Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2017) Volume 6, Issue 5
Background: Changes in the total fertility rate-lifetime births per woman have dramatic effects on population size. More than 100 million women in developing countries, or about 17 present of all married women would prefer to avoid a pregnancy but are not using any form of family planning.
Method: Cross-sectional study including both quantitative and qualitative surveys. Multistage stratified sampling was employed considering all governmental and private non health post-secondary institutions.
Result: Mothers level of education has a significant gross effect on awareness of emergency contraception (OR=0.848, P<0.01). Respondents who had no experience of communicating with their respective mother was lower by 62.6% as compared with those who had experience of discussion about reproductive health issues with their mothers (OR=0.374, P<0.001). Those who had no experience of communicating with their respective partner was less by 71.2 (OR=0.288, P<0.01) as compared to those who had no experience. Female students who never had sexual intercourse was less by 71.4% as compared with their counter parts (OR=0.286, P<0.05). Those who had no experience of discussion with their respective mothers and who had no experience of discussion with sexual partner were found less by 59.1% (OR=0.409, P<0.01) and 64.8% (OR=0.352, P<0.001) respectively. Respondents who have no intention to use modern contraceptives and who had poor knowledge of EC was less by (OR=0.272, P<0.05) and OR=0.194, P<0.01) respectively.
Conclusion: Building providers’ capacity through in-service and pre- service trainings with emphasis on methods regimen available for different products and method of teaching and counseling of clients according to the method guideline became very vital.
Keywords: Emergency contraceptive; Post-secondary school; Female students; Emergency contraception
Changes in the total fertility rate-lifetime births per woman have dramatic effects on population size and are, therefore the focus of many research, analysis and debate among demographers. Despite this increase, still the use of family planning varies widely between countries and within countries from less than 10% of women of reproductive age in some sub -Saharan countries like Mali to more than 75% in many developed countries including Mexico and Thailand [1-3]. More than 100 million women in developing countries, or about 17 present of all married women would prefer to avoid a pregnancy but are not using any form of family planning. In some countries, however, particularly in sub-Saharan Africa, unmet need remains persistently high (more than one-fifth of married women) [1-3]. Ethiopia is one of the sub-Saharan African countries expected to be the world’s 10th largest country in population by 2050 [4]. According to EDHS 2005 current contraceptive prevalence of the country is around 15% among married women which shows an increase by 7% compared with the 2000 EDHS report [5]. As shown in the EDHS 2000 the unmet need for family planning either to space or limit pregnancy is 36%, which is huge compared with other countries [5].
About 210 million pregnancies occur in the world annually; of this total, about 79 million are estimably to be unintended- either mistimed or never wanted. Of these unintended pregnancies an estimated 40- 50 million end in abortion, 20 million of which are considered unsafe. 95% of all these unsafe abortion take place in developing countries. Of the estimated 600,000 annual- pregnancy- related maternal deaths worldwide on average, 13% of all deaths are due to unsafe abortion and in some countries this number is as high as 60%. Every year, over 70,000 women die and millions more suffer injuries as a result of unsafe abortion. Mortality due to abortion is highest in Africa, 680 deaths per 100,000 procedures [6-9].
Only 13% of married adolescent age 15-19 use contraception in sub-Saharan Africa compared with 55% in Latin America and the Caribbean [1-3] 61% of sexually active women used a modern contraceptive method, yet 53% of all births were reported as mistimed or unwanted and 78% of births to women aged 19 or younger were unplanned [10]. In Ethiopia according to the survey conducted in 2000 by ESOG in nine administrative regions, 25.6% of 1075 abortion cases were induced abortions. Among them, 58% of the cases were in the age range 20-29 years. Of those pregnancies ended in abortion 60% were unplanned and 50% were unwanted. Emergency contraception involves methods of contraception used for preventing a pregnancy after unplanned or unprotected sexual intercourse.
Young people aged 15-24 years constitute about 20% of sub- Saharan Africa’s population and will, therefore, have a substantial impact on future population growth, make an understanding of the patterns of sexual behavior of young men and women a significant issue for research and policy [11]. In Ethiopia also young people aged 10-24 account 32% of the total population [1-3].
This study is designed to assess the perspective and practices of emergency contraception by female students in post–secondary institutions and male students and the provider’s perspective in Hawassa town, where number of governmental and private postsecondary institutes placed. It sought to understand the factors that affect the knowledge, attitudes and utilization of emergency contraception by this group of female students and the circumstances under which they use it.
Study design and setting
The study methodology was a cross-sectional study including both quantitative and qualitative surveys.
Sample size and sampling procedure
There are few previous studies on knowledge, attitude and practice of EC among University students in Ethiopia, based on which the sample size has been estimated [12] which is used to determine the sample size based on single population proportion.
Therefore, the sample size of the study was determined based on the assumption that:
P=proportion of awareness of EC=22.2%
Zα/2=the standard normal value corresponding to the desired level of confidence, 95% which corresponds to the value 1.96. Where α is the risk of a type I error (failing to accept the null hypothesis-false positive) usually equal to 0.05.
Zβ=the standard normal value corresponding to the desired level of confidence, 80%, which correspond to the value 0.84. Where β is the risk of a type II error (failing to reject the null hypothesis-false negative) taken as the value 0.20.
d=the effect size defined by the alternative hypothesis (the existing difference), 5% is accepted.
Power of the study is equal to 1-β which is the probability of obtaining a statistically significant P value, if a true difference exists that is equal to the effect size defined by the alternative hypothesis. Since β=0.20 the power of the study is equal to 80% (0.80).
