
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2022)Volume 13, Issue 5
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome virus coronavirus 2 (SARS-CoV-2) which mainly affects lungs with common symptoms of fever, cough and shortness of breath. COVID-19 is an ongoing global pandemic causing a serious health problem. Computerized Tomography (CT) has an important role in initial evaluation and follows up of the disease. Main CT finding of the disease is bilateral extensive ground-glass opacification with a peripheral or posterior distribution, mainly involving the lower lobes. In this report, we present a case of pneumothorax in a patient with COVID-19 undergoing bone oncologic surgery and the subsequent management and follow-up.
COVID-19; Osteosarcoma; Surgery; Opacification
COVID-19 was first seen in December 2019 in Wuhan, and has since spread globally, resulting in a global pandemic [1]. At hospital admission, most common symptoms of COVID-19 are fever, cough and shortness of breath. Abdominal pain, myalgia, diarrhoea, sore throat, fatigue and loss of smell are other possible symptoms [2]. The diagnosis is made by real time– reverse transcription polymerase chain reaction (rRT-PCR) from a nasopharyngeal swab.
Imaging with Computerized Tomography (CT) is strongly recommended especially in COVID-19 suspected cases on either initial evaluation or follow-up. Known radiologic hallmarks of COVID-19 pneumonia on CT are bilateral extensive groundglass opacification with a peripheral or posterior distribution, mainly involving the lower lobes. Uncommon features also seen are pleural and pericardial effusion, lymphadenopathy, cavitation, CT halo sign, and pneumothorax [3]. In descriptive study of Chen et al. which reported the characteristics of 99 patients with COVID-19, they reported that a patient presented with pneumothorax on CT in first admission (Figure 1) [4].
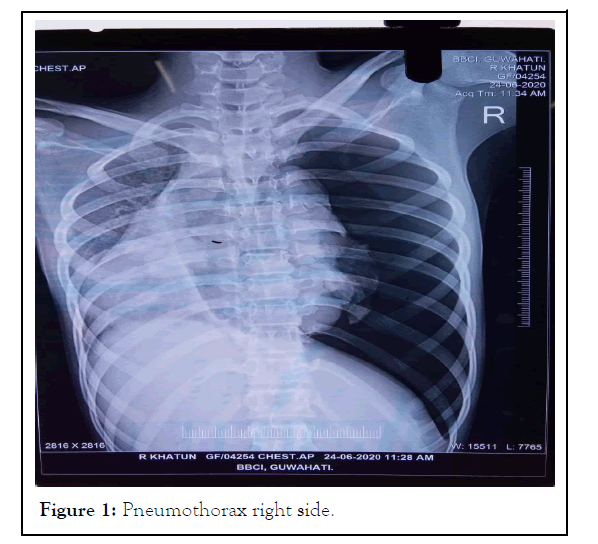
Figure 1: Pneumothorax right side.
In this report, we describe a case of a female patient diagnosed with COVID-19 pneumonia with pneumothorax as an initial presentation presenting for a bone oncologic surgery and the anaesthetic and surgical management that followed initial diagnosis.
A 17-year old female presented to the out-patient department of our tertiary cancer care hospital with pain in the left thigh and restricted movement of the thigh and knee. She had a history of fall and swelling around the knee joint three months back. X-ray of the knee joint showed an old fracture in distal end of femur along with soft tissue swelling. At that time her chest X-ray was normal. She had no other associated symptoms like fever, and no significant past or present medical or surgical history. After workup she was provisionally diagnosed as non-metastatic osteosarcoma with pathological fracture and admitted to the ward one week later (Figure 2). Core biopsy of the swelling showed stage IV osteosarcoma. Her laboratory picture showed anaemia with haemoglobin of 5.4 g/dL for which she received three units Packed Red Blood Cells (PRBC) after which her Hb (haemoglobin) increased to 10 g/dL.
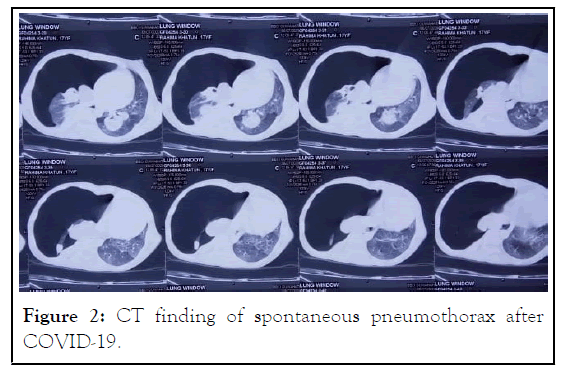
Figure 2: CT finding of spontaneous pneumothorax after COVID-19.
