
Journal of Clinical and Cellular Immunology
Open Access
ISSN: 2155-9899

ISSN: 2155-9899
Research Article - (2023)Volume 14, Issue 5
Globally, remarkable progress has been made in the fight against malaria over the last two decades, yet the rate of reduction of malaria case incidence and mortality seems stalled. Globally, malaria case incidence (i.e., cases per 1000 population at risk) reduced from 80 to 58 and only to 57 in 2019. Mosquirix (RTS, S/AS01), a four-dose malaria vaccine with an effectiveness of 39%, was piloted by the WHO in three countries including Malawi where it was integrated into the EPI as a regular schedule dose. Fidelity was assessed to evaluate the degree of adherence to the planned protocol for the roll out of the program. This is a qualitative study that used the implementation fidelity framework where 12 healthcare workers were interviewed, 47 parents attended 2 focused group discussions, and a non-participatory observation checklist determined the status of vaccine storage and administration, in 2 separate health centers serving as immunization clinics. Framework approach analysis was used in this study. 59 participants were interviewed in this study. 12 health workers that were interviewed, 2 (17%) were female and 10 (83%) were male whereas all 47 (100%) parents were female. The average age of HCWs was 38 years while for the parents it was 29 years. The study demonstrated fidelity to the malaria vaccine protocol but to a much lesser extent. It has to some extent been implemented with fidelity and there is demonstrable adherence to the vaccine protocol, nevertheless, numerous gaps still exist.
Malaria; Immunization; Malaria vaccine; Vaccine administration; Mosquirix
CI: Confidence Interval; COM: College of Medicine; COMREC: College of Medicine Research Ethics Committee; COVID-19: Coronavirus Disease; DEHO: District Environment Health Officer; EPI: Expanded Program on Immunization; EPIC: Expanded Program on Immunization Coordinator; HCW: Health Care Worker; HIV: Human Immunodeficiency Virus; HSA: Health Surveillance Assistant; IDI: In-depth Interview; IRS: Indoor Residual Spraying; ITN: Insecticide Treated Net; MDHS: Malawi Demographic Health Survey; MVC: Malaria Vaccine Coordinator; MVIP: Malaria Vaccine Implementation Program; OPD: Out Patient Department; P. falciparum: Plasmodium falciparum; STI: Sexually Transmitted Infections; WHO: World Health Organization
Globally remarkable progress has been made in the past decade towards malaria control. The World Health Organization’s (WHO) World Malaria Report 2020 stated that malaria case incidence (i.e., cases per 1000 population at risk) reduced from 80 in 2000 to 58 in 2015 and 57 in 2019 globally. Between 2000 and 2015, global malaria case incidence declined by 27%, and between 2015 and 2019, it fell by less than 2%, indicating a slowing of the rate of decline since 2015. Additionally, the report further suggested that the malaria mortality rate globally (i.e., deaths per 1,00,000 populations at risk) reduced from about 25 in 2000 to 12 in 2015 and 10 in 2019, with the slowing of the rate of decline in the later years. The most prevalent malarial parasite in sub-Saharan Africa, accounting for 99% of the estimated malaria cases, remains Plasmodium falciparum.
There has been an amplified prerequisite for complementary apparatuses to lessen the disease burden and achieve a world free of malaria. In October 2015, the WHO called for pilot implementation of the RTS, S/AS01 Mosquirix™ vaccine in 3 to 5 settings in sub-Saharan Africa which include Ghana, Malawi and Kenya. The Mosquirix™ vaccine, during the phase 3 trial in children aged 5 to 17 months old, showed reduced malaria episodes by 39% (95% CI 34-43) [1]. This is a 4-dose schedule required at 5, 6, 7 and 22 months of age. Mosquirix™ was deemed safe to be administered in conjunction with other routine vaccines in the national childhood immunization programs.