Hence, the sample size was determined by the following Mark Woodward formula based on the above assumptions.
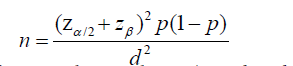
where n is the sample size (Woodward, 1992).
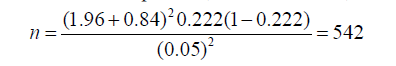
By taking additional 10% contingency for non-response rate, the total sample size would be:
542+10% (non-response rate)=596
After calculating the sample size, the multistage stratified sampling was employed considering all governmental and private non-health post-secondary institutions in Hawassa town, streams or departments and year of study in the sampling process for the selection of the study subjects. Initially, of the whole nine governmental and private non-health post-secondary institutions in the town two institutions, Hawassa College of Teacher Education (ACTE) which is governmental and the private owned institute Africa Beza University College (ABUC) were selected randomly and the total sample size of the study was distributed over each of the institute proportional to their size. In the second stage, streams for ACTE and departments for ABUC were selected using simple random sampling (SRS) technique from each selected institute and accordingly the sample size of the study allocated to each institute was distributed to each of the stream and department proportional to their size. Finally, the required numbers of female students were selected randomly (applying SRS) from each year of study again proportional to their size from the randomly selected streams and departments (Figure 1).
After obtaining the consent of respondents, the data was collected by ten trained enumerators for two consecutive days (a day for each) under the follow up of two trained supervisors and the principal investigator for its accuracy and completeness.
The data collected from the survey were entered into computer for analysis mainly using Statistical Package for Social Sciences (SPSS). The analysis part consisted of descriptive statistics (frequency and cross tabulation) and the gross effect of each predictor (independent) variable on the dependent variables was tested by crude odds ratio resulted after each individual variable has been fitted in the binary logistic regression without controlling all the other variables. Selecting the important variables, logistic regression model (multivariate analysis) was used to test the net effect of each selected predictor variable on the dependent one controlling all the other variables.
Data quality control
The primary data for the study was generated through three main tools: structured questionnaire, focus group discussion (FGD) and key informants interview. The survey questionnaire which generated the quantitative data pertaining to verify students’ knowledge, attitude and practice of EC and their socio-demographic characteristics was adapted from previous studies on EC to keep the quality of the data. The questionnaire was tested before the actual survey within a pilot survey on 40 college students to ensure its clarity, ordering, consistency and acceptance. Finally, the questionnaire was made ready after the necessary correction.
In this study, out of the total 596 female college students 38.4% of them ever had sexual intercourse with mean age 18.24 and median 18 at their first intercourse. 28.0% began sexual intercourse before age 18, 53.7% at age 18 and above and the rest did not remember or know the actual age at their first sexual intercourse. Consequently, 69% of the respondents had single partner and the rest had multiple partners during the study time (Table 1). This findings of the study explained that premarital sex among the female college students is prevalent and significant number of students also exposed to sex at early ages even with multiple partners.
| Background characteristics | Number | Percent |
|---|---|---|
| Sexual Experience | ||
| Ever had sexual intercourse | 229 | 38.4 |
| Never had sexual intercourse | 367 | 61.6 |
| Total | 596 | 100 |
| Age at first sexual intercourse | ||
| Below 18 | 64 | 28 |
| 18 and above | 123 | 53.7 |
| Do not remember/know | 42 | 18.3 |
| Total | 229 | 100 |
| Number of life time partner/s | ||
| One | 158 | 69 |
| Two | 27 | 11.8 |
| Three | 20 | 8.7 |
| More than three | 14 | 6.1 |
| Do not remember/know | 10 | 4.4 |
| Total | 229 | 100 |
| Family planning Knowledge by methods* | ||
| Oral pills | 437 | 73.3 |
| Injectables | 410 | 68.8 |
| Condoms | 387 | 64.9 |
| Calendar/rhythm | 339 | 56.9 |
| Norplant | 251 | 42.1 |
| IUD | 206 | 34.6 |
| Withdrawal | 194 | 32.6 |
| Others** | 15 | 2.5 |
| Knowing at least one method | 594 | 99.7 |
| Approval of Family planning methods | ||
| Yes | 591 | 99.2 |
| No | 5 | 0.8 |
| Total | 596 | 100 |
| Exposure to family planning methods information | ||
| Yes | 390 | 65.4 |
| No | 206 | 34.6 |
| Total | 596 | 100 |
| Ever use of contraceptive | ||
| Yes | 200 | 87.3 |
| No | 29 | 12.7 |
| Total | 229 | 100 |
| Ever used contraceptives by methods | ||
| Oral pills | 41 | 20.5 |
| Injectables | 43 | 21.5 |
| Condoms | 62 | 31 |
| Calendar/rhythm | 41 | 20.5 |
| Others*** | 13 | 6.5 |
| Total | 200 | 100 |
| Intention to use modern contraception in the future | ||
| Yes | 425 | 71.3 |
| No | 65 | 10.9 |
| Not sure | 106 | 17.8 |
| Total | 596 | 100 |
Table 1: Percentage distribution of female students of ACTE and ABUC by sexual experience, family planning knowledge and practices.
Out of the total respondents who ever had sexual experience 83.7% had ever used one of the contraceptive methods and also mentioned condoms as the most commonly used method. 49.3% of those sexually experienced respondents ever had pregnancy and the majority (69.9%) reported that their pregnancy was unplanned and 58.2% end with induced abortion (Table 1).
