Reproductive System & Sexual Disorders: Current Research
Open Access
ISSN: 2161-038X
ISSN: 2161-038X
Research Article - (2017) Volume 6, Issue 1
Introduction: Maternal mortality can be significantly reduced in low-income settings by increasing access to skilled attendants which has close link to anti natal care, emergency obstetric care and family planning services. In spite of this clear importance of maternity care which includes anti natal care, poor access to and low utilization of such services continue to be important determinants of maternal mortality and morbidity throughout the world.
Methodology: A community based cross-sectional study was conducted in April 2015 among all women reproductive age group (15-49 years) who have had a birth in the last 12 months. A multi-stage sampling scheme was used to identify the study subjects. The kebeles of the woreda were first stratified in to semi-urban and rural kebeles. The data were collected house to house by using interviewer administered, structured, and a pre-tested questionnaire. Data were analyzed by using statistical package for social science version 20. The association and significance between the explanatory and response variables were measured using binary logistic regression analysis and finally the relative contribution of each selected variable to the outcome of interest was assessed using multiple logistic regression analysis.
Result: The overall coverage for antenatal care service utilization was 87.9% for women in their pregnancy time which is relatively good. In this study, it was found that 58.9% of women have antenatal follow up, at least 2+ antenatal care from modern health care providers and close to 37% had 4 and above visit which is below World Health Organization recommendation. It reveals that a woman without complications should have at least four focused visits to provide sufficient care. For the women of age between 35-49 years, the adjusted odd ratio is 0.178 (0.05, 0.61), educational status of mother with primary school adjusted odd ratio is 4.14 (1.06, 16.15), lack of housebound support adjusted odd ratio is 0.18 (0.07,0.44), received tetanus toxid vaccination during recent pregnancy 8.12 (2.43, 27.29), waiting time to access antenatal careless than 30 min adjusted odd ratio is 3.38 (1.08, 10.58) and 31-60 min were significant factor for anti natal utilization.
Conclusion and recommendation: Antenatal care utilization among the study participants relatively good in coverage but the pattern and timing of follow up was found to be inappropriate in most cases. Almost more than half of the mothers were started utilizing antenatal care services in their second trimester. Increasing awareness of mothers on the danger signs of pregnancy and the importance of antenatal care utilization in addressing the problem, emphasis should be given on advantage of early attendance of antenatal care with involvement of husband.
<Keywords: Antenatal care, South Omo, Ari woreda
Maternal mortality is one of the greatest development and health challenge facing by the developing world. Maternal mortality ratios have barely fallen in the last 50 years, even as other health indicators have improved. Improved maternal health is one of the key goals of millennium declaration. Target is to reduce maternal mortality by three quarters between the years 1990 and 2015 [1-3].
The share of Sub-Saharan Africa from the total death toll for developing countries is more than 50% and lifetime risk of dying from pregnancy is extremely high; that is, for every 26 mothers, one mother dies as the result of pregnancy and childbirth in Sub-Saharan Africa [4]. According to the 2011 EDHS report, the coverage of antenatal care was 34%. This varied from 76% for women residing in urban areas to 26% of women in rural areas. Even among those who use ANC, high proportions of women received care, below WHO recommendations (beginning ANC in the first trimester and making four antenatal care visits) one woman in every five mothers (19%) made four or more antenatal care visits during the course of her pregnancy and the median duration of pregnancy at the time of the first antenatal visit is 5 months. Moreover, large majority of the births (90%) in Ethiopia occur at home, and only 10% of births are delivered with the assistance of trained health professionals [5].
Child bearing is one of the hazardous experiences that women engage in while bringing new life to this world. It is often associated with complications that may cause morbidities, disabilities and mortalities. World Health Organization estimates that more than half a million women lose their lives in the process of reproduction worldwide every year; of these deaths, about 99% are from developing countries [6]. The antenatal period presents an important opportunity for identifying threats to the mother and unborn baby’s health, and for counseling on nutrition, birth preparation, delivery care and family planning options after birth [3].
Since long ago, however, it is well known that maternal mortality can be significantly reduced in low-income settings by increasing access to skilled attendants which has close link to ANC, emergency obstetric care and family planning services [3,4]. In spite of this clear importance of maternity care which includes ANC, poor access and low utilization of such services continue to be important determinants of maternal mortality and morbidity throughout the world.
