International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2021)
Stroke mechanism of Medullary Infarction (MI) mainly consists of penetrating artery disease (PAD), Large Artery atherosclerotic Occlusive Disease (LAOD) and dissection. The prevalence of stroke mechanism and its correlation with long-term outcome was previously reported. The prevalence of stroke mechanism and its correlation with longterm outcome has been studied. One hundred seven patients with acute isolated medullary infarction including 71 patients with LMI and 36 with MMI from the registration of 3820 consecutive acute ischemic stroke patients were selected. PAD was the most predominant cause and tended to show favorable functional outcome than other two mechanisms. Patients with LAOD showed poor functional outcome one year after onset in both groups of LMI and MMI. Although dissection in LMI exhibited worse functional state in acute phase, it did not show long-term poor outcome. Spontaneous early improvement of luminal narrowing in dissection may contribute to this finding. Atherosclerotic vertebral artery occlusive disease may expose ischemic insults to persistent hemodynamic compromise status. In patients with LAOD, the aggressive medical management or strict control of vascular risk factors should be considered.
Medullary infarction; Hypo-perfusion; Dysphagia
Previously a brief study has been done on the stroke mechanism of medullary infarction (MI) and their correlation with functional prognosis [1]. Findings were that Penetrating Artery Disease (PAD) was the most predominant stroke mechanism and showed favorable outcome compared with Large Artery atherosclerotic Occlusive Disease (LAOD) and dissection. Continuous hypo-perfusion status in patients with LAOD and dissection may lead to more extensive ischemic insult during a long period.
However, accumulating more patients after previous reports, it was revealed that patients with dissection exhibited more favorable outcome than previously experienced. Since the previous study, we subsequently collected more consecutive patients and analyzed again in terms of stroke mechanisms and their functional outcome.
Subjects
One hundred seven patients with acute isolated medullary infarction including 71 patients with LMI and 36 with MMI from the registration of 3820 consecutive acute ischemic stroke patients were selected.
Patients were prospectively registered who entered hospital within 5 days of onset in the Kyoto Second Red Cross Hospital from January 2009 through September 2019.
Patients were prospectively registered who entered hospital within 5 days of onset in the Kyoto Second Red Cross Hospital from January 2009 through September 2019.
Data collection
The following data were calculated: age, sex, clinical features, including National Institute of Health Stroke Scale (NIHSS) on admission and discharge, symptom progression after admission and modified Rankin Scale (mRS) ≥ 2/ dysphagia one year after discharge [2]. The Institutional Review Board of Kyoto Second Red Cross approved this study and informed consent was obtained from all patients.
Evaluation of vascular lesions and presumed stroke mechanism
Magnetic resonance imaging and Computed Tomography Angiography (CTA): All patients had MRI and Magnetic Resonance Angiography (MRA). MRI scans were performed using 1.5-T superconducting magnets (Gyroscan Intera Achieva 1.5 Pulsar, Philips). Each MRI was performed within 3 days after stroke. Diffusion-weighted scans (TR 1861 ms/TE 69 ms, EPI factor 37) and Fluid Attenuated Inversion Recovery (FLAIR) scans (TI 2000 ms, TR 6000 ms, TE 120 ms) were obtained at a slice thickness of 5 mm. Three-dimensional time-of flight images were acquired in the axial plane with a repetition time of 25 ms, echo time of 6.9 ms, flip angle of 18º, 210-mm field of view, partition of 64, 219 9 512r acquisition matrix and one signal average, for a total imaging time of 4 min 33 s. All patients had MRI and Magnetic Resonance Angiography (MRA). MRI scans were performed using 1.5-T superconducting magnets (Gyroscan Intera Achieva 1.5 Pulsar, Philips). Each MRI was performed within 3 days after stroke. Diffusion-weighted scans (TR 1861 ms/TE 69 ms, EPI factor 37) and Fluid Attenuated Inversion Recovery (FLAIR) scans (TI 2000 ms, TR 6000 ms, TE 120 ms) were obtained at a slice thickness of 5 mm. Three-dimensional time-of flight images were acquired in the axial plane with a repetition time of 25 ms, echo time of 6.9 ms, flip angle of 18º, 210-mm field of view, partition of 64, 219 9 512r acquisition matrix and one signal average, for a total imaging time of 4 min 33 s.
