International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Case Report - (2020)Volume 8, Issue 5
Necrotizing vasculitis in rheumatoid arthritis (RA) can lead to different patterns of neuropathy, including entrapment neuropathies, mononeuritis multiplex and distal symmetric sensory or sensorimotor neuropathy.
82 years old Female with Past medical history of Hypertension, presented with painless swelling of the right elbow for 1-year duration associated with inability to fully extend the elbow and inability to hold objects with both hands. She denies any numbness or tingling of upper or lower extremities. No history of neck pain, no history of any other joint pain or swelling. No difficulty of ambulation and no urinary or bowel incontinence. No fever or weight loss [1].
Physical exam revealed purplish rash and livido-reticularis over the extensor aspect of both elbows and wrists. Non-tender Swelling of both wrists with synovial thickening, ulnar deviation and volar subluxation of Metacarpophalangeal joints (MCP) (Figure 1).
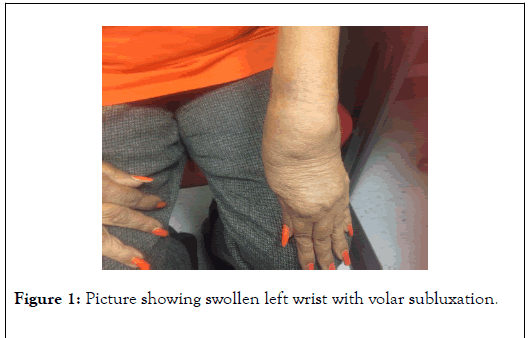
Figure 1. Picture showing swollen left wrist with volar subluxation.
Non-tender soft swelling of right elbow joint with flexion deformity 45 degrees. Neurological exam Revealed; marked wasting of both thenar, hypothenar and small muscles of the hands. Intact Sensation of all extremities.
Negative Tinel sign and Phalen test for both median nerves. Upper and lower DTJ G2.MMT: Thenar and, Hypothenar G2/5 bilaterally. Small muscles of both hands G1/5, Long flexors 3/5bilaterally, all remaining muscles 5/5. Her Gait was normal.
Laboratory tests revealed elevated ESR and CRP, normal renal and liver function, positive RF, ANA, and Anti-CCp, Negative Anti DSDNA, normal C3 and C4 level, low serum iron, elevated TIBC, low hemoglobin. MRI right elbow showed advanced arthritic changes with large effusion and diffuse synovitis.
Nerve conduction study revealed reduced CMAP of both median, both ulnar, and right tibial nerve. EMG revealed abnormal rest potentials of both first dorsal interosseous muscles.
The patient presented for the first time by manifestation of advanced RA in the form of swelling of the wrists with synovial thickening and ulnar deviation and volar subluxation of MCP joints as well as swelling of the elbow with flexion deformity.
Also, the laboratory findings suggested severe sero-positive RA together with MRI of right elbow which showed advanced arthritic changes with effusion (Figure 2).
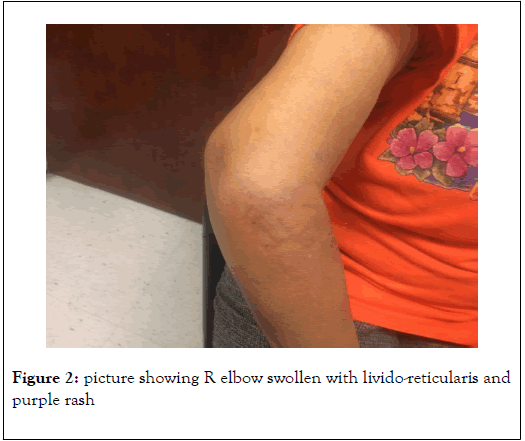
Figure 2. Picture showing R elbow swollen with livido-reticularis and purple rash
The patient also had a manifestation suggesting rheumatoid vasculitis as purplish rash and livido-reticularis, weakness and wasting of small muscles of both hands which was evidenced by nerve conduction studies as axonal motor neuropathy with sparing of the whole sensory nerves.