Two weeks later she had one episode of breathing difficulty. It was treated conservatively with oxygen supplementation and nebulization. Radiological findings showed massive pneumothorax on the right side with shifting of the mediastinum to the opposite side. The cause of the pneumothorax was ascertained to be spontaneous rupture of bullae. There was some resolution of symptoms after chest drain insertion. Other findings in CXR were pneumonic patches/ metastases (Figure 3).
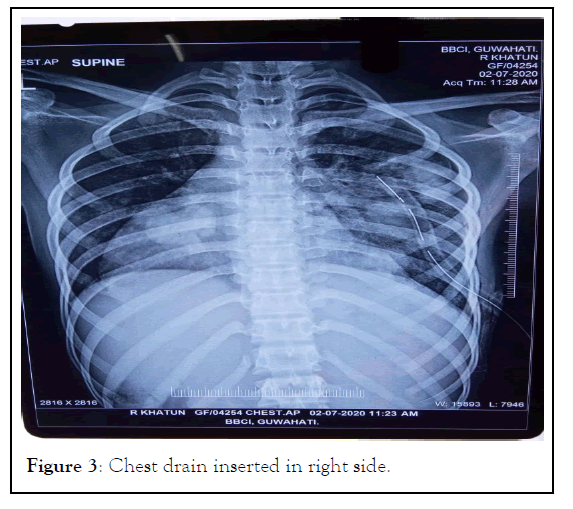
Figure 3: Chest drain inserted in right side.
She was posted for left below knee amputation for which Pre- Anaesthetic Checkup (PAC) was done. Her blood works and other investigations were not highly significant. One week later before her scheduled surgery, she tested positive for SARSCov- 2. Associated symptoms were productive cough and one or two episodes of fever. She was shifted to the covid isolation ward of the hospital and started on treatment for SARS-Cov-2 with hydroxychloroquine, ivermectin, remdesivir, oxygen therapy and nutrition supplements (Figure 4).
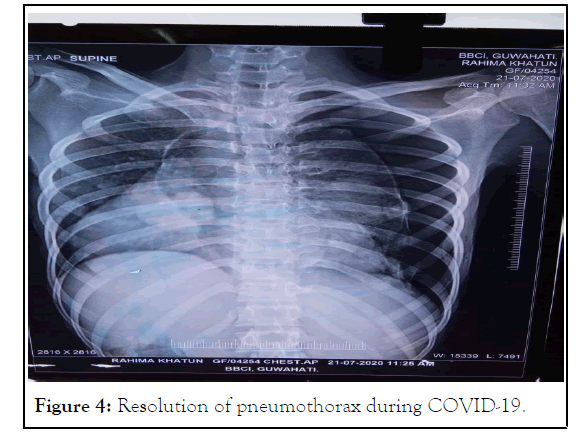
Figure 4: Resolution of pneumothorax during COVID-19.
On day 14 of her positive swab test, her test turned negative. She was again examined in the PAC clinic for left hip disarticulation. Five days later amid preparations for an elective surgery, there was development of spontaneous bleeding during dressing of the swelling. Her Hb dropped to 6.7 and TLC rose to 19320. Anemia was corrected and Inter Costal Drain (ICD) was removed as there was no more breathlessness or chest pain. She was put up for emergency palliative hip disarticulation. It was considered a surgical emergency because of the fun gating growth and there was also the open pathological fracture which was bleeding (Figure 5).
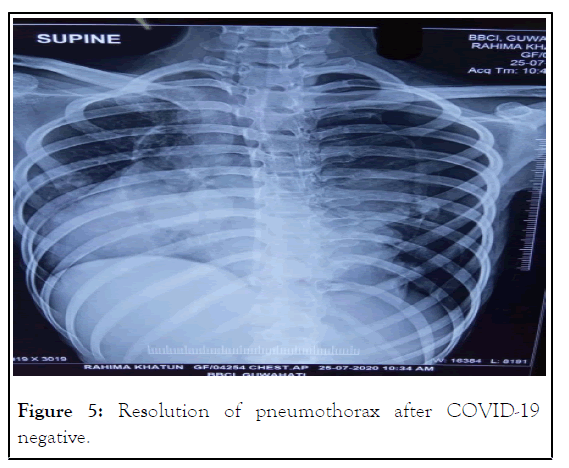
Figure 5: Resolution of pneumothorax after COVID-19 negative.
