Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2019)Volume 10, Issue 2
This case represents a very rare manifestation of leukemia cutis and highlights the importance of both routine physical examination and the suspicion of immunologic reaction in these patients.
Leukemia cutis; Kobner phenomena; Acute myeloid leukemia; Blasts
A 70 y/o female with a history of diabetes mellitus was previously diagnosed with normal karyotype NPM1-mutated acute myeloid leukemia. She was given induction chemotherapy with 7+3, which was followed by 3 courses of consolidation with intermediate dose cytarabine. Molecular remission was documented soon after induction chemotherapy. Eight months before current admission her disease recurred with documented FLT3-ITD (allelic ration 1:1). Her disease did not respond to salvage chemotherapy, however she achieved a second complete remission with a combination of venetoclax, azacitidine and sorafenib. A month before admission the leukemia recurred. The patient was admitted for allogeneic HCT from 10/10- HLA identical unrelated donor. The conditioning regimen was based on the FLAMSA protocol. In addition, the patient was given a sliding insulin scale with long term insulin (lantus) and short term insulin (apidra).
Soon after starting insulin, she developed a painful hemorrhagic purpura confined to the injection site (Figure 1A). She was given a broad spectrum antibiotic, however the event recurred in every injection site and a skin biopsy was performed. Histopathological evaluation showed a diffuse lymphocytic infiltrate in the dermis and in the subcutaneous tissue, admixed with clusters of enlarged atypical cells and extravasated erythrocytes. Immunohistochemical analysis showed strong cytoplasmaic granular staining for myeloperoxidase (MPO) in the atypical cells, indicating a myeolid origin, compatible with diagnosis of cutaneous leukemic infiltrate (Figure 2). Soon after completion of the preparative regimen, all previous lesions disappeared and no new lesions were documented at new injection sites (Figure 1B).
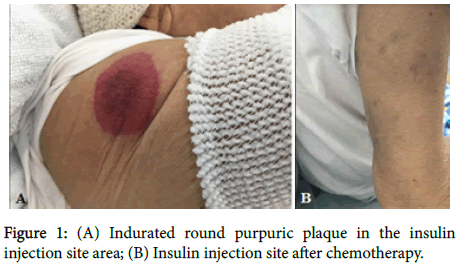
Figure 1. (A) Indurated round purpuric plaque in the insulin injection site area; (B) Insulin injection site after chemotherapy.
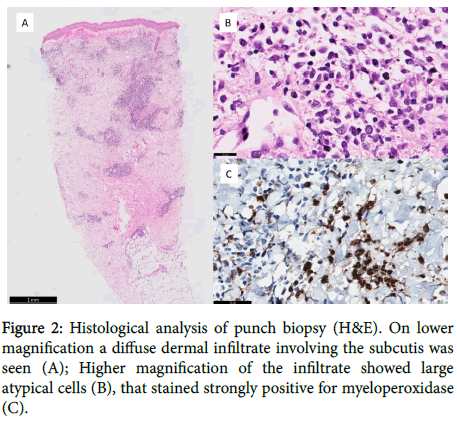
Figure 2. Histological analysis of punch biopsy (H&E). On lower magnification a diffuse dermal infiltrate involving the subcutis was seen (A); Higher magnification of the infiltrate showed large atypical cells (B), that stained strongly positive for myeloperoxidase (C).
Acute leukemia may present in a variety of extramedullary tissues with or without bone marrow disease. Extramedullary leukemia is a relatively rare, but clinically significant, phenomenon that often poses therapeutic dilemmas. Leukemia cutis, the infiltration of the epidermis, dermis, or subcutis with leukemia cells, complicates 5-10% of cases of acute myeloid leukemia in adults and is considered a marker of poor prognosis [1]. The survival rate is 30% at 2 years in patients with Acute Myeloid Leukemia (AML) without skin lesions as compared to 6% in patients with skin lesions indicating grave prognosis of leukemia cutis [2]. The majority of leukemia cutis occurs at presentation with systemic leukemia (23-44%) or in the setting of an established leukemia (44-77%) [3,4]. While several cases of cutaneous leukemic infiltration have been previously reported confined to inserted central lines areas, to the best of our knowledge this is the first report of leukemia cutis limited only to injection sites that has completely resolved after starting chemotherapy [5,6].
The pathophysiology of the specific migration of leukemic cells to the skin is not clear. It has been speculated that the chemokine integrin and other adhesion molecules may play a role in skin specific homing of T and B leukemic cells [7]. Two pathologic mechanisms may explain this phenomenon. Allergic reaction at injection site is a common phenomenon and both normal immunologic cells as well as "bystander" leukemic blasts may be involved; however, in this case, we would presume that after clearance of the leukemia, injection site allergic reactions will be still documented. Alternatively, we hypothesize that leukemic cells either spread to the site of insulin injection by a Koebner-like phenomenon. Koebner's phenomenon is represented by a skin alteration induced by several kinds of nonspecific trauma such as burn scars, surgical wounds, injections, and so on. Associations with numerous systemic disorders, including malignancies of the hematopoietic system have been reported [8]. The pathogenesis of the Koebner phenomenon involves inflammatory cells and local production of various cytokines and adhesion molecules like CD56 and TGF-β1 [7,8]. Both are able to create a microenvironment that promotes the induction of migration and infiltration of leukemic cells to the skin.
In summary, this case represents a very rare manifestation of leukemia cutis and highlights the importance of both routine physical examination and the suspicion of immunologic reaction in these patients.
Citation: Luttwak E, Zeeli T, Werner VZ, Ram R (2019) "Blast off" Dermatitis. J Clin Exp Dermatol Res 10: 483. doi:10.4172/2155-9554.1000483
Received: 26-Dec-2018 Accepted: 31-Jan-2019 Published: 11-Feb-2019
Copyright: © 2019 Luttwak E et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Sources of funding : GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).