Prior to the rollout, an efficacy and safety of the RTS, S/AS01 candidate malaria vaccine was conducted in Malawi from March 2009 till January 2011; children (age 5-17 months) and young infants (age 6-12 weeks) were enrolled at 11 health facilities. Correspondingly, a similar study was done in Ghana and Kenya [2]. These studies collectively reported that RTS and S/ AS01 prevented a substantial number of clinical malaria cases over a 3-4-year period in young infants and children when administered with or without a booster dose. The results of these studies demonstrated that the vaccine had the potential to make a substantial contribution to malaria control when used in combination with other preventive measures, especially in areas of high transmission [2]. This prompted the next phase-pilot the vaccine’s efficacy in the large population, hence Malawi’s decision to integrate the malaria vaccine into the EPI.
In 2019, Malawi integrated the malaria vaccine into the EPI as a regular schedule dose vaccine [1]. 11 districts were chosen participating in the program based on the high malaria burden, high extended program of immunization (EPI) coverage and high coverage of malaria interventions [3,4]. The districts include Karonga, Nkhata Bay, Ntchisi, Mchinji, Lilongwe, Balaka, Mangochi, Machinga, Phalombe, Chikwawa and Nsanje. Each of these eleven districts was further subdivided into clusters, each comprising two or more health facilities. These clusters are randomly grouped into two; half are malaria vaccine implementation areas, and the other half are serving as a comparison area (placebo). The comparison cluster sites will later obtain the vaccination upon successful implementation of the MVIP.
Implementation fidelity refers to how an intervention is delivered as planned [5]. For the vaccine to be effective and achieve the intended goal of offering protection against malaria in children, health workers must administer it or implement the pilot study on vaccine fidelity. Evaluating the program will contribute to the available literature in understanding the challenges in the post-vaccine or rollout phase. Such challenges may include side adverse side effects or, indeed high failure rate of the vaccine.
The conceptual framework of implementation fidelity applied here is composed of five elements which include: Adherence (the extent to which the delivered intervention corresponds to the designed intervention); Dosage or Exposure (the amount of an intervention received by the participants); Quality of delivery (how a staff member delivers a program); Participant responsiveness (engagement of participants in activities of the intervention); and Program differentiation (the presence of unique and critical elements of the intervention) (Figure 1) [5].
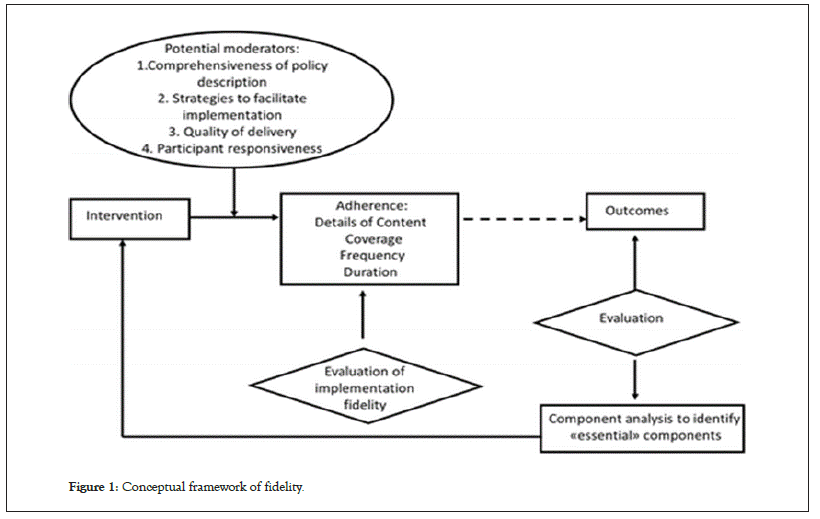
Figure 1: Conceptual framework of fidelity.
This study aimed to assess the level of fidelity of the malaria vaccine implementation program in Malawi. Further assessing the adherence of the program in Mangochi district to the malaria vaccine implementation protocol. Lastly, it also assessed the magnitude of the moderators of the malaria vaccine implementation program in Mangochi district with reference to the implementation fidelity framework.
This was a qualitative study conducted in Mangochi district. The clusters (health centers) selected for this study included Mangochi district hospital and Chiponde health center. The population was composed of healthcare workers who are currently working in the malaria vaccine implementation program and the parents/ guardians of the children that were eligible for the malaria vaccines. A purposive extreme deviant case sampling method with a maximum variation on sites (static and outreach) was administered, and all the available stakeholders were approached for better data collection. To reach a data saturation point, 12 healthcare workers were interviewed, and their data was analyzed. For the focused group discussions, all the available participants were approached to participate. Data was also collected using a structured checklist for non-participatory observations.
