
Cell & Developmental Biology
Open Access
ISSN: 2168-9296

ISSN: 2168-9296
Case Report - (2020)Volume 9, Issue 3
Knowledge of neurovascular variants in the upper limb is important to neurologists in explaining unusual neurological presentations, to trauma surgeons in the selection of appropriate surgical interventions, and to neuroradiologists in the interpretation of images. Here we present the case of an absent subscapular artery coexisting with multiple variants of the brachial plexus nerves in the left limb of a 71-year-old female cadaver. The median nerve was formed from 3 roots, 2 contributed by the lateral cord and one from the medial cord. The thoracodorsal branch shared a common trunk of origin with the lateral thoracic artery, while the circumflex scapular arose directly from the axillary artery. The musculocutaneous nerve did not penetrate the coracobrachialis muscle, but coursed superior to the second lateral root, and about the proximal and middle third of the brachium supplied the flexor arm muscle, continuing distally as the lateral cutaneous nerve of the forearm. The first lateral root coursed initially within the medial root proximally, exiting about 3 cm distally before travelling superolaterally to join the second lateral root. Final formation of the median nerve was in the distal third brachium. There is uniqueness in this median nerve formation; a variant or a reverse of Le Minor Type 2 was observed except that this lateral root joined the medial root initially, unlike in Type 2 in which the medial root joins the musculocutaneous nerve, both re-exiting to join in median nerve formation. Clinically, unexplained sensorimotor deficits in the flexor compartments distal to the elbow may be explained by inadvertent ligation to any of these median nerve roots.
Le Minor Type 2; Absent subscapular artery; 3 roots formation of the median nerve; Unexplained sensorimotor deficits
The axillary artery (AA) begins at the outer border of the first rib and ends at the inferior border of the teres major muscle, divided into three parts by the pectoralis muscle and carrying six independently arising vessels. Three of these vessels arise from the third part of the artery which stretches between the lateral border of the pectoralis minor, ending in the inferior border of teres major to continue as the brachial artery. The vessels in the third part consist of the subscapular artery (SSA) and the anterior and posterior circumflex humeral arteries. The SSA is the largest of the six branches of the AA, and variations in the AA are centered around the SSA. These numerous variations include the SSA of “high origin,” which occurs when the artery arises much nearer or on a level with the thoracoacromial artery (TAA) or from its retropectoral part. Keen reported a range of incidence from 26.3 % to 31.7% of the SSA arising from the second part of the artery [1]. When the SSA was absent (1.7%), the circumflex scapular artery arose directly from the third part of the axillary artery and the thoracodorsal artery was a branch of the lateral thoracic artery or it had a separate and direct origin from the axillary artery. Huelke reported a 1.7% incidence of the absence of the SSA [2].
Among the ventral primary rami contributing to the brachial plexus, the upper two rami (C5 and C6) join, as do the lower two rami (C8 and T1). The middle ramus (C7) continues on its own. The five ventral primary rami are thereby reduced to three nerve trunks. Each trunk then separates into an anterior and a posterior division. All three posterior divisions unite into a single posterior cord. The fundamental simplicity of the brachial plexus would be more obvious if the three anterior divisions were also to unite into a single common flexor cord. Instead, there are two, the lateral and medial cords of the brachial plexus innervating the anterior or flexor musculature [3].
The musculocutaneous nerve (MCN) and the median nerve (MN) are two of the principal peripheral nerves of the brachial plexus, which include the axillary and radial nerves from the posterior cord, and the ulnar (C8, T1) from the medial cord. The MCN is given off by the lateral cord, while the MN is formed from two roots, one contributed from the lateral cord and the other from the medial cord. Extensive communications have been reported between many of these peripheral nerves, most especially between the MCN and the MN. Veniaratos and Anagnostopoulu reported 22 communications occurring between the MCN and the MN in 16 out of 79 cadavers [4].
Le Minor (1992) classified these variations of the MCN and its communication with the MN into 5 types:
Type 1: No communication between MN and MCN.
Type 2: The fibers of the medial root of the MN pass through the MCN and join the MN in the middle of the arm.
Type 3: The fibers of the lateral root of the MN pass through the MCN and after some distance leave it to form the lateral root of the MN.
Type 4: The MCN fibers join the lateral root of the MN and after some distance the MCN arise from the MN.
Type 5: The MCN is absent and all the MCN fibers pass through lateral root of MN; fibers to the muscles supplied by MCN branch out directly from MN. In this type, the MCN does not pierce the coracobrachialis muscle [5].
An incidental finding of a bilateral communication between the MCN and MN was reported by Mao-Q-H in the limbs of a 79- year-old Chinese cadaver; this communication occurring distal to MCN had pierced the coracobrachialis muscle [6].
During routine dissection, we noted an absent SSA coexisting with multiple variants of the brachial plexus nerves in the left limb of a 71-year-old female cadaver. The MN was formed from 2 roots contributed by the lateral cord and 1 from the medial cord (Figure 1). The thoracodorsal branch shared a common trunk of origin with the lateral thoracic artery, while the circumflex scapular arose directly from the AA (Figure 1). The MCN did not penetrate the coracobrachialis muscle, but coursed within the thirdsuperiorly to the second lateral root and , exiting about the junction of the proximal and middle thirds of the brachium issued branches to supply the flexor arm muscles, continuing distally as the lateral cutaneous nerve of the forearm (Figure 1). The first lateral root (LR1) coursed within the medial root proximally, exiting about 3 cm distally (LR1*) before travelling superolaterally to join the second lateral root. Final formation of the median nerve was in the distal third brachium.
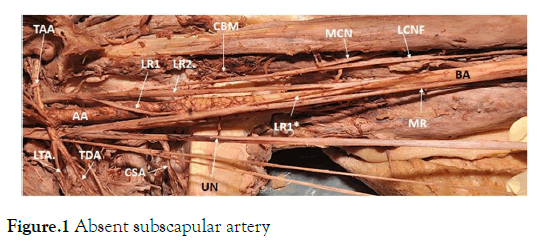
Figure 1. Absent subscapular artery
This image shows the left limb with an absent subscapular artery, the thoracodorsal artery (TDA) haring a common trunk with the lateral thoracic artery (LTA). The musculocutaneous nerve (MCN) did not penetrate the coracobrachialis muscle (CBM . The nerve gave supplies to the flexor muscles and continued as the lateral cutaneous nerve of the forearm (LCNF).
The lateral cord (LC) gave rise to 2 roots contribution to the formation of the median nerve (MN). The1st lateral root exited from the lateral cord , coursed medially to run with the medial root (MR) , running with the medial root for about 2-3 cm and then exited and coursed supero-laterally (LR1*) to join the 2nd lateral root(LR2) proximal to the latter joining the medial root (MR) to form the median nerve at about the distal 1/3rd of the arm.
AA; axillary artery, BA; brachial artery. LR1*; 1st lateral root reexiting to join 2nd lateral root.
There is uniqueness in the formation of the MN in this cadaver, a reverse of Le Minor Type 2 except that here the lateral root joined the medial root initially, unlike in Type 2 Le Minor in which the medial root joins the MCN, both re-exiting to join in MN formation.
Variant anatomy of the AA occurs when there is a failure of normal development of the artery, resulting in a number of heterogeneous anomalies of the artery and its branches. The sprouting theory on embryological development by earlier researchers [7] has been described obsolete. The findings suggest that these arterial patterns develop from an initial capillary plexus by a proximal to distal differentiation