This study was identified the most important factors influencing the antenatal care services utilization in study area which have demographic and socio cultural factors. However, this does not detract from the relevance of service-related factors, especially in the rural areas. The demographic and socio-cultural factors identified in this study include maternal age, education, place of residence, parity, household monthly income, distance, long waiting time and husband/ partner/disapproval of ANC etc., which are similar to those documented in many settings throughout Africa and other developing countries.
The anticipated applications of the results from this study will increase awareness of health professionals and all others concerned about the possible causes of non-attendance of antenatal care and about the utilization for planning and evaluation of maternal and child health services in the study area.
Study setting and source population
A community based cross-sectional study was conducted in April 2015 among all women reproductive age group (15-49 years) who have had a birth in the last 12 months prior the survey date, in South Ari woreda, South Omo Zone, Southern Ethiopia.
Inclusion and exclusion criteria
All women in the Age group of 15-49 years of age who have given at least one birth in last 12 months prior to the survey date. All women who were critically ill and those who could not talk or listen was not permanent resident of study area were excluded from the study.
Sample size determination
The Sample size determination for the study was computed with the assumption of confidence interval of 95%, critical value z=1.96 (from significance level α=5%) and degree of precision, w=0.05, (antenatal care prevalence was 87% study conducted in Central Ethiopia. The sample size was calculated using a formula for single population proportion.
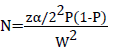
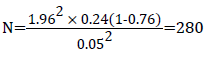
After considering 5% non-response rate and design effect of 1.5 the final sample size was 434.
Sampling methods and procedure
A multi-stage sampling method was used to identify the study subjects. Each kebele was first stratified into semi-urban and rural kebeles. From 47 kebeles (42 rural and 5 semi-urban kebeles), 10 kebeles were randomly selected by using a lottery method. Secondly, the number of households living in the area was recorded; the allocated sample size for each kebele was obtained using proportional to the size of households found in each kebele, then from ten sampled kebeles, a total of 434 study participants were selected using systematic random sampling procedure.
Data collection procedure and quality control
An interviewer administered structured and a pre-tested questionnaire was used to collect the data. Ten data collectors who completed grade 12 and above and two nurses with diploma who could speak local language were recruited, trained and assigned as data collectors and supervisors respectively. The data were collected using house-to-house interview techniques and questionnaire which consists of 37 variables, categorized into four parts. A maximal effort has been made to ensure privacy and right of participates to withdraw or refuse during interview section. The principal researchers and supervisors were around every day to control as well as to support data collectors.
Data analysis and management
Data entry, cleaning and analysis was made using SPSS version 2.0 of statically software program. All the data were coded in terms of numbers. Variables were described using descriptive statistics and frequency tables. The association and significance between the explanatory and response variables were measured using binary logistic regression analysis. The relative contribution of each selected variable to the outcome of interest was assessed using multiple logistic regression analysis.
Operational definition and definition of terms
Antenatal care: was defined as if the women had received antenatal care check-up at least once during their pregnancy from formal sources.
Antenatal care attended: pregnant women who had attended antenatal clinics during the recent pregnancy at least once.
Antenatal care non-attended women: is a pregnant woman in her third trimester and those women within 12 months of post-delivery at the time of the interview and hasn’t attended antenatal clinics at all or women who had not attended antenatal care clinics at all during her recent pregnancy.
Ethical consideration
Ethical clearance was obtained from the ethical review committee of Arba Minch University and official permission was secured from different authorities of the South Omo Zone administration and respective departments and study kebeles. The respondents were informed about the objective and purpose of the study and verbal consent was obtained from each respondent. Confidentiality of the information was maintained through meticulous training of data collectors.
Socio demographic characteristics of the study subjects
From all eligible women included in the study, 413 participants were responded correctly and completely which make response rate of 95.2%. The majority of the study participants, 208 (50.4%) were in the age group of 25 to 34 years with the mean age of 28.02 (±5.69 SD) years.