The study finding shows that out of all the respondents 71.3% intended to use modern regular contraception in the future and significant number of respondents (17.8%) were not sure about their future use. 10.9% of the remaining female students in the study were not interested to use any regular contraceptive method in the future because of the most commonly stated reasons, religious or moral motives (50%) and fear of side effects (32.3%) (Table 2). 49.3% of those sexually experienced female students in the study ever had pregnancy and the majorities 69.9% reported that their pregnancies were unplanned (Table 2). Of those reported having unplanned pregnancy, 29.5% failed to prevent pregnancy due to miscalculation in calendar method, 12.8% condom slippage or rupture, 56.3% never used any method because of forced sexual intercourse (12.8%), forgot to take contraception (12.8%), casual sex (19.2%) and unavailability of contraceptives(11.5%). Furthermore, out of those respondents who ever had pregnancy, 40.7% had an induced abortion while 9.7% did not response about their abortion history (Table 2). Of those unplanned pregnancies 58.2% were terminated by induced abortion, 30.4% end with unwanted live births and the situation of the rest (11.4%) remain unknown.
| History of Pregnancy and Abortion | Number | Percent |
|---|---|---|
| Ever had pregnancy (n=229) | ||
| Yes | 113 | 49.3 |
| No | 116 | 50.7 |
| Ever had unplanned pregnancy (n=113) | ||
| Yes | 79 | 69.9 |
| No | 34 | 30.1 |
| Reason for unplanned pregnancy (n=79) | ||
| Forced sexual intercourse | 10 | 12.8 |
| Calendar method was not correct | 23 | 29.5 |
| Condom slippage/ rupture | 10 | 12.8 |
| Forgot to take contraception | 10 | 12.8 |
| Casual sex | 15 | 19.2 |
| Other* | 11 | 13.9 |
| Ever had induced abortion(n=113) | ||
| Yes | 46 | 40.7 |
| No | 56 | 49.6 |
| No response | 11 | 9.7 |
Table 2: Percentage distribution of female students of ACTE and ABUC by their history of pregnancy and induced abortion.
About 212 (35.6%) of the whole respondents only ever heard about EC; 73.6% were from ACTE and the remaining 26.4% from ABUC. In addition, majority of the respondents (63.7%) who heard about EC were in the age group 20-24 (Table 3). In the two focus group discussions conducted among female students of both ACTE and ABC only five students had ever heard about ECs. The rest vast majority of the discussants were unaware of any modern product which could be taken after unprotected intercourse in order to prevent unplanned pregnancy. Whereas majority of the participants were mentioned induced abortion as the best mechanism to prevent unwanted pregnancy. Furthermore, respondents those who had ever heard about EC were asked about their first source of information about EC (Table 3). 40.1% of those female students who had ever heard about EC mentioned female friends as their first source of information about EC. Significant number of respondents also mentioned television/ radio and health care providers (each 38.2%) as their first source of information besides reproductive health clubs (24.5%), magazines and newspapers (21.2%), College clinic (17%) and boyfriend or partner (14.6%) (Table 4).
| Emergency Contraceptive Awareness | Number | Percent |
|---|---|---|
| Ever heard about emergency contraception | 212 | 35.6 |
| Never heard about emergency contraception | 384 | 64.4 |
| Total | 596 | 100 |
Table 3: Percentage distribution of female students of ACTE and ABUC by emergency contraception awareness.
| First Source of Information about EC* | Number (n=212) | Percent |
|---|---|---|
| Television / Radio | 81 | 38.2 |
| Magazines / Newspapers | 45 | 21.2 |
| Relatives | 20 | 9.4 |
| Internet webpage | 2 | 0.9 |
| From course / formal lecture | 2 | 0.9 |
| Boyfriend / Partner | 31 | 14.6 |
| Female friends | 85 | 40.1 |
| Health care providers | 81 | 38.2 |
| Campus / College clinic | 38 | 17.9 |
| Reproductive health clubs | 52 | 24.5 |
| Parents | 13 | 6.1 |
| Other sources** | 4 | 1.9 |
Table 4: Percentage distribution of female students of ACTE and ABUC by their first source of information about EC.
As shown in Table 5, 60.8% of female students who had heard about EC knew at least one correct method of EC. Furthermore, the listed traditional practices such as bitter medications and home remedies and herbal vaginal passaries were also unexpectedly mentioned as emergency contraception by 6.1% and 3.8% of respondents respectively. Awareness of the circumstances under which EC might be needed vary among respondents as shown in Table 5. Sexual assault (58%) and accidental breakage or slippage of condom (57%) were the most cited situations followed by missed pills (43.9%), miscalculation in calendar method (25.5%) and failure of contraception (17.5%) under which EC should be taken to prevent pregnancy.