Anesthetic management
Regional anaesthesia was decided upon as the choice of anaesthesia because of the following factors: her breathingdifficulty episodes led us to believe that she had a bad lung which was compounded by the fact that she had recently recovered from COVID-19 infection. There was apprehension of possible prolonged mechanical ventilation with difficult to wean scenario in the ICU Intensive Care Unit (ICU). There was also the advantage of limiting aerosol transmission following intubation in general anaesthesia. However, regional anaesthesia was not without its own disadvantages as the patient had an active bleeding tumour which could lead to detrimental fall in central circulation. There was the added disadvantage of a difficult positioning for regional anaesthesia as due to her fracture there was an elizarov pin attached to her hip joint, making her unable to sit or turn sideways (Figure 6).
Figure 6: Stages involved in anesthetic management of a Post-Covid Osteosarcoma Patient.
Finally the decision was made to give her a low-dose graded epidural. With the help of two assistants the patient was put in a semi-prone position and epidural was given using 18 gauges Tuohy needle in a single shot at the level of L2-L3 to achieve a level of block till T10. The epidural catheter was inserted after checking for negative aspiration of blood or Cerebro Spinal Fluid (CSF) and fixed at 10 cm from the skin. Local anaesthetic Inj levobupivacaine 0.5% was given in a graded manner. 5 ml was first injected and the effect of block was observed after ten minutes. After observing for unchanged hemodynamics another 5 ml was injected and similarly observed. In total she received 15 ml of local anaesthetic which seemed to be adequate for her physical frame and height. Intra-operatively she received 2 L of crystalloid and two units of packed cells. Intraoperative period was uneventful. For post op management of pain, epidural infusion was given with inj levobupivacaine 0.25% of 2 ml/h which was continued for the next 24 hours of post op period with proper monitoring. She was weaned off from ICU and shifted to the ward on day four of surgery.
Pneumothorax in covid
Pneumothorax is a clinical entity which is defined as presence of air between visceral and parietal pleura, which can impair oxygenation and ventilation. Pneumothorax can be classified into three categories as spontaneous (primary or secondary), traumatic and iatrogenic, with spontaneous pneumothorax being the most common type. The term spontaneous pneumothorax refers to the presence of air in the pleural spacethat is not caused by trauma or other obvious precipitating factor (trauma or iatrogenic during a procedure).Secondary spontaneous pneumothorax occurs due to preexisting lung disease, like pneumonia or in recent times COVID-19 viral pneumonia [5,6]. The proposed mechanism of spontaneous pneumothorax in patients with COVID-19 disease is thought to be related to the structural changes that occur in the lung parenchyma. These include cystic and fibrotic changes leading to alveolar tears [7]. Patients with COVID-19 infection can develop severe pneumonia leading to acute respiratory distress syndrome (ARDS) characterized radio graphically by ground glass opacities, evolving into consolidative and fibrotic changes. These changes, in addition to possible over distention of the alveoli by mechanical ventilation may put patients at risk for developing pneumothorax.
Even though mechanical ventilation appears to be a predominant risk factor for development of pneumothorax with COVID-19 pneumonia, Wang et al. reported a case of a patient who developed spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema who was not on any mechanical ventilation.6 Similarly, Zhou et al. reported a case of spontaneous pneumomediastinum in a patient with COVID-19 who was spontaneously breathing [7]. Persistent cough can cause increase in intrathoracic pressure and severe strain leading to pneumothorax in COVID-19 pneumonia. Cough may enhance leakage of air out of the alveoli by causing sudden lengthening and shortening of the pulmonic vessels and associated bronchi during respiration and further moving the “train of bubbles” along the vascular sheaths. Baseline imaging may be predictive for patients who may develop pneumothorax. One case report described a patient with no baseline lung disease who developed a giant bulla as a result of COVID-19 infection that ended up rupturing and causing pneumothorax [8]. In our case also, the most likely cause of pneumothorax was rupture of bullae. Anaesthetic issues in covid positive patients.
COVID-19 usually presents with fever and dry cough. Sometimes non-significant symptoms such as fatigue, diarrhoea, and mild myalgia are also recorded. In addition, 50% of asymptomatic cases can still be infectious which can complicate the perioperative period [9]. Our patient also showed symptoms of fever, cough and respiratory distress. 10% of covid patients in the ICU need mechanical ventilation owing to respiratory distress, sepsis, and multiple organ dysfunctions. Severe hypoxaemia is observed usually following the 7th day of the start of the symptoms [10]. During the preoperative evaluation, protective measures should be taken carefully with Personal Protection Equipment (PPE) used as needed.