A formal signed written consent was sought from all the participants with an option to opt-out before the start of the interview or the discussions. A unique identification number was assigned to each recorded interview and focused group discussion and each checklist used for non-participatory observations. Recordings of the discussions were uploaded onto a computer and later transcribed using verbatim. While the in-depth were analyzed using thematic analysis. All interviews done in Chichewa were translated to English for analysis. The data collected was then transcribed (and translated where required) and analyzed using the framework analysis approach. The non-participatory observations were compared and evaluated against the checklist that the author developed through the training manual used for the training of HCWs.
Statistical analysis
We performed the statistical analysis and graphics using Analyseit software version 6.10 (Microsoft Excel add-on, Analyse-it Software, Leeds, United Kingdom). Due to the small cohort, continuous variables had a non-Gaussian distribution and are presented as medians and interquartile ranges. Categorical variables are presented as numbers and relative frequencies. For continuous variable comparisons between groups, we used nonparametric tests. For categorical variables, we used the chi-square test. We considered statistical significance at a p-value less than 0.05. We calculated BNP variability after the test as the difference between BNP at rest and BNP immediately after the stress test as a marker for the release of stored BNP. BNP variability 24 h after the test was the difference between BNP at rest and BNP 24 h after the stress test as a marker for the de novo production of BNP. We also computed BNP variability after the test and 24 h after the test.
Demographics
59 people participated in this study, out of whom, 12 were HCWs, and 47 were guardians. Of the 12 health workers were interviewed, of which 2 were female and 10 were male. While for the parents, all 47 were female. The average age of HCWs was 38 while for the guardians it was 29. All the 12 HCWs had completed a minimum of secondary education. While for the guardians, 35 had completed primary school, 11 had completed secondary education, and one had tertiary education. Additionally, 38 of the guardians were able to read and write, and nine could not do so. The average years of experience for the HCWs were 16. Additionally, 4 out of the 12 HWCs were senior HSAs. While for the guardians, 26 of them were housewives, 20 of them were self-employed (business) and one was formally employment.
Adherence to the malaria vaccine implementation protocol
This section illustrates the findings that determine the implementation protocol’s adherence and uptake with respect to the implementation framework. The tenets of the framework include commitment, dosage, quality of delivery, participant responsiveness, and program differentiation.
Knowledge and adherence
It was noted that there was some adherence to the protocols but to a lesser extent. The reasons varied from programmatic challenges to personnel. Training and orientations were not extensive; the HSAs had only one orientation session in which they were required to understand the entire protocol. This led to some parts of the protocol being adhered to, while others crucial to the study missed out by the implementers on the ground. Some of the features of the protocols that were not adhered to were during the pre-vaccination phase, where guardians were not allowed to ask questions about the vaccine; during the vaccination phase, the vaccination points didn’t have first aid kits for management of side effects. In some instances, guardians were not informed of the management of post-vaccine side effects and the supervision of vaccine providers was not done by supervisors. Health care workers during the interviews expressed knowing the study protocol. However further discussions and responses showed that they did not fully understand the protocols.
Almost all respondents, both HWCs and parents/guardians were able to describe what the vaccine is and the aims of the vaccines. Parents/guardians in the FGDs from both well performing and struggling facilities expressed satisfaction in the effectiveness of the vaccine in preventing malaria. Parents/guardians also said that they did not experience any problems with the vaccine. Most of the HCWs, especially from the well performing facility, in agreement also expressed satisfaction in malaria case reduction at the facility. This is what some HCWs and guardians had to say.
“We are seeing the number of children with malaria reduced if we compare to before. The reason is maybe the malaria vaccine” (HCW, 53, Male, Facility 1).
“I have children, and previously all used to have regular malaria as if it was contagious. But now after the malaria vaccine programs it seems as if this has changed” (Parent/Guardian, 18, Single, Female, Primary, facility 2).
Acceptance and uptake
All the HCWs expressed that there was a positive vaccine uptake by parents/guardians. HCWs attributed high uptake to the hope that parents have had for a malaria free generation of their children. Some HCWs expressed that the positive uptake is also a result of decent counseling they provide to the guardians/parents.