| Knowledge assessment questions | Number (n=212) | Percent |
|---|---|---|
| Which can be used as emergency contraception?* | ||
| Combined oral pills | 73 | 34.4 |
| Progestin only pills/Postinor | 57 | 26.9 |
| Estrogen only pills | 32 | 15.1 |
| IUCD | 8 | 3.8 |
| Herbal Vaginal Passaries | 8 | 3.8 |
| Bitter medications (e.g. Qunine, Lemmon, Potash) | 13 | 6.1 |
| Monthly injectable | 20 | 9.4 |
| I do not know | 48 | 22.6 |
| Know at least one correct method | 129 | 60.8 |
| When should be EC taken after unprotected sexual intercourse? | ||
| Immediately after sex | 32 | 15.1 |
| Within 24 hours after sex | 39 | 18.4 |
| Within 72 hours after sex | 67 | 31.6 |
| Within 4-6 days after sex | 5 | 2.4 |
| I do not know | 69 | 32.5 |
| Drug compositions in ECPs compared to the regular contraceptives | ||
| The same as in the regular contraceptives | 42 | 19.8 |
| The same but a high doss in the same hormones | 28 | 13.2 |
| Completely different from the drug of regular contraceptives | 23 | 10.9 |
| I do not know | 119 | 56.1 |
| The mechanism of action of EC | ||
| Prevent pregnancy from occurring | 58 | 27.4 |
| Induced abortion | 39 | 18.4 |
| Prevent pregnancy and induced abortion | 22 | 10.4 |
| I do not know | 93 | 43.8 |
| Effectiveness of ECPs in preventing pregnancy | ||
| Highly effective (99%) | 45 | 21.2 |
| Three-fourth (75%) | 33 | 15.6 |
| Half (50%) | 29 | 13.7 |
| Below one third (30%) | 3 | 1.4 |
| Uncertain | 59 | 27.8 |
| I do not know | 43 | 20.3 |
| Situation(s) that EC should be taken to prevent unintended pregnancy* | ||
| When forced to have sex | 123 | 58 |
| When condom slipped or broken | 121 | 57.1 |
| When there is missed pills | 93 | 43.9 |
| When there is failure of contraception | 37 | 17.5 |
| When there is infrequent sex | 21 | 9.9 |
| When there is miscalculation in calendar method | 54 | 25.5 |
| I do not know | 52 | 24.5 |
| Other** | 1 | 0.5 |
| Know at least two situations | 140 | 66 |
| Knowledge of Emergency Contraceptive (Summary index) | ||
| Poor /No/ knowledge | 24 | 11.3 |
| Fair knowledge | 152 | 71.7 |
| Good knowledge | 36 | 17 |
Table 5: Percentage distribution of female students of ACTE and ABUC, who had heard of EC and gave responses to knowledge assessment questions regarding EC.
Out of the 212 respondents who had heard about EC, only 17.0% had good knowledge and 11.3% had no specific knowledge about the method. The remaining 71.7% of the respondents were included under the fair knowledge category. This finding reveals that detail knowledge about EC methods is lacking among college female students.
As shown in Table 6, far more than half of the respondents (80.2%) who heard about EC shown their willingness to use EC or recommend others in case of need in the future. Most of the participants of the focus group discussions accepted the availability of EC particularly for the youth at college level and also willing to use or recommend others in case of method need in the future. Far more than half (65.6%) of the respondents who had ever heard about EC had favorable attitude towards EC (Table 6).
| Indicators of Attitude | Yes (Number/ Percent) | No (Number/ Percent) | Do not know/Not sure | Total (Number/Percent) |
|---|---|---|---|---|
| EC may hurt the baby in case it does not work | 134 (63.2) | 62(29.2) | 16 (7.6) | 212 (100) |
| EC is necessary to prevent abortion and its complications | 136 (64.2) | 68 (32.1) | 8 (3.7) | 212 (100) |
| Worry about that if men knew the existence of the method, they might encourage or impose women to use it | 128 (60.4) | 73 (34.4) | 11 (5.2) | 212 (100) |
| Willingness to use EC or recommend others in case of need in the future | 170 (80.2) | 33 (15.6) | 9 (4.2) | 212 (100) |
| Attitude towards EC (Summary index) | ||||
| Favorable | 139 (65.6) | 212 (100) | ||
| Unfavorable | 73 (34.4) | |||
Table 6: Percentage distribution of female Students of ACTE and ABUC by attitude towards EC (n=212).
About 80% of female students of ACTE and ABUC who had heard about EC would like to use emergency contraceptives in the future, 15.6% would not, while 4.2% were unsure (Table 7). The commonest reason given by those intending to use ECs in future was that it is more convenient than the regular contraceptives (71.8%). On the other hand, the commonest reason (48.5%) for those without such intention were that it is dangerous to one’s health (Table 7). Of those 165 respondents having an experience of sexual intercourse without using any barrier method and never used EC, 73 (44.2%) ever had unintended pregnancy which might be terminated by induced abortion or resulted unwanted live births. Moreover, out of 106 respondents who had EC awareness but ever had an experience of sexual intercourse without using condom or any contraceptive, 48 (45%) ever had unplanned pregnancy too. This finding also suggests that significant number of female college students were highly exposed to unintended pregnancy which paves the way to an induced abortion and its complications. Female students’ awareness towards EC increases with an increase in their age and female students having urban background are more likely to be aware of EC than their counter parts. Marital status was found to be statistically significant factor of awareness of EC among female students without controlling other variables. Ever married female students were found to be 6.67 times more likely to be aware of EC than those who never married.
| Reasons | Number | Percent |
|---|---|---|
| Reasons given by the respondents who were aware of EC and planned to use it in the future (n=170/80.2%)* | ||
| It is safer than the regular contraceptives | 74 | 43.5 |
| It is more convenient than the regular contraceptives | 122 | 71.8 |
| It is more effective than the regular contraceptives | 46 | 27.1 |
| Other** | 5 | 2.9 |
| Reasons given by the respondents who were aware about EC but do not wish to use it in the future (n=33/15.6%)* | ||
| It is against my religion | 11 | 33.3 |
| It is not effective | 4 | 12.1 |
| It is dangerous to ones health | 16 | 48.5 |
| I am using a regular contraceptive method | 9 | 27.3 |
| My partner does not like it | 0 | 0 |
| It causes abortion | 2 | 6.1 |
| Other*** | 2 | 6.1 |
| Respondents who have awareness about EC but not sure to use in the future | 9 | 4.2 |
Table 7: ACTE and ABUC female students’ willingness to use EC in the future.