Majority of the respondents 249 (60.3%) were orthodox religion followers, and more than half (63%) of the respondents have never attended formal education. Regarding occupation, majority of women (90.8%) were house wives (Table 1).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Age of mother | 15-24 | 100 | 24.25 |
| 25-34 | 208 | 50.4 | |
| 35-44 | 96 | 23.3 | |
| 45-49 | 9 | 2.17 | |
| Educational status | Illiterate | 175 | 42.4 |
| Read & Write | 85 | 20.5 | |
| Primary School | 123 | 29.7 | |
| Secondary & above | 30 | 7.26 | |
| Ethnicity | Ari | 287 | 69.5 |
| Amahara | 43 | 10.4 | |
| Gamo | 18 | 4.4 | |
| Others** | 65 | 15.7 | |
| Occupation | House wife | 375 | 90.8 |
| Maid/servants | 7 | 1.7 | |
| Merchant | 20 | 46.5 | |
| Others*** | 11 | 2.7 | |
| Marital status | Married | 392 | 94. 9 |
| Divorced | 7 | 1.7 | |
| Widowed | 10 | 2.4 | |
| Others* | 4 | 1 | |
| Residence | Urban | 139 | 33.65 |
| Rural | 274 | 66.34 | |
| Parity | One | 52 | 12.6 |
| Two | 74 | 17.9 | |
| Three | 94 | 22.8 | |
| Four | 82 | 19.9 | |
| Five & above | 111 | 26.9 | |
| Family monthly income | 0-100 | 271 | 65.6 |
| 101-500 | 97 | 24 | |
| 501-1000 | 29 | 7 | |
| 1001 & above | 16 | 3.9 | |
| **Include-Bena, Malle, Gamo, Welaita, Mesketo, Oromo and Konso | |||
| ***Government employees, Daily laborers students, and Farmers | |||
| *Include, Single and separated couple | |||
Table 1: Socio-demographic characteristic of respondents in South Ari worda, Southern, Ethiopia, April 2015.
Respondents’ knowledge on danger signs of pregnancy
Among women who had participated in this study, most of them had knowledge on danger signs of pregnancy like hypertension during pregnancy, severe anemia, persistent vomiting, severe headache, malposition of the fetus, prolonged labor vaginal bleeding, delay and retained placenta and others. Concerning exposure to illness in the past or the recent pregnancy, the majority 209 (50.6%) have an exposure to an illness and had experienced some health problems, relatively 204 (49.4 %) didn’t experienced an illness. The majority 283 (68.5%) had perception and perceive susceptibility to dangerous health problems in the future pregnancies and while only 130 (31.50%) didn’t have such perception.
Factors associated with ANC utilization
In the binary logistic regression analysis age of mother, educational status, occupation, parity, place of residence, knowledge about danger signs of pregnancy were some of the predisposing factors that showed a statistically significant association with antenatal care utilization. Among the enabling factors, presence of husband approval, distance, waiting time to access ANC services and house holds monthly income were showed association with antenatal care utilization. Besides, planned pregnancy and received TT vaccination during recent pregnancy were some of the need factors that showed a statistically significant association with antenatal care utilization at P<0.25. Women who are living in urban settings were three times more likely to seek ANC services than their counterparts, COR=2.96 and 95% CI=(1.351,6.505) and women who have planned their recent pregnancies were two times more likely to attend ANC services than those women who didn’t panned their actual fertility with COR=2.48 , CI (1.35, 4.56).
In multivariable model, age between 35-49 years AOR is 0.178 (0.05, 0.61), educational status of mother with primary school AOR is 4.14 (1.06, 16.15), lack of housebound support AOR is 0.18 (0.07, 0.44), received TT vaccination during recent pregnancy is 8.12 (2.43, 27.29), waiting time to access ANC less than 30 min AOR is 3.38 (1.08, 10.58) and 31-60 min were significant factor for antenatal care utilization (Table 2).