“The vaccine is being received well. Parents of children are happy to bring their children to get the vaccines” (HCW, 35, Male, Facility 2).
“I’m just grateful that with the malaria disease that has been problematic, those of us in this vaccination program can see some change with it…...” (Parent/Guardian, 27, Married, Female, Primary, Facility 2).
On actual uptake, not all HCWs were impressed. Some HCWs argued that just like many health care interventions, there were crucial challenges on uptake in the malaria vaccine program, particularly attributed to low literacy levels and misinformation by the public.
“One problem I would think of is probably the low literacy level of the population here in Mangochi. We can counsel women regularly and use appropriate routes through chiefs to reach out to them but comes of a surprise to us that some people claim to not know anything about the vaccine, this shows that some have a problem with understanding this program” (HCW, 29, Male, Facility 2).
One HCW, in agreement, attributed the struggle in uptake to the rollout of the program. The HCW argued that the rollout should have considered counter-information that may affect the uptake of the vaccine. He argued that the inability to deal with these incidents right from the outset resulted in challenges.
Coverage, dosage and vaccine administration
Study participants were also interviewed on eligibility, dosage, and vaccine administration. All parents/guardians from both the facilities could describe the prerequisites. Their understanding was as outlined in the study guidelines. Additionally, all HCWs were also equally able to describe the guidelines, including the procedures for enrolling a child who presents late to the facility for their first dose.
The high level of knowledge observed in the HCWs from the well performing facility was reflected in the FGDs with parents/ guardians, this however was not the case with FGD participants from the struggling facility. All parents/guardians from the well performing facilities were able to describe why their children were enrolled into the vaccine program. HCWs from underperforming facility attributed this low level of knowledge among parents/ guardians to low literacy levels.
From the observations, it was noted that although, the parents and guardians are further informed and encouraged to use ITNs and other standard preventive measures of malaria along with the vaccine. Parents and guardians were not given an opportunity to ask questions or seek clarifications for issues they had regarding the vaccine. When prompted, some parents/guardians argued that the vaccines are offered in group set-up that does not allow one to express them fully. An element of inferiority complex was also noted among clients from rural villages towards HCWs precipitating the lack of meaningful participation.
From observations, during vaccine administration, poor adherence to the protocol was reflected. Neither of the centers had a first aid kit available. The ages of the children were however verified prior to administration of the vaccine; yet crucial information such as adverse reactions to previous vaccines was not obtained. The well performing facility had ruled out contraindications to the administration of the vaccine by asking mothers if their children had ever reacted to any medicine before. However, in contrast, at facility 2, the contraindications were not ruled out.
When prompted on coverage, HCWs revealed that the district was unable to meet the set target. HCWs agreed that the low performance observed in the national aggregations were genuine however were quick to dispute that it was not entirely HCWs fault. Some HCWs argued that amongst those reached at the facility, the uptake was good, but in general there was still a problem in having the wider community accept the vaccine. Superstition and poor program implementation were the factors highlighted repeatedly by HCWs.
Storage, transport and cold chain
The study observed that the guidelines for vaccine storage were well adhered to. The temperature was within the recommended range of 2 to 8°C and vials stored away from all cold air vents. There were no other food items in the fridge. Vaccines were placed in plastic trays within the racks. During transportation, vials were placed in cold boxes with adequate ice packs. Prior to the start of the clinic, vaccine expiry dates were checked, and the vaccine vial monitor was checked to ensure viability of the vaccine. The diluent and antigen were reconstituted appropriately and used well within 6 hours of reconstitution with dedicated syringes. Almost all HCWs were able to explain in detail the processes and detailing out the technical aspects of reconstitution and transportation.
Management of side effects
Further deficiencies were observed at both sites, reflecting poor knowledge on side effects as seen in both parents/guardians and HCWs. Parents and guardians were not informed of the signs and symptoms of adverse reactions to look out for. In an observed session, the HCWs did not explain about side effects. The HCWs were just quick to say if the child falls sick, the parents/guardians should rush with the child to a health facility.