Respondents who were in their second year of study were found 2.29 times more likely to be aware of EC. Likewise, female students who were in their third year of study were also found 6.30 times more likely to be aware of EC. This finding also ascertained the first hypothesis that female students awareness about EC increases with an increase in their level of education (year of study). As the analysis result indicated, the likelihood of EC awareness among respondents of those who had never heard or seen information about FP methods was less by 74.5% as relatively compared with those who exposed to FP messages controlling the other variables (OR=0.255, P<0.001) (Table 8). Female students who ever had sexual intercourse were found 7.35 times more likely to be aware of EC than their counter parts. Respondents those who had ever used the regular contraceptives were found to be 11.89 times more likely to be aware of EC than those who had no experience of contraceptives. The crude odds ratio indicated that experience of pregnancy has a statistically significant positive effect on the awareness of EC among female students while the net odds ratio explained its negative association. Experience of induced abortion was found to be highly significant factor of awareness of EC when all the other variables were not controlled. Female students who had an experience of induced abortion were 5.26 times more likely to be aware of EC than their counter parts. The analysis result showed that respondents’ mothers level of education has a significant gross effect on awareness of EC (OR=0.848, P<0.01). While the other variables controlled, it was found to be insignificant factor of awareness of E.C.
| Predictor variables | Gross Effect | Net Effect (Model) | ||
|---|---|---|---|---|
| SE | Exp (B) | SE | Exp (B) | |
| Age (years) | ||||
| 15-19 (RC) | 1 | 1 | ||
| 20-24 | 0.198 | 6.065*** | 0.322 | 1.920* |
| 25+ | 0.454 | 18.132*** | 0.673 | 4.034* |
| Previous Place of Residence | ||||
| Urban (RC) | 1 | 1 | ||
| Rural | 0.225 | 0.189*** | 0.334 | 0.255*** |
| Religion | ||||
| Protestant (RC) | 1 | 1 | ||
| Orthodox Christian | 0.185 | 1.723** | 0.293 | 1.218 |
| Others§ | 0.281 | 0.703 | 0.435 | 1.351 |
| Religiosity | ||||
| Attending Regularly (RC)@ | 1 | 1 | ||
| Attending Some times | 0.275 | 2.438*** | 0.442 | 0.809 |
| Marital status | ||||
| Never Married (RC) | 1 | 1 | ||
| Ever Married | 0.272 | 6.666*** | 0.474 | 2.358 |
| Year of Study | ||||
| First Year (RC) | 1 | 1 | ||
| Second Year | 0.223 | 4.672*** | 0.321 | 2.292** |
| Third Year | 0.231 | 7.376*** | 0.391 | 6.295*** |
| Exposure to FP methods information | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.304 | 0.069*** | 0.37 | 0.255*** |
| Sexual Experience | ||||
| Ever had sexual intercourse | 0.205 | 12.899*** | 0.372 | 7.345*** |
| Never had sexual intercourse (RC) | 1 | 1 | ||
| Number of life time sexual partners | ||||
| One (RC) | 1 | |||
| Multiple | 0.323 | 0.735 | ||
| Do not remember/know | 0.669 | 0.257 | NI | NI |
| Ever used contraception (n=229) | ||||
| Yes | 0.205 | 11.889*** | ||
| No (RC) | 1 | NI | NI | |
| Ever been pregnant (n=229) | ||||
| Yes | 0.223 | 4.985*** | 0.437 | 0.297** |
| No (RC) | 1 | 1 | ||
| Ever had induced abortion (n=113) | ||||
| Yes | 0.34 | 5.261*** | ||
| No (RC) | 1 | NI | NI | |
| Respondents’ fathers level of education (n=535) | ||||
| Literate (RC)± | 1 | 1 | ||
| Illiterate | 0.232 | 0.734 | 0.424 | 0.965 |
| Respondents’ mothers level of education (n=557) | ||||
| Literate (RC) | 1 | 1 | ||
| Illiterate | 0.206 | 0.548** | 0.38 | 0.685 |
| Discussion about reproductive health issues with father (n=535) | ||||
| Yes | 0.185 | 1.384 | 0.294 | 0.963 |
| No (RC) | 1 | 1 | ||
| Discussion about reproductive health issues with mother (n=557) | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.209 | 0.374*** | 0.334 | 0.575 |
| Discussion about reproductive health issues with boyfriend /husband | ||||
| Yes | 0.199 | 9.944*** | 0.284 | 2.158** |
| No (RC) | 1 | 1 | ||
| Discussion about reproductive health issues with peers | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.306 | 0.137*** | 0.409 | 0.288** |
Table 8: The socio-demographic and other determinant variables of awareness of EC among female students of ACTE and ABUC (n=596).
As shown in Table 8, the likelihood of awareness of EC among respondents who had no experience of communicating with their respective mother was lower by 62.6% as compared with those who had experience of discussion about reproductive health issues with their mothers (OR=0.374, P<0.001) (Table 8). Whereas when the other variables controlled, its net effect was found to be insignificant. Experience of discussion with husband or boyfriend had a positive effect on EC awareness. Female college students who ever had an experience of communicating with their boyfriends or husbands on the issue of sexual matters were found 2.16 times more likely to be aware of EC than their counter parts. The likelihood of awareness of EC among respondents who had no experience of communicating with their respective partner was less by 71.2% as compared with those who had experience of discussion about reproductive health issues with their boyfriends or husbands (OR=0.288, P<0.01) (Table 8). This output also verified the third hypothesis that those female students who had an experience of communication with their friends (peers) about reproductive health issues are more likely to be aware about EC than their counter parts.
