | <0.001 |
| 54 | 62.06 ± 4.96 | 49.55 ± 3.47 | 7.63 | <0.001 |
| 60 | 64.70 ± 7.53 | 49.88 ± 3.58 | 6.22 | <0.001 |
| 66 | 66.29 ± 6.90 | 50. 57 ± 5.31 | 6.80 | <0.001 |
| 72 | 65.00 ± 8.37 | 49.64 ± 4.25 | 5.78 | <0.001 |
Table 1: Cerebral oximetry between survivors (n=29) and non-survivors (n=11). T test = Students’ t test. P= Probability. P value <0.05 = statistically significant.
The Near Infrared Spectroscopy (NIRS) was used to estimate cerebral oxygenation in our study. The dual-probe device we used measures the percentage of oxyhemoglobin to total haemoglobin in the mixture of arteries, capillaries, and veins of the cerebral circulation in a slice of tissue approximately 2 cm [6]. Currently, NIRS oximetry is widely used for the non-invasive monitoring purposes of brain oxygen saturation and the maintenance of CrSO2 values within target ranges as a clear therapeutic goal supported by evidence in the literature [8,9].
In the current study, we highlight other new advantages of NIRS monitoring in circulatory shock (septic) as a continuous monitor and as an outcome predictor. The most important observation from this study is the significant correlation between NIRS oximetry readings and hemodynamic variables, especially lactic acid, central venous oxygen saturation (CvSO2) in patients experiencing shock. These data, therefore, propose a method for rapid and non-invasive assessment of circulatory status in patients experiencing shock.
In a similar study done by P Ostadal et al. [10], which was conducted specifically on 10 patients with cardiogenic shock and patients on Extracorporeal Membrane Oxygenator (ECMO) support, they found strong correlations between CrSO2 and systemic vascular resistance index (SVRI) (r=-0.47; P=.0001), but not MAP. Those results are matching with our study where a good correlation was also found between CrSO2 with MAP, but SVRI was not included in our study as we were recruiting patients with different categories of shock (septic, cardiogenic, and mixed) with variable trends of SVRI.
Good correlation between the CrSO2 and MAP was observed in another study done by Hershenson et al. [11] on 30 patients with supraventricular tachycardia in which the changes in hemodynamic were correlated linearly with CrSO2. Changes in systolic blood pressure, diastolic blood pressure, and MAP were correlated positively with changes in NIRS, as denoted by I values of 0.52, 0.57, and 0.67, respectively, and a p value less than 0.05 for all 3 association tests.
Many other studies [12,13] are using NIRS technology to study the correlation between the peripheral oxygen saturation recorded from the thenar eminence by tissue oximetry and Cardiac Index (CI) or MAP and other hemodynamic parameters in patients with severely hypotensive shock; but, we believe that the expected hypoperfusion in the peripheral circulation during shock will definitely affect the accurate measurement in the peripheries and at least from the theoretical point of view that monitoring the cerebral circulation should be more valuable and appealing, which represents one of the important positive point related to the novelty of this study as the use of CrSO2 as a monitoring tool in shock is not yet explored in the current publications; but, we believe that the literature will carry a lot of studies in the field and maybe the growing evidence will put this newly studied tool as a part of the routine practice in hemodynamic monitoring.
Alejandro Rodriguez et al. also studied that septic shock patients with forearm skeletal muscle rSO2 ≤60% throughout first 24 hours after ICU admission had significantly greater mortality [14].
