
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2022)Volume 13, Issue 8
The methemoglobinemia is rare clinical condition to encounter during perioperative period. However, methemoglobinemia diagnosis should be considered with patients presenting complaints of cyanosis and hypoxia or low SpO2 (On pulse oximeter) which is unrelated to cardiopulmonary causes. Patient who was known case of Hansen’s disease on multi drug therapy planned for ulnar nerve decompression had low saturation even on providing oxygen therapy which on evaluation found to be drug induced methemoglobinemia. Plan and mode of anesthesia preference for consideration of any type of surgery with methemoglobinemia needs to be evaluated thoroughly as it being a rare disease.
Saturation of oxygen; Methemoglobin; Histidine; Tyrosine; Glucose-6-phophate dehydrogenase; Logarithm hydrogen ion concentration; Surgery; Analgesics; Bicarbonate; Anaesthetic drugs
The methemoglobinemia is a rare clinical condition to encounter during perioperative period. However methemoglobinemia diagnosis should be considered with patients presenting complaints of the cyanosis and hypoxia or low SpO2 (On pulse oximeter) which is unrelated to cardiopulmonary causes. Methemoglobin is formed by oxidation of the heme iron of hemoglobin to the ferric state. Methemoglobin has very high oxygen affinity and virtually no oxygen is delivered to the tissues. Methemoglobinemia may be congenital or acquired. Congenital methemoglobinemia arises from mutations that stabilize iron in the ferric state (e.g., HbM Iwata (α87 His→Tyr)) or from mutations that impair the enzymes that reduce methemoglobin to hemoglobin (e.g., methemoglobin reductase, NADP diaphorase), and manifest early in life [1].
Many pharmacological agents and toxins have propensity to cause methemoglobinemia for i.e., dapsone, nitrates, quinone, salfonamides, aniline, chlorates etc. The time of onset of symptoms and duration depend on the agent and its concentration. For many agents, the onset is within hours, but is delayed for others such as dapsone and nitroethane [2]. Cyanotic discoloration of skin due to dark-colored methemoglobin is typically observed at levels greater than 15% and is often one of the earliest clinical manifestations (Table 1).
| Classes | Drugs |
|---|---|
| Acetamides | Phenacetin |
| Analgesics | Phenazopyridine |
| Antibiotics | Dapsone, Trimethoprim, Sulfonamides |
| Antigout agents | Rasburicase |
| Antimalarials | Chloroquine, Primaquine |
| Antineoplastic agents | Cyclophosphamide, Flutamide |
| Industrial/household Products | Aniline dyes, Naphthalene, Aminophenols, chlorates, Bromates, Herbicides, and Pesticides |
| Local anesthetics | Articaine, Benzocaine, Lidocaine, Prilocaine |
| Nitrate derivatives | Nitrates salt, Nitroglycerin |
| Nitrite derivatives | Nitroprusside, Amyl nitrite, Nitric oxide |
Table 1: Showing causes of methemoglobinemia.
Dapsone is metabolized in the liver by N-acetylation and Nhydroxylation. Dapsone hydroxylamine is a strong oxidant and responsible for inducing methemoglobinemia. Dapsone induced methemoglobinemia is not related to G6PD activity and significant variation in magnitude of clinical manifestation is observed [3,4]. Signs and symptoms may varies depends on level of methemoglobin level in blood but severity range from asymptomatic to serious cardio-pulmonary arrest even death, which may require emergency medical attentions (Table 2). A written consent has been obtained from the patient for publication.
| Methemoglobin Concentration | Signs and Symptoms |
|---|---|
| 0%-3% | No symptoms |
| 10%-20% | Mild symptoms cyanosis, Chocolate brown blood (as presented in case report) |
| 20%-50% | Dyspnea, Decreased exercise tolerance, Fatigue, tachycardia |
| >50% | CNS hypoxia, Seizure, Metabolic acidosis, Tachypnea |
| >70% | Severe hypoxia, Coma, Death |
Table 2: Signs and symptoms of the methemoglobin concentration.
A 30-year-old male patient, diagnosed as a case of Hansen’s disease who presented with history of paraesthesia of right ulnar nerve distribution since last three months and red raised circular lesion since last few days. The patient had no known comorbidity. Patient was started on treatment Tab Dapsone 100 mg OD, Cap Rifampicin 600 mg OD, Cap Clofazamine 50 mg OD and Tab Prednisolone 60 mg OD since last one month.
On evaluation, found thickened ulnar nerve right side with features of micro abscess. The patient was therefore initially planned for urgent right ulnar nerve decompression under regional anaesthesia.
The patient on arrival was evaluated at pre-operative room was found to have low SpO2 on pulse oximeter 86% and it was not improving even on providing oxygen with face mask at 10-15 litres per minute. However on detailed evaluation and examination patient did not have any chest and respiratory discomfort. Other vitals parameter and systemic examination were under normal limits. Hence Arterial Blood Gas evaluation was planned after taking informed consent of patient. Arterial Blood Gas sampling revealed dark brown colour on inspection as shown in Figure 1 and values recorded were pH 7.44, PaCO2 27.7, PaO2 72.3, HCO3 19.1, Lac 0.8 on room air. Hence correlation between Spo2 and PaO2 was not justified. In view of this surgery was deferred for further evaluation and management for low SpO2.