CTA was performed for five patients with dissection. The patient receives an intravenous injection of contrast and then the head and neck were scanned using a high speed CT scanner. When vessel imaging was unclear, digital subtraction angiography was performed for three patients with .dissection.
Vascular lesions were assessed on MRI, MRA, CTA or conventional angiography. The stenosis degree in the vertebral artery was categorized into 3 groups: Normal or mild stenosis (<50% diameter reduction), severe stenosis (≥ 50% diameter reduction) and occlusion (non- visualization of artery). Dissection was diagnosed when such imaging findings were found as double lumen, intimal flap, intramural hematoma, pearl and strings or fusiform or irregular aneurysmal dilation with rapid change in morphology [3].
The presumed stroke mechanisms based on vascular lesions were defined as follows: 1. Penetrating Artery Disease (PAD); intrinsic artery disease or branch atheromatous occlusion of penetrating arteries that arise from the vertebral artery or basilar artery [4,5]. When the vertebral artery on the affected side was normal or mild stenosis (<50%), PAD was diagnosed. 2. Large Artery Occlusive Disease (LAOD); when severe atherosclerotic stenosis (≥ 50%) or occlusion on the vertebral artery in the affected side. 3. Dissection; when angiographic findings of the vertebral artery consistent with dissection. 4. Cardiogenic Embolism (CE); when there was atrial fibrillation without large artery occlusive disease and symptoms occurred abruptly.
Functional evaluation and neurological sequelae: All of the patients were evaluated for neurological severity based on the NIHSS on admission and discharge. Long term functional outcome was evaluated using the mRS and the presence of dysphagia [1,2]. Progression or worsening in acute phase was defined as more than 1 point increase on NIHSS during 5 days after admission. Those who showed the mRS ≥ 2 and/or dysphagia at one year after onset were defied as poor outcome. Most patients’ outcomes were confirmed by their outpatient clinic or transferred hospital. Although dysphagia is not counted into mRS, it may be one of the serious neurological sequelae that afflict patients. We thus set the significant neurological sequela index as a condition that includes the mRS ≥ 2 and/or dysphagia.
Statistical analysis
Pearson’s chi-square test and Kruskal-Wallis test were performed to compare the clinical features among different stroke mechanism groups setting the PAD group as a reference. All statistical analyses were performed using JMP 12 software (SAS Institute Inc., Cary, NC).
The demographics and neurological functional status in different stroke mechanism groups were given in the Table 1.
| LMI (n=71) | |||||||
|---|---|---|---|---|---|---|---|
| Stroke mechanism | PBD | LAOD | p value | DIS | p value | CE | p value |
| 20 (40.0) | 11 (22.0) | - | 18 (36.0) | - | 1 (2.8) | - | |
| Age (mean ± SD) | 61.7 ± 17.8 | 69.2 ± 13.2 | - | 52.7 ± 13.4 | 0.039 | 81 ± 5.0 | - |
| Male | 15 (51.7) | 12 (75.0) | - | 18 (75.0) | - | 1 (100) | - |
| NIHSS on admission | 2 [1-3] | 2 [1.25-4] | - | 3 [1-5] | 0.022 | 3 [1-5] | - |
| NIHSS on discharge | 1 [0-1.5] | 2 [0.25-3] | 0.056 | 1.5 [1-3.75] | 0.0104 | 4 [2.5-4] | - |
| acute worsening | 2 (6.9) | 8 (50.0) | 0.0009 | 8 (33.3) | 0.014 | 0 | - |
| mRS ≥ 2 and/or dysphagia at 1 year after onset | 3 (10.3) | 7 (43.7) | 0.0099 | 6 (25.0) | 0.15 | 1 (50.0) | - |
Table 1: Characteristics in patients with LMI. Age is expressed as mean (standard deviation). NIHSS on admission and discharge were expressed as median (range). Other items mean number (%).