Female students following Orthodox Christian religion were found to be 2.41 times more likely to have favorable attitude towards EC than those who follow the Protestant religion. The ever married respondents were found to be 2.02 times more likely to have favorable attitude towards EC as compared with the never married one without controlling the other variables. While the other variables controlled, it was found to be insignificant factor of the attitude towards EC (Table 8).
According to the result shown in Table 9, being not sexually experienced had a negative impact on the likelihood of favorable attitude towards EC. The likelihood of favorable attitude towards EC among those female students who never had sexual intercourse was less by 71.4% as compared with their counter parts (OR=0.286, P<0.05) (Table 9). This finding ascertained the second hypothesis that sexually active female post- secondary students are more likely to intend to use EC than those who are not. Regular contraceptives experience of female students found to be a highly significant factor of attitude towards EC when the other variables were not controlled. The likely hood of favorable attitude towards EC among the respondents those who had never used the regular contraceptives were less by 82.2% as compared with those who had an experience of contraceptives without controlling the other variables.
| Predictor variables | Gross Effect | Net Effect (Model) | ||
|---|---|---|---|---|
| SE | Exp (B) | SE | Exp (B) | |
| Age (years) | ||||
| 15-19 (RC) | 1 | 1 | ||
| 20-24 | 0.337 | 1.401 | 0.569 | 0.535 |
| 25+ | 0.514 | 1.44 | 0.826 | 0.403 |
| Previous Place of Residence | ||||
| Urban (RC) | 1 | 1 | ||
| Rural | 0.408 | 0.708 | 0.547 | 0.788 |
| Religion | ||||
| Protestant (RC) | 1 | 1 | ||
| Orthodox Christian | 0.307 | 1.866* | 0.432 | 2.411* |
| Others§ | 0.527 | 1.84 | 0.778 | 6.584* |
| Religiosity | ||||
| Attending Regularly (RC)@ | 1 | 1 | ||
| Attending Some times | 0.453 | 2.169 | 0.573 | 1.38 |
| Marital status | ||||
| Never Married (RC) | 1 | 1 | ||
| Ever Married | 0.348 | 2.017* | 0.601 | 0.936 |
| Year of Study | ||||
| First Year | 0.348 | 0.924 | 0.549 | 0.951 |
| Second Year | 0.353 | 1.393 | 0.48 | 2.127 |
| Third Year (RC) | 1 | 1 | ||
| Exposure to FP methods information | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.59 | 0.303* | 0.804 | 1.027 |
| Sexual Experience | ||||
| Ever had sexual intercourse (RC) | 1 | 1 | ||
| Never had sexual intercourse | 0.334 | 0.216*** | 0.564 | 0.286* |
| Number of life time sexual partners | ||||
| One (RC) | 1 | |||
| Multiple | 0.416 | 0.858 | ||
| Do not remember/know | 1.175 | 0.997 | NI | NI |
| Ever used contraception (n=229) | ||||
| Yes (RC) | 1 | |||
| No | 0.319 | 0.178*** | NI | NI |
| Ever been pregnant (n=229) | ||||
| Yes | 0.331 | 2.627** | 0.563 | 1.824 |
| No (RC) | 1 | 1 | ||
| Ever had induced abortion (n=113) | ||||
| Yes | 0.555 | 4.548** | ||
| No (RC) | 1 | NI | NI | |
| Respondents’ fathers level of education (n=535) | ||||
| Literate (RC)± | 1 | 1 | ||
| Illiterate | 0.388 | 0.611 | 0.572 | 0.585 |
| Respondents’ mothers level of education (n=557) | ||||
| Literate (RC)± | 1 | 1 | ||
| Illiterate | 0.354 | 0.737 | 0.543 | 0.671 |
| Discussion about reproductive health issues with father (n=535) | ||||
| Yes | 0.301 | 1.335 | 0.419 | 1.584 |
| No (RC) | 1 | 1 | ||
| Discussion about reproductive health issues with mother (n=557) | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.343 | 0.409** | 0.484 | 0.408 |
| Discussion about reproductive health issues with boyfriend /husband | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.327 | 0.352*** | 0.48 | 0.822 |
| Discussion about reproductive health issues with peers | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.676 | 0.139** | 0.849 | 0.469 |
| Intention to use modern contraception in the future | ||||
| Yes (RC) | 1 | 1 | ||
| No | 0.503 | 0.227** | 0.649 | 0.272* |
| Knowledge towards EC | ||||
| Poor/No knowledge | 0.502 | 0.168*** | 0.634 | 0.194** |
| Fair knowledge (RC) | 1 | 1 | ||
| Good knowledge | 0.557 | 4.040* | 0.653 | 4.024* |
Table 9: The socio-demographic and other determinant variables of attitude towards EC among female students of ACTE and ABUC (n=596).
The odds of favorable attitude towards EC among the respondents who had an experience of pregnancy was found to be 2.63 times those who had no the experience. Whereas, controlling the other variables, the net effect of experience of pregnancy was found to be insignificant.