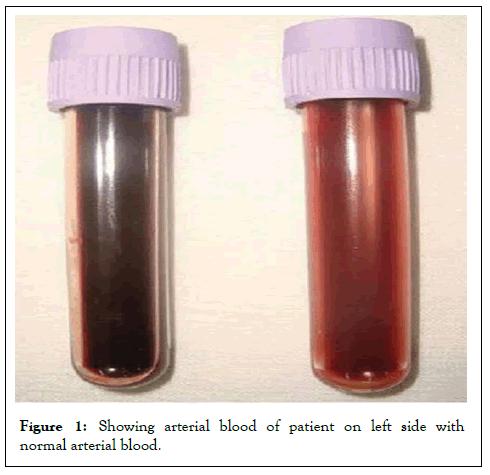
Figure 1: Showing arterial blood of patient on left side with normal arterial blood.
The cause for low SpO2 was evaluated. Patient had blue coloured sclera. All systemic examination was found to be within normal limits. The dissociation between low SpO2 and near normal PaO2 raised suspicion of Methemoglobinemia. On further evaluation by Co-oximetry it was found that there is raised methemoglobinemia of value 22% and G6PD deficiency evaluation was negative. Immediately the cause for Methemoglobinemia in a young was searched. The evaluation showed Tab Dapsone as one of them which produces methemoglobinemia and hence was stopped in consultation with Dermatologist. SpO2 level improved to 97% on room air while on Oxygen with Facemask is 100% after 5 days. Other cardiac and pulmonary evaluation was found within normal limits. Hence a final diagnosis was made as Dapsone induced methemoglobinemia. After optimization of the patient he was planned for elective ulnar nerve decompression under regional anaesthesia.
Methemoglobinemia is a rare condition and may occur on exposure to oxidising agents such as aniline dyes, nitrobenzene, nitrate, nitrite, lidocaine, prilocaine, dapsone, pyridium, nitric oxide, nitrous oxide and naphthalene due to overwhelming capacity of reducing enzymes [1]. Children are more susceptible due to the presence of foetal haemoglobin, which oxidises more easily, low levels of NADH reductase, higher gastric pH, which promotes growth of nitrate reducing organisms causing conversion of dietary nitrates to nitrite [1,3,4].
Clinically, methemoglobinemia is differentiated from cardiopulmonary diseases by lack of significant pulmonary and cardiac finding on history, examination and investigations and cyanosis, which fails to respond to supplemental oxygen. Arterial Blood Gas reveals the classical ‘saturation gap’, with normal PaO2 despite cyanosis [1]. The symptoms appear depending on methemoglobin level in blood. Chocolate colour cyanosis presents at levels of 5-15% and appears early in anaemic patients. Even at least 5 mg of reduced haemoglobin must be present for cyanosis to be detected. At 30-40%, weakness, headache, dyspnoea, tachycardia and dizziness occur. Patient will be lethargic, stuporous, confused and comatose at concentration of 55-60% and at about concentration of 70% circulatory collapse occurs [1,2].
Intraoperative monitoring must include co-oximetry, which detects the presence as well as quantifies methemoglobin level [5]. Injection methylene blue is the antidote and it should made available at operation theatre [1,3]. Also uses of vitamin C in perioperative period should be considered which may help by increasing the level of NADH methemoglobin reductase, which helps in conversion of ferric ion to ferrous ion. Exchange transfusion and haemodialysis is indicated in severe cases. In acquired methemoglobinemia the chemical agent of cause which is causing it should be withdrawn at earliest. Anaesthetic drugs, which induce methemoglobinemia, are local anaesthetics example (lidocaine, benzocaine etc), metoclopramide, nitrous oxide, and nitroglycerine and sodium nitroprusside. They should be avoided or may be used on titrated doses [5-7]. Thorough planning and preference for mode of anesthesia for consideration of any type of surgery with methemoglobinemia needs to be evaluated thoroughly as it being a rare disease [8,9].
Methemoglobinemia is a rare clinical condition to be encountered during perioperative period. However, methemoglobinemia diagnosis should be considered in any patient presenting with complaints of cyanosis and hypoxia or low SpO2 (On pulse oximeter) who is unrelated to cardiopulmonary causes or without any complaints. The dissociation between low SpO2 and near normal PaO2 should be evaluated by arterial blood gas analysis and should raise the suspicion of Methemoglobinemia. Intraoperative monitoring must include co-oximetry, which detects the presence as well as quantifies methemoglobin level. Thorough planning and preference for mode of anesthesia for consideration of any type of surgery with methemoglobinemia needs to be evaluated thoroughly as it being a rare disease.
None
None
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Naik S, Jaiswal A, Agarwal M, Goel A (2022) Anesthetic Concerns of Patient Planned for Urgent Surgery with Incidental Diagnosis of Methemoglobinemia in Hansen’s Disease: A Case Report. J Anesth Clin Res. 13:1078.
Received: 25-Jul-2022, Manuscript No. JACR-22-19035; Editor assigned: 28-Jul-2022, Pre QC No. JACR-22-19035 (PQ); Reviewed: 12-Aug-2022, QC No. JACR-22-19035; Revised: 19-Aug-2022, Manuscript No. JACR-22-19035 (R); Accepted: 25-Aug-2022 Published: 25-Aug-2022 , DOI: 10.35248/2155-6148.22.13.1078
Copyright: © 2022 Naik S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.