In LMI group, the scores of NIHSS on admission were not different between PAD and ATBI but the prevalence of poor outcome was clearly higher in ATBI than in PAD.
On the other hand, although NIHSS on admission and discharge or the prevalence of acute worsening were higher in dissection than in PAD, functional outcome after one year was not significantly different between dissection and PAD (Table 2).
Vertebral-artery occlusion accounted for 87.5% among total 24 patients with LAOD. Both groups of LAOD and dissection showed acute worsening more frequently than PAD, being more frequent in LAOD than in dissection (Tables 1 and 2).
| MMI (n=36) | |||||||
|---|---|---|---|---|---|---|---|
| Stroke mechanism | PBD | LAOD | p value | DIS | p value | CE | p value |
| 20 (55.5) | 13 (36.1) | - | 2 (5.6) | - | 1 (2.7) | - | |
| Age (mean±SD) | 72.4 ± 10.0 | 71.5 ± 10.7 | - | 54.5 ± 12.0 | 0.038 | 74 | - |
| Male | 12 (60.0) | 10 (76.9) | - | 2 (100) | - | 1 (100) | - |
| NIHSS on admission | 2 [1-3] | 2 [1.25-4] | 0.037 | 3 [1-5] | - | 3 [1-5] | - |
| NIHSS on discharge | 1 [0-1.5] | 2 [0.25-3] | - | 1.5 [1-3.75] | - | 4 [2.5-4] | - |
| acute worsning | 10 (50) | 4 (30.7) | - | 0 | - | 0 | - |
| mRS ≥ 2 and/or dysphagia at 1 year after onset | 3 (10.3) | 7 (43.7) | 0.017 | 6 (25.0) | - | 1 (100) | 0.012 |
Table 2: Characteristics in patients with MMI. Age is expressed as mean (standard deviation). NIHSS on admission and discharge were expressed as median (range). Other items mean number (%).
Figures 1 and 2 showed diffusion weighted images and magnetic angiography of two patients with lateral medullary infarction who showed acute worsening.
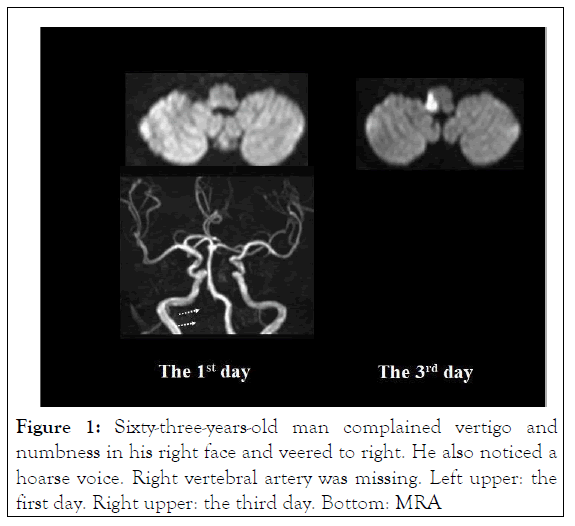
Figure 1: Sixty-three-years-old man complained vertigo and numbness in his right face and veered to right. He also noticed a hoarse voice. Right vertebral artery was missing. Left upper: the first day. Right upper: the third day. Bottom: MRA
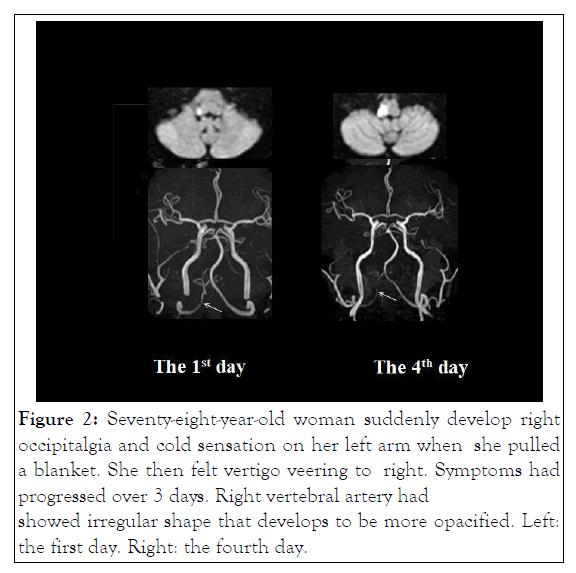
Figure 2: Seventy-eight-year-old woman suddenly develop right occipitalgia and cold sensation on her left arm when she pulled a blanket. She then felt vertigo veering to right. Symptoms had progressed over 3 days. Right vertebral artery had showed irregular shape that develops to be more opacified. Left: the first day. Right: the fourth day.