Without controlling other variables, the odds of favorable attitude towards EC among those respondents who had an experience of induced abortion were found to be 4.55 times their counter parts. As the result shown in Table 9, the likelihood of favorable attitude towards EC among respondents who had no experience of discussion with their respective mothers were found less by 59.1% as relatively compared with their counter parts without controlling the other variables (OR=0.409, P<0.01) (Table 9). While other variables controlled, the net effect of experience of communication with mother about sexuality issues was found to be insignificant.
Controlling all the other variables, the odds of respondents who had no experience of discussion with sexual partner was less by 64.8% than their counter parts (OR=0.352, P<0.001). Whereas, as all the other variables were controlled, its net effect has been found statistically insignificant. Without controlling all the other variables, the odds of female students who had no experience of discussion about RH matters with their peers was less by 86.1% than their counter parts (OR=0.139, P<0.01) (Table 9). Whereas, it has no significant net effect on attitude of respondents as all the other variables were controlled.
As it is shown in Table 9, the likelihood of favorable attitude towards EC among respondents who have no intention to use modern contraceptives was less by 72.8% as relatively compared with those who have plan to use regular contraception in the future when all the other variables were controlled (OR=0.272, P<0.05). Controlling all the other variables, respondents who had good knowledge of EC were found 4.024 times more likely to have favorable attitude towards EC as compared with those who had fair knowledge of EC. Correspondingly, the likelihood to have favorable attitude towards EC among those who had poor knowledge of EC was less by 80.6% as compared with those who had fair knowledge of EC (OR=0.194, P<0.01) (Table 9). This outcome verified the sixth hypothesis that the better the knowledge of EC associated with the better the positive attitude towards EC among female students.
Concerning the family planning knowledge of the respondents shows that, 99.7% of female students in the study have ever known at least one modern regular contraceptive method. While only 2 students (0.3% of the respondents) never heard about any family planning method in their life time. This result shows the existence of better awareness towards the regular contraceptives compared with the study result at Jimma University where 93.9% of the respondents had ever heard about regular contraceptives [12]. Accordingly, oral contraceptive pills (73.3%), injectables (68.8%), condoms (64.9%) and the calendar/rhythm (56.9%) were the methods most frequently mentioned by the majority of students. These findings agreed with the survey findings of [12,13] in which oral contraceptives, condoms and injectables were the most familiar methods by the respondents of their studies. Furthermore, the result also consistent with the survey finding of the Ethiopian DHS 2005, which shows that oral pills, injectables and condoms were the most widely known regular contraceptives both by women and men [5].
Of the total respondents, 99.2% approved that family planning methods prevent unwanted pregnancy and space child birth. Due to moral and religious reasons only 0.8% of the respondents refused to approve the modern family planning method. The survey finding also showed that 65.4% of female students heard about family planning information for the last six months prior to the survey. Moreover, in the study those sexually experienced female students were asked about their contraceptive use. Out of the 229 sexually experienced respondents 83.7% had ever used one of the contraceptive methods. Condoms (31.0%), injectables (21.5%) and calendar methods (20.5%) were the most commonly used regular contraception by the female students in the study. Except the injectables, condoms and calendar methods were similarly mentioned as commonly used contraception by Bahir Dar University students as reported in the study [13]. Similarly, condom (64.3%) was the most popular method used by post-secondary school students in south west Nigeria [9]. 35.6% of the whole respondents only ever heard about EC; 73.6% were from ACTE and the remaining 26.4% from ABUC. In addition, majority of the respondents (63.7%) who heard about EC were in the age group 20- 24 (Not shown). This result looks better as compared with the study findings at Jimma University on female students (22.2%) and among post abortion service seeking women of selected hospitals in Addis Ababa (14.1%), while nearly similar with the study result on female students of Bahir Dar University (34.8%) [13-15]. The female students’ awareness on emergency contraception is far less than the figures for some developing nations, 75.7% among South West Nigerian postsecondary school female students and 50% among the Kenyan female and male university students [15-17].
Correspondingly, survey findings of studies on post–secondary school female students in Nigeria and university students in Kenya cited that communication with friends was the commonest source of information about EC (33% and 17% of the respondents respectively) [18] and also a study on KAP of EC among urban family planning clients in Honduras indicated that friends/family; Television/video and radio were the leading sources of information for the method [19]. While a study result among female students of Bahir Dar University reported that television and radio as the most popular first sources of information (26.7%) followed by female friends (24.4%) [13]. Moreover, contrarily, health institutions were mentioned as the first source of information about EC among post abortion service seeking women in Addis Ababa (40.8%) while followed by friends or relatives (33.9%) [10].