Data management
From the observations, it was noted that the immunization tally sheet, which counts the number of doses provided, is not completed following the clinic. However, the HCWs would complete it another day, usually more than two days later, which may have led to errors in documentation. This can perhaps be attributed to lack of consistent supervision noted in the study period. When asked, some HCWs argued that in some cases they run out of tally sheets while in the field, as such it was hard to document.
Assess the magnitude of the moderators of the implementation with reference to the implementation fidelity framework.
Strategies and feedback mechanisms
All HCWs reported that the program had no official feedback structures. The HCWs do know their supervisors but have never been visited by them. They relied on the knowledge they had received during their training or had to ask other HSAs for clarification when uncertain. This was more prevalent in the underperforming facility, perhaps due to the location and increased distance to the district hospital. HCWs argued that in some instances their superiors have not been a part of the team during program briefings hindering with proper supervision. HCWs from the well performing facilities cited that in cases of doubt they had human resources nearby to seek guidance from.
In addition to HCW feedback and reporting mechanism, all HCWs reported that they had no feedback mechanisms with parents/guardians. They said that the only opportune time they had with parents/guardians was during a vaccination meeting. Most of them took the initiative to ask parents/guardians if they had noted side effects or other challenges with the vaccine. Some of the HCWs from the underperforming facilities argued that they believed that for parents/guardians who are shy to ask for clarification and stay further from the facility, seeking further help when they experience side-effects and problems was low. They argued that this would negatively affect adherence to the vaccine in cases where the side effects were severe.
Increased workload and no incentives
Health care workers expressed that increased workload was a challenge. They argued that although the program was incorporated into the standard EPI programs, the work in the vaccine program was demanding, which made their overall work tiresome. This was heavily tied to the lack of incentives for HCW participation in the program. All HCWs argued that allowances during the vaccine period would motivate most of them as compensation for their increased workload. These sentiments were shared by HCWs from both facilities, with HCWs from the underperforming facility being vocal and emotional on the topic.
This is a key lesson that highlights the fact that the health workers did not fully understand that administering the malaria vaccine was part of their daily routine tasks. Therefore, clarification at the beginning of the program would have addressed the expectations of the HCWs to not perceive it as an additional responsibility. Unfortunately, the perception of administering the vaccine as an additional task requiring incentives may have had an impact on fidelity as HCWs could have cut corners because it is an additional responsibility of which they are not being compensated for.
Stock out of resources and supplies
Stock outs of resources to be used in the program were also frequently mentioned by the HCWs. Materials like syringes would often run short during their vaccination campaigns. Stockouts were discouraged parents/guardians who were adherent and those who travelled long distances; these groups were also not likely to return on the following suggested date.
From observations, stock outs were mainly due to poor planning. This was more common in the poor performing facility. HCWs argued that they depended on supplies from the district hospital, which were staggeringly replenished. In the program, tally sheets were introduced for planning purposes, and with an improper use, HCWs struggled to prepare for the next vaccination activity.
Furthermore, the deficiency in required additional IEC materials (flyers, pamphlets) also raised several red flags from the observations. Neither of the sites had the IEC materials available, nor did they have furniture to operate from. However, they did have a provision of water and soap and a safe disposal box. Each facility had a vaccine register and child health profile with inadequate malaria vaccine stickers and no calendar. From the observation notes, we noted that child health passports were available in both centers, however, neither of the centers had any of the following: under 2-year-old registers; vaccine tally sheets; guidebooks for HSAs; reference manuals; nor a vaccine vial monitoring poster.
Erratic power supply
Supply of electricity, a common problem countrywide, was also frequently mentioned. HCWs argued that frequent blackouts affect their effectiveness. This remains a major challenge if the malaria vaccine study was expanded before mitigating the power shortages.
Lack of proper training and refresher training
Lack of extensive knowledge on the vaccine that is compounded with absence of refresher courses for HCWs was also a challenge. Training period for all HSAs was scheduled for 8 weeks, but an individual HSA would only be trained within 2 days. Most HCWs agreed that the training period was short and that there was supposed to be additional training or updated SOP shared to ensure consistency in work for all HSAs. Such an approach will equip the HSAs on how to deal with challenges from the field like traditional beliefs.