There is a decrease in WBC (White Blood Cell) with increased neutrophils, mild increases in Aspartate Amino Transferase (AST), Alanine Amino Transferase (ALT), bilirubin, cardiac troponin levels and decrease in albumin, high factor VIII levels with prolonged Activated Partial Thromboplastin Time (aPTT) but normal Prothrombin Time (PT). Increased D-dimer levels, prothrombin time, and thrombocytopenia are predictive of adverse outcome and disseminated intravascular coagulation that can escalate the blood loss during surgery [11]. Elevatedcreatinine and Blood Urea Nitrogen (BUN) levels may lead toincreased morbidity and mortality which warrants the avoidance of nephrotoxic drugs during anesthesia [12].
Drugs used for the treatment of COVID-19 may cause deranged liver function tests [13]. These antiviral drugs may interact with anaesthetic agents like propofol, sevoflurane and tramadol and may lead to various adverse effects including cardiac arrhythmias. Atazanavir and lopinavir/ritonavir can potentiate the effects of bupivacaine, ketamine, rocuronium, fentanyl and tramadol. Tocilizumab can decrease the effects of bupivacaine, ketamine and fentanyl. Favipiravir can increase the effect of paracetamol. All these must be kept in mind while choosing the anaesthetic agents.
All patients admitted to the operation room should be considered infected with COVID-19. As thrombocytopenia is very common in severe patients, platelet levels should be checked before the operation and if needed, blood products including platelets must be kept prepared. Even in patients with no cardiac history, COVID-19 can present itself with cardiac arrhythmias. Hence, proper monitoring with standard American Society of Anaesthesiologists (ASA) monitoring guidelines must be done.
Although for many emergency or oncological surgeries, general anaesthesia is recommended, regional anaesthesia should be preferred over general anaesthesia wherever possible in order to minimise aerosol-generating procedures such as intubation and extubation [14]. Regional anaesthesia also reduces postoperative pulmonary complications, which can complicate the respiratory failure in a COVID-19 infection further. The contraindications such as bleeding disorders must be taken into account as it is a common finding mainly in severe COVID-19 patients. Platelet count should be monitored before Neuraxial block administration [15].
Standard monitoring should be used for all patients. Deep sedation should be avoided in order to reduce the need for airway manipulations. During regional anaesthesia, patients should wear surgical mask at all times. The anaesthesiologist should wear N95 respirators during the regional anaesthesia intervention. We decided upon regional anaesthesia for our patient for the same reasons as stated above. If general anaesthesia is indicated, Rapid Sequence Intubation (RSI) is recommended in order to minimize the spread of aerosols. There is no direct data concerning fluid therapy for COVID-19 patients. Restricted fluid strategy is recommended based on studies concerning sepsis and ARDS by Surviving Sepsis Campaign Guideline. Balanced crystalloids should be chosen over colloids. Norepinephrine and vasopressin can be used as vasoactive agents in shock [16].
Hypothermia must be avoided as it along with acidosis and coagulopathy in COVID-19 patients, may worsen the patient’s condition. Warming intravenous and irrigation fluids must be preferred to forced air-warming systems to achieve normothermia.
It is difficult to ascertain the exact cause of respiratory distress in a situation compounded by associated diagnosis such as SARS-Cov2. Spontaneous pneumothorax is a rare complication of COVID-19 viral pneumonia. It may occur at any time during the course of the disease. Patients with baseline ground-glass opacities and consolidations and those who are mechanically ventilated appear to be at high risk. Clinicians should be vigilant about the diagnosis and treatment of this complication.
Anaesthetists are among those health care workers at high risk of infection with COVID-19 both in the operation theatre and the ICU. With proper judgments, precaution and decision making, the risks of COVID-19 pneumonia and associated complications can be reduced or avoided in both patients and heath care workers. In the coming years, the risk of developing infection with coronavirus will still remain high so it is imperative to be clinically sound and develop more research methods for the proper management of the disease.
[Cross Reference] [Google Scholar] [Pubmed].
Citation: Ninu M, Chintey D, Kakati SD, Kakati B, Das A (2022) Anaesthetic Management of a Post-Covid Osteosarcoma Patient with Spontaneous Pneumothorax and an Active Bleeding Tumour. J Anesth Clin Res. 13: 1061
Received: 04-May-2022, Manuscript No. JACR-22-17599; Editor assigned: 06-May-2022, Pre QC No. JACR-22-17599(PQ); Reviewed: 23-Jun-2022, QC No. JACR-22-17599; Revised: 30-May-2022, Manuscript No. JACR-22-17599(R); Published: 06-Jun-2022 , DOI: 10.35248/2155-6148.22.13.1061
Copyright: © 2022 Ninu M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.