One study, closely resembles to this study, by Tayar AA [15] et al. showed strong correlation between CrSO2 (measured by INVOSTM Oximeter 5100C) with other perfusion parameters like lactate, CvSO2, MAP in a population of 20 patients. They also showed significant difference between the value of CrSO2 in the survivors (12 patients) and the non-survivors (8 patients) after 72 hours from admission was noted, but The results in the first hours up to 3 days were not significantly different. But our study showed significant difference (p<0.001) from 1st hour to 72 hours (Table 2).
| CrSO2 | Lactate | CvSo2 | SaO2 | MAP | |||||
| 0 hr | -0.956 | <0.001 | 0.993 | <0.001 | 0.988 | <0.001 | 0.976 | <0.001 | |
| 6 hr | -0.946 | <0.001 | 0.976 | <0.001 | 0.973 | <0.001 | 0.966 | <0.001 | |
| 12 hr | -0.938 | <0.001 | 0.982 | <0.001 | 0.981 | <0.001 | 0.99 | <0.001 | |
| 18 hr | -0.899 | <0.001 | 0.981 | <0.001 | 0.972 | <0.001 | 0.988 | <0.001 | |
| 24 hr | -0.876 | <0.001 | 0.904 | <0.001 | 0.981 | <0.001 | 0.982 | <0.001 | |
| 30 hr | -0.937 | <0.001 | 0.972 | <0.001 | 0.98 | <0.001 | 0.965 | <0.001 | |
| 36 hr | -0.767 | <0.001 | 0.967 | <0.001 | 0.888 | <0.001 | 0.97 | <0.001 | |
| 42 hr | -0.865 | <0.001 | 0.986 | <0.001 | 0.95 | <0.001 | 0.987 | <0.001 | |
| 48 hr | -0.831 | <0.001 | 0.982 | <0.001 | 0.982 | <0.001 | 0.993 | <0.001 | |
| 54 hr | -0.862 | <0.001 | 0.989 | <0.001 | 0.962 | <0.001 | 0.967 | <0.001 | |
| 60 hr | -0.79 | <0.001 | 0.979 | <0.001 | 0.864 | <0.001 | 0.988 | <0.001 | |
| 66 hr | -0.808 | <0.001 | 0.988 | <0.001 | 0.927 | <0.001 | 0.957 | <0.001 | |
| 72 hr | -0.749 | <0.001 | 0.977 | <0.001 | 0.869 | <0.001 | 0.986 | <0.001 | |
| r value | p value | r value | p value | r value | p value | r value | p value | ||
CrSO2-Cerebral oximetry; CvSO2-Central mixed venous oxygen saturation; SaO2-Arterial Oxygen saturation; MAP-Mean arterial pressure; r-Pearson correlation coefficient; p-Probability. p value <0.05=statistically significant
Table 2: Correlative value of cerebral oximetry with different other parameters.
Another study by O. Tatli, O. Bekar et al. showed in 2017 that cerebral oximetry monitoring shows significantly low CrSO2 value in brain dead patients [16-18].
Aamer Ahmed, Giovanni Mariscalco narrated in a study in 2017 that cerebral oximetry monitoring significantly improve cardiovascular outcomes and length in hospital stays [19,20].
Anneliese Moerman and Stefan De Hert in 2015 shows that in a variety of surgical patients’ cerebral oximetry measurement improves outcome in both neurological point of view and organ mobility [21-23].
Our study had several limitations. Cardiac invasive monitoring should be done for studying patient with septic shock. But no such monitoring was used in our study. If it was done the correlation will have much stronger value with significance. Another thing is that this study is containing only 40 patients in a single cantered base pilot study. So, for globally validating this results study should contain much larger population and multi centre well organised larger trial to be done.
Cerebral regional oxygen saturation might be helpful as one of the perfusion parameters in patients with septic shock; it also informs us tissue oxygen saturation in real time and also the trends of the same. This parameter could have been used as a prognostic value in prediction of mortality in those septic shock patients.
Citation: Das D, Mitra K, Das S (2021) Brain Co-oximetry: An Useful Non-Invassive Parameter Adjuvant to Standard Perfusion Parameters in Septic Shock. J Anesth Clin Res. 12: 987.
Received: 14-Jan-2021 Accepted: 28-Jan-2021 Published: 04-Feb-2021 , DOI: 10.35248/2155-6148.21.12.987
Copyright: © 2021 Das D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.