Lack of sensitization and support from stakeholders
Another challenge mentioned by HCWs was lack of proper sensitization, specifically, lack of support from chiefs. HCWs argued that unlike many vaccine campaigns where chiefs were trained and tasked to sensitize locals, the vaccine program excluded chief’s involvement. Due to hierarchal traditions, it is a colossal challenge to convince parents/guardians without chiefs’ approval.
The findings of the study have demonstrated a general positive adherence to the malaria vaccine protocol, evidenced by HCW being able to explain the necessary steps. Comments by some guardians expressing knowledge of the vaccine, its purpose and even the schedule is a testimony of the same.
As presented in the findings, it is evident that HCWs are to some extent adhering to the malaria vaccine protocol. Similarly, a study by Fatiregun, et al. on missed opportunities for vaccination among children aged 0-23 months visiting health facilities in a southwest State of Nigeria found that 59% had sufficient knowledge about vaccination [6]. Despite some personnel and programmatic challenges, the health workers tried to follow the recommended protocol for the vaccine. The perception by caregivers that the malaria vaccine has led to reduction in malaria episodes among children, parents agree with other studies on vaccines that have shown that vaccines play a crucial role in reducing diseases. Furthermore, as noted in other studies, vaccination has greatly decreased the burden of infectious diseases globally and has dramatically decreased the threat of diseases that were once widespread and often fatal [7,8]. Therefore, all these are an indication that health care workers can explain to parents what the vaccine is all about, the dosage, the route of administration and side effects which suggests that the health workers were to some extent, able to adhere to the vaccine implementation protocol. Additionally, the experience acquired from administering other vaccines and Integration of the malaria vaccine protocol assisted the health care workers to properly administer the malaria vaccine.
However, it was also apparent that there were challenges with adherence to implementation protocol evidenced by some HCWs not providing adequate and correct information to parents which could have had an impact on the vaccine uptake and efficacy of the vaccines. In agreement, a study on missed opportunities and barriers for vaccination in four African countries found reluctance by health workers to open a ten-dose measles vaccine vial for a few children despite policy guidelines allowing the health workers to open the vial even for one child [9]. In the case of malaria vaccination, it may lead to the same challenges when caregivers are not provided with correct and adequate information regarding the vaccine.
Additionally, all facilities did not have first aid kit which is critical in management of any adverse effects of the vaccine. The study findings have shown that there was minimal exploration of side effects by health workers across all facilities and minimal information given to caregivers regarding side effects reflecting findings from other studies. Health workers have communicated little-to-poorly with mothers, such that some mothers leave not knowing when to return and what to do about side effects [10]. Similarly, in a study by Nkwenkeu, et al. on health worker’s perceptions and challenges in implementing meningococcal serogroup a conjugate vaccine in the routine childhood immunization schedule in Burkina Faso found that health workers were unable to engage in health education with care givers during immunizations sessions because they are overloaded with multiple responsibilities [11].
Additionally, the study findings have demonstrated that in all sites health workers had poor knowledge of the vaccine side effects. Despite this being the case, as part of the vaccine administration protocol health workers are supposed to properly explain to caregivers all the necessary information about the vaccine and unfortunately this indicates noncompliance to vaccine administration with fidelity as it is against recommended practice. Similarly, Xeuatvongsa, et al. argues that health-care workers should clearly provide information on vaccinations, including the vaccination schedule [12]. Perhaps apart from documenting the next vaccine dates in the child’s health passport, there is need for more proactive approaches by health workers in providing vaccine information to caregivers, such strategies could be playing prerecorded messages about vaccines at under 5 clinics, providing leaflets to caregivers and utilizing every opportunity a mother or care giver come to the clinic with the child, by providing information about vaccines.
Several factors have an influence on the implementation fidelity framework. As indicated, most health workers expressed little or no supervision at all which meant that even if the health workers were doing the wrong things, they had no way of knowing as there was no external observation or any kind of feedback. As earlier alluded to, workload was another factor that affected health worker’s vaccine practices which led to the health workers cutting corners for them to complete administering the vaccine so that they can attend to other tasks since apart from the malaria vaccine program; they also had to support other programs. This was also noted in another study by Nkwenkeu et al. where health workers indicated that staff shortages lead to overwork among health workers who are responsible for broad-ranging tasks including nursing care, registering children, filing records, health education, managing and administering vaccines [11,13].