Concerning the correct time for method use, the finding of this study is better than the result obtained in the study among Jimma University students (11.7%). Whereas, lower than 49.2% found in Addis Ababa among post abortion care service seeking women and 35% in Bahir Dar University [8]. Compared with some other developing nations, the finding is better than 18% found in Nigeria among female undergraduates [20] and 13% in Kenya among university students [15]. According to the survey findings, 63.2% of the 212 respondents thought that EC may hurt the baby in case it fails to work. It is a finding greater than 53.3% found in Bahir Dar University among female students [13]. The commonest reason given by those intending to use ECs in future was that it is more convenient than the regular contraceptives (71.8%). On the other hand, the commonest reason (48.5%) for those without such intention was that it is dangerous to one’s health. These findings agree with findings obtained in South West Nigeria in which similarly convenience of ECs cited by 58.5% of the respondents as the main reason for their willingness to future use, while 46.8% those having no intention to use cited as best reason as it is dangerous to one’s health [14]. Similar finding also cited by Atsede [13], that EC awareness increases as age of the respondents increase. A study on knowledge and attitude about EC in a military population of the United States Air Force revealed that older age (over 21 years) correlated with better knowledge about EC [21]. A consistent finding also cited in the study about knowledge and attitude of military population of the US Air Force as marital status had a statistically significant association with awareness of EC [21]. As the result indicated, being ever sexually experienced had a positive effect on the likelihood of awareness of EC as compared with being never sexually experienced. Female students who ever had sexual intercourse were found 7.35 times more likely to be aware of EC than their counter parts. This finding is consistent with the result obtained in the study about knowledge and attitude towards EC among teenagers in the United States that teenaged girls who are sexually experienced were more likely to have heard of ECPs than other teenaged girls [15]. Out of the total respondents who ever had sexual experience 83.7% had ever used one of the contraceptive methods and also mentioned condoms as the most commonly used method. 49.3% of those sexually experienced respondents ever had pregnancy and the majority (69.9%) reported that their pregnancy was unplanned and 58.2% end with induced abortion. According to the survey findings of this study, only 35.6% of the whole respondents heard about EC of which the majorities (63.7%) were in the age group 20-24. This is far less than the figures for some developing nations, 75.7% among South West Nigerian post-secondary school female students and 50% among the Kenyan female and male university students [14,15].
In this study only 35.6% of the female students have the awareness about EC and of these 17% only had good knowledge of EC. Consequently, the findings of this study ascertained that awareness and precise knowledge of EC among ACTE and ABUC female students is far less than from the anticipated. Lack of adequate knowledge on the method among most of the female students in this study suggests that the situation is more likely to be the worst for majority of teenagers and young adults with no or less educational attainment. Furthermore, the study findings indicate that, the promotion of emergency contraceptive methods through programs aimed at reducing unintended pregnancy and its adverse consequences among youths in general and post-secondary students in particular is very limited. Although the respondents raised their concern towards EC, majority of them (65.6%) had favorable attitude towards the method. The female students’ attitude towards EC was significantly associated with their level of knowledge about the method (OR=4.04, P<0.05) as stated by the crude odds ratio. Moreover, the extent of knowledge about EC was also found to be a highly determinant factor for favorable attitude towards the method (OR=4.024, P<0.05). The finding revealed that the likelihood of favorable attitude increased as the extent of knowledge of EC increased. Respondents those who had good knowledge of EC were found 4.024 times more likely to have favorable attitude towards EC than those who had fair knowledge on EC.
On the other hand, utilization of EC is very low despite the significant proportion of unplanned pregnancies and induced abortions as well as favorable attitude towards it. This finding strongly suggests that adequate knowledge of the method and its availability is lacking among the female students. Hence, there is a need to educate post- secondary students in particular and adolescents in general about ECs, with emphasis on the methods available, the correct time limit for use and accurate message about its effect on health. The study findings also realized that male students played a significant role in the dissemination of information about EC methods and in the decision of females to use the method. Whereas, in the focus group discussions it had been ascertained that male students were also lacking adequate knowledge of ECs even though they expressed their approval of the method availability and positive attitude for future use in need. Hence, every intervention program to enhance the current level of awareness and knowledge of EC should make male adolescents particularly students as part of it. Majority of the health service providers in this study lack a comprehensive knowledge about EC regimens. Therefore, there is also a need for building providers’ capacity through in-service and pre- service trainings with emphasis on methods regimen available for different products and method of teaching and counseling of clients according to the method guideline.
As the finding of this study declared the female students’ awareness on EC is far less than the figure among South West Nigerian postsecondary school female students (75.7%) [14]. Therefore, strategies and programs should be specifically designed to provide appropriate information and access to EC should be improved in the country in general and in post- secondary institutions in particular to enhance the appropriate awareness of EC among adolescents.
It is observed that a very wide difference between this study finding on female students’ awareness on EC and findings from countries where there are a school sex educational programs, 98% among Princeton University students [22]. This imposes to suggest the responsible bodies of the country to design sex education programs at both high school and higher institution levels.
The study result indicated that discussion within female friends about sexual matters has significant role in the promotion of modern contraception in general and emergency contraception in particular. In Kenya the well-informed students had heard of the method through peer counselor training too [15]. Thus, the academic institutions and those organizations working on RH matters should work on the promotion and enhancement of peer education or counseling among students of post-secondary institutions.
Besides the role of peer counseling and education, the media have a significant role in the dissemination of appropriate information about FP methods as stated in this study and also a study in South West Nigeria by [14]. Therefore, interventions aiming at adolescents’ RH issues including EC should use different media as the main means to broadcast appropriate information and address the target population.
However, because condoms are the only contraceptive method available that also protects against the transmission of HIV and other sexually transmitted diseases, efforts at counseling and education need to teach skills for proper condom use, to reduce the likelihood of failure particularly for college students and generally for the other youth group.
Some studies done in USA also indicated, knowledge of emergency contraception among providers increased by 53%; Which was 13.2% prior to the implementation of training programs of emergency contraception for providers and clients [22]. Therefore, there is also a need for an intervention of building providers’ capacity through inservice and pre- service trainings with emphasis on methods regimen available for different products and enhancement of their skill of teaching and counseling of clients according to the method guideline.
Use of EC among participants of this study is far less than findings of studies done in communities where awareness for EC is widespread and service is widely available, 31.4% among secondary school students in Lothian, South-east Scotland [12]. Hence, there should be an intervention designed to expand service availability particularly at college level and advance provision of dedicated ECs for potential clients especially for post- secondary students.