| Variables | ANC Utilization | Crude OR with 95% (CI) | Adjusted OR with 95% (CI) | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Age of mother | 15–24 | 96 | 4 | 1 | 1 |
| 25–34 | 202 | 6 | 1.403(0.384, 5.084) | 3.703(0.88,15.65) | |
| 35–49 | 65 | 40 | 0.068 (0.023,0.198 )* | 0.178(0.05 ,0.61)* | |
| Educational status of mother | Illiterate | 214 | 46 | 1 | 1 |
| Primary | 120 | 3 | 8.59 (2.62,28.24 )* | 4.14(1.06 ,16.15)* | |
| Secondaryandabove | 29 | 1 | 6.23 (0.83,46.93) | 1.39(0.16,12.13) | |
| Occupation | Housewives | 336 | 39 | 1 | 1 |
| Maid servants | 6 | 1 | 0.69(.0.82, 5.94) | 2.78(0.16 ,47.96) | |
| Merchants | 14 | 6 | 0.27 (0.48,0.75)* | 0.24 (0.03,1.93) | |
| Others | 7 | 4 | 0.20(0.57,0.725)* | 0.13 (0.01 ,1.16) | |
| Residential | Urban | 131 | 8 | 2.96(1.357,6.505)* | 1.50(0.48,4.72) |
| Rural | 232 | 42 | 1 | 1 | |
| Parity | 1-2 | 117 | 9 | 1 | 1 |
| 3-4 | 159 | 17 | 0.72(0.32,1.67) | 3.03(0.70,13.16) | |
| 5 & above | 87 | 24 | 0.28(0.12 ,0.63) * | 3.77(0.82, 17.37) | |
| Knowledge ondanger signs of pregnancy | Yes | 75 | 20 | 3.84 (2.09,7.07)* | 1.84(0.71, 4.78 ) |
| No | 288 | 30 | 1 | 1 | |
| Presence of Husband approval | Positive | 305 | 23 | 1 | 1 |
| Negative | 58 | 27 | 0.201 (0.11, 0.51)* | 0.18(0.07,0.44)* | |
| Distance b/n from home to health Facility | Very close | 111 | 5 | 5.96( 2.23, 15.97 )* | 2.24(0.54, 9.39) |
| Average | 144 | 16 | 2.42(1.25, 4.67)* | 1.02 (0.37, 2.791) | |
| Too Far | 108 | 29 | 1 | 1 | |
| Received TT vaccination during recent pregnancy | Yes | 353 | 32 | 19.85(8.46, 46.62) | 8.12(2.43, 27.29)* |
| No | 10 | 18 | 1 | 1 | |
| Planned your recent Pregnancy | Yes | 219 | 19 | 2.5 (1.35, 4.56) | 0.69 ( 0.25, 1.93) |
| No | 144 | 31 | |||
| Waiting time to access ANC | <30 min. | 103 | 5 | 6.25(2.39, 16.3)* | 3.38(1.08, 10.58)* |
| >31 min. | 125 | 4 | 1 | 1 | |
Table 2: The result of logistic regression: the effect of demographic and socio-cultural factors on the antenatal care utilization of 15-49 age group of women in South Ari Woreda Southern, Ethiopia April/2015.
In this study, the overall coverage for antenatal care service utilization was 87.9% for women in their pregnancy time. This result was higher than studies conducted in Yem Special Wereda which is 28.5% and in Afar Assayeta which was 73% antenatal care utilization [7,8].
This increment might be due to the massive health promotion on antenatal care service utilization, increased awareness of respondents and accessibility. In this study, it was found that 58.9 % of women sought at least 2+ ANC from modern health care providers and close to 37 % had 4 and above visit which is below recommended, that WHO recommends a women without complications should have at least four focused visits to provide sufficient care. ANC is more effective in preventing adverse pregnancy outcomes when it is sought early in pregnancy and is continued throughout pregnancy [5,6].
Concerning the trimester at which the mothers started first ANC visit. Out of those who utilized ANC services 55.4% of them made their first visit in their second trimester of pregnancy and nearly 40% of them made their first visit in first trimester of pregnancy and 4.7% visited in third trimester. Nearly 37 % of mothers had four or more visits during their last pregnancy which is higher than study conducted in Yem special woreda i.e., 12.5% of them made their first visit in their second trimester of pregnancy.
The majority of study participants (93.2%) were received tetanus toxoid prevention vaccination during one year preceding the survey and only 47.8% were received TT2: this is lower than the recommended national coverage and study conducted in Afar Assayeta, which shows 73% of mothers were received TT2+ during their recent pregnancy.
The difference with that of ANC service coverage may be attributed to miss opportunity at the health facility. Among respondents 232 (63.9 %) mothers were received antenatal care from the health post, while 125 (34.4%) and 6 (1.7%) from health center and private clinics respectively.