The present study demonstrated that PAD was the most prevalent stroke mechanism both in groups with LMI and MMI, accounting for 40.8% and 55.5%, respectively. The second most prevalent mechanism in LMI group was dissection accounting for 33.8%, succeeded by LAOD for 22.5%. In MMI group, LAOD was the second most frequent cause accounting for 36.1%. Patients with PAD showed better functional outcome than those with LAOD or dissection. In both groups, LAOD compared with PAD was significantly correlated with poor outcome (p=0.0009 in LMI and p=0.017 in MMI, respectively). In LMI group, interestingly, although dissection showed unfavorable functional state during admission, the prevalence of poor outcome was not different between dissection and PAD.
Thus a bit different result from the previous study was obtained by adding 26 more patients.
The observational study of Vertebrobasilar Flow Evaluation and Risk of Transient Ischemic Attack and Stroke (VERiTAS) studied 82 patients with VB atherosclerotic stenosis and/or occlusion and found that patients with low distal flow status are at higher risk of subsequent posterior circulation stroke [6]. Distal flow status was evaluated by phase-contrast Quantitative Magnetic Resonance Angiography (QMRA) [7]. Researchers presumed that low distal flow may reduce the washout of emboli leading to thrombus formation [8]. In the present study, the continuous presence of hemodynamic compromise associated with vertebral artery occlusion may predispose ischemic lesions to being irreparable, albeit no occurrence of recurrent stroke during follow-up period. Such mechanism is in line with the perfusion-weighted MRI study by Lee et al. [9]. They studied patients with medullary infarction and found patients with LAOD and dissection showed delayed perfusion, whereas all patients with PAD showed normal findings.
Of note, dissection did not show significant poor outcome different from previous results. It has been well known that the natural history of intracranial vertebral artery dissection frequently shows spontaneous angiographic improvement [10- 13]. Moreover, it was reported that VAD improvement of vertebral artery dissection primarily occurs within 6 months after onset [14]. It thus is unsurprising that patients with dissection in the present study showed relatively favorable longterm outcome compared with those with LAOD. The aggressive medical management including circulation activator and strict control of vascular risk factors may be necessary in patients with LAOD [15].
In conclusion, PAD is the most predominant cause of medullary infarction and tended to show favorable functional outcome. Patients with LAOD showed poor functional outcome one year after onset in both groups of LMI and MMI. Although dissection in LMI exhibited worse functional state in acute phase, it did not lead to long-term poor outcome. Spontaneous early improvement of luminal narrowing in dissection may contribute to this finding. Atherosclerotic vertebral artery occlusive disease may expose ischemic lesions to persistent hemodynamic compromise. In patients with LAOD, the aggressive medical management and strict control of vascular risk factors should be considered.
We have no conflict of interest.
Citation: Yamamoto Y, Makita N, Nagakane Y (2021) Atherosclerotic Vertebral Artery Occlusive Disease Predicts Poor Functional Outcome in Medullary Infarction. Int J Phys Med Rehabil. S7:001.
Received: 13-Aug-2021 Accepted: 27-Aug-2021 Published: 03-Sep-2021 , DOI: 10.35248/2329-9096.21.s7.001
Copyright: © 2021 Yamamoto Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.