Additionally, lack of routine refresher training was an issue as this meant that the health workers had no way of refreshing their skills and knowledge. Furthermore, stock outs of vaccines and erratic power supply affected the implementation of the malaria vaccine. Similar findings have been noted in other studies in Africa and Asia. Abdullahi, et al. argue that studies conducted in Asian and sub-Saharan African countries identified inadequate vaccine supply and logistics systems, insufficient human resource capacity and poorly trained and supervised managers as systemic barriers to the uptake and completion of vaccination schedules [12].
It is very clear from the findings that health workers have demonstrated fidelity despite gaps in the process, evidenced by both health workers and parents explaining the aims of the vaccine, the target group and the vaccine schedule. Further to this, the suggestions by health workers on areas that need to be improved are a demonstration of ownership and understanding of the ideal situation. Therefore, responsible government officers must put in steps to address the shortcomings in the process as per the recommendations made by the health workers and those that this study has made.
It is evident that the Malaria vaccine program has to some extent, been implemented with fidelity and there is demonstrable adherence to the vaccine protocol. Nevertheless, some gaps still exist and it is the role of the Ministry of Health through the respective health offices to learn from such experiences and employ strategies that will even increase adherence to the vaccine protocol by health workers, which ultimately will reduce the malaria burden in the country since adherence to the protocols may also lead to improved efficacy of the vaccine.
Based on this study, the authors would recommend deliberate initiatives for HCWs to undergo refresher trainings after a determined period post training. This will allow them to learn skills and experiences from colleagues, reflect on their competence, and, consequently, improve their abilities and adherence to recommended vaccine guidelines. Routine and consistent care by supervisors should be encouraged as it will provide an opportunity for feedback to the health workers, which may also motivate them to even since the presence of the supervisor indicates that their efforts are being recognized despite any existing challenges. Health education sessions within communities will play a critical role as it provides an opportunity for the health care workers to engage with parents. Consequently, any existing misconceptions about the vaccine are cleared. Further, it helps to improve the health worker’s understanding of the vaccine as they must prepare by reading and consulting with colleagues about the vaccine before giving such information to caregivers. Possible areas of further research could include, but not limited to exploring the behavioral aspects influencing the acceptability of the malaria vaccine.
The authors would like to acknowledge the hard work of Dr Robert Mkweu for the data collection, as well as Dr William Chimsanga and Dr Hudson Nyondo for their English to Chichewa translation skills employed on data collection tools.
PKP developed the research topic, introduction, literature review, worked on the discussion of the results, and developed the manuscript. LNM and NK worked on methodology sections, analysis of the results and reviewed the final manuscript.
This study possessed a low overall risk for ethical issues. College of Medicine Research Ethics Committee approval was obtained before conducting the study. Informed consent was administered, and the option to opt-out was presented to all participants for the qualitative data collection before any questions asked. The names of the participants were replaced with an identification number to protect their privacy of the participant.
This study possessed a low overall risk for ethical issues. College of Medicine Research Ethics Committee (COMREC, certificate number: P.03/20/2970) approval was obtained prior to the start of the study. Informed consent was administered, and the option to opt-out was presented to all participants for the qualitative data collection before any questions asked. The names of the participants were replaced with an identification number to protect their privacy of the participant. The data collected was password protected, and all documents were stored in a lockable cabinet to which only the researcher had access. All information was confidentially stored and accessible only to the investigator of the study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Patel PK, Nyondo-Mipando LA, Kalanga N (2023) Assessing the Fidelity of the Malaria Vaccine Implementation in Malawi. J Clin Cell Immunol.14:697.
Received: 16-Aug-2023, Manuscript No. JCCI-23-26100; Editor assigned: 18-Aug-2023, Pre QC No. JCCI-23-26100 (PQ); Reviewed: 01-Sep-2023, QC No. JCCI-23-26100; Revised: 08-Sep-2023, Manuscript No. JCCI-23-26100 (R); Published: 15-Sep-2023 , DOI: 10.35248/2155-9899.23.14.697
Copyright: © 2023 Patel PK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.