The patient was not complaining of any sensory manifestation and her sensory exam was intact. In the contrary, the swelling of right elbow as well as the wrists were totally painless although the inflammatory parameters as indicated by C-reactive protein and sedimentation rate were high. This suggests local affection of the joint innervation by neuropathy as part of the manifestations of the vasculiticneuropathy.
Although sensory nerve conduction for both median and ulnar were intact, but the innervation of normal joint is not amenable to testing by nerve conduction study.
Elderly-onset rheumatoid arthritis (EORA) defined as rheumatoid arthritis with onset age at 60 years or over. It is characterized by a higher frequency of acute onset with systemic features, higher disease activity, more radiographic damage and functional decline [2].
Incidence of rheumatoid vasculitis (RV)is approximately 2-5% among those having rheumatoid arthritis (RA) [3-6]. Vasculitic neuropathy is a frequent complication of rheumatoid vasculitis1,7. It results from inflammation of vasa nervosa [7].
Approximately 40% of patients with RV have sensory neuropathy and up to 20% develop manifestation of a mixed motor and sensory neuropathy (Figure 3). Both mono-neuritis multiplex and distal symmetric sensory or sensorimotor neuropathy can occur [8,9].
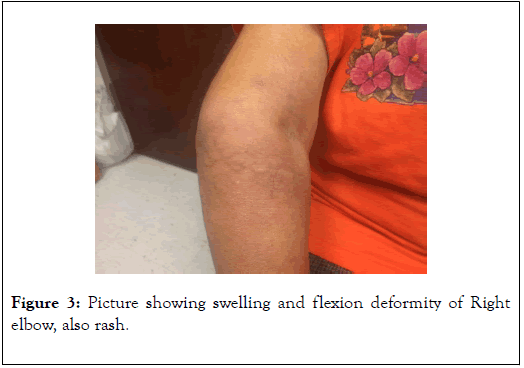
Figure 3. Picture showing swelling and flexion deformity of Right elbow, also rash.
Joints are supplied by both primary and accessory nerves. Primary nerves are branches of peripheral nerves passing near to the joint, whilst accessory nerves are branches of intramuscular nerves crossing the joint capsule.
Some joints such as the knee and ankle receive a nerve supply from cutaneous nerves in the overlying skin. The articular nerves are less than 5 μm in diameter; those that are less than 2 μm in diameter are unmyelinated. These fibers carry nociceptive information with a slow conduction velocity [10].
Evidently this above-mentioned patient suffered from elderly onset RA complicated with Rheumatoidvasculitis that affect her skin as well as her motor nerves resulting in axonal pure motor neuropathy. The painless elbow and wrist joint swelling although with evidence of severe inflammation supposed to be severely painful. This could be explained by affection of the joint innervation by the vasculitis neuropathy process, as that could not be obtained by routine nerve conduction study.
The presence of pure motor neuropathy is unusual form in case of vasculitis neuropathy as it is usually either sensory or sensorimotor. But in this case the patient has no subjective or objective sensory deficit, but instead presented with pure weakness i.e. motor manifestation. Although affection of the nerves of the joint could still be sensory nerve affection but these nerves cannot be tested by nerve conduction studies.
This Case presented an elderly onset rheumatoid arthritis complicated with vasculitis manifested by pure axonal motor neuropathy and skin affection.
Citation: Hussein N, Victor Nwopara (2020) Axonal Motor Neuropathy in Rheumatoid Vasculitis: A Case Report. Int J Phys Med Rehabil. 8:562. DOI: 10.35248/2329-9096.20.08.562
Received: 06-Aug-2020 Accepted: 12-Aug-2020 Published: 21-Aug-2020 , DOI: 10.35248/2329-9096.20.08.562
Copyright: © 2020 Hussein N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.