Regarding place of delivery, 297 (71.9%) mothers delivered at health center, 74 (17.9 %) at hospital and the rest of 28 (6.8 %) and 14 (3.4%) gave birth at health post and home respectively. This finding is consistent with the studies in other regions in Ethiopia and Africa [9-11].
Multivariate analysis result showed that age, education, presence of husband approval and waiting time to access ANC were significantly associated with ANC utilization. For instance, when considering age, it was found that women in the age group 35-49 years were less likely to use ANC service than women in the age group of 15-24 years. Several studies found out that women age plays a significant role in the utilization of maternal health care [12-15].
This might be because younger women are more cautious about their pregnancies and sought trained professionals, but older women tend to believe that modern health care is not necessary due to experiences and accumulated knowledge from previous pregnancies and births.
Enabling factors, presence of husband’s approval and waiting time to access ANC services were found to be independent predictors of antenatal care service utilization. Husband or partner’s approval of ANC was most significantly related to antenatal care attendance. This result was similar to study conducted in similar setting in developing countries. It is expected that having a husband who approves antenatal care significantly increase the likelihood that a woman used anti natal care, irrespective of the husband’s background characteristics. Therefore, efforts to improve husband or partner’s attitude would probably increase utilization of health services by women [16-22].
Women who live within an hour walking distance from the health facility were more likely to visit antenatal care than above an hour distance by walking and a woman who reported waiting time less than 60 min to get/access/ANC services in the clinics were more likely to utilize ANC than those reported greater than 60 min. It agrees with previous studies conducted in Jigjig, Afar Assayeta, Malawi, and other studies conducted in Africa.
Majority of mothers were asked about the reasons that initiate them to start first ANC visit; majority 196 (54%) women replied-due to health problems to seek treatment and 167 (46 %) to start regular check-up. The major reasons for not attending ANC for women who did not utilize antenatal care were: 8 (16%) - no illness experienced during pregnancy; 28 (56%) - being too busy; 10 (20%) - husband disapproval and 4 (8%) - said long waiting time to access ANC. It is consistent with other studies conducted in Ethiopia [7,9].
Concerning benefit of ANC service utilization majority of mothers response were 310 (75.1%) beneficial both for the mother and fetus, 85(20.6%) beneficial only for the mother, 18 (4.4%) beneficial only for fetus.
Antenatal care utilization among the study participants relatively good in coverage but the pattern and timing of follow up was found to be inappropriate in most cases. Almost more than half of the mothers 201 (60.5 %) started utilizing antenatal care services in their second trimester; 17(4.7%) mothers were started their first ANC visit at third trimester of pregnancy.
Considering the late initiation of antenatal care visit of respondents, the effectiveness of the visit in reducing maternal morbidity and mortality could be hindered. The reasons given by the individual women for not attending antenatal care were found to be absence of illness (being healthy), being too busy, long waiting time, husbands/ family disapproval and poor quality of services are the most alarming intervention. Moreover, the use of ANC also varied with women’s exposure to previous pregnancy related illness, unwanted pregnancy and their perceived susceptibility to pregnancy related illness in their future pregnancies. Hence, there is a need to increase the availability and accessibility of antenatal care services to the needy, particularly to those rural women. Awareness about ANC through BCC/IEC activities should be emphasized targeting women, men, and influential family and community members through culturally accepted communication media and easy languages.
Increasing awareness of mothers on the danger signs of pregnancy and the importance of antenatal care utilization in addressing the problem, emphasis on advantage of early attendance of antenatal care (together with her husband or partner involvements). Increase women’s autonomy within the family enhancing their ability to earn and control income and decided on their own health. Education was found to have an impact on the use of antenatal care service suggests that improving educational opportunity for women may have a large impact on improving utilization of antenatal care services. In addition, improving the working condition of women, especially for parity of four and above, is one of the solutions to increase antenatal care utilization and increase the quality of health services. Focusing in family planning including contraceptive and vaccines, it helps to promote good health of mother and child for their best health condition and also to the responsible agent needs to give due attentions.
The authors have no conflict of interests.
W.W initiated and conducted the research, analyzed and interpreted the data, and prepared the draft manuscript. MG and EA advised on data collection, data interpretation and helped to write the manuscript.
We would like to thank the data collectors, South Omo Zone health office, South Ari Woreda health office and the staff of health facility for their persistent effort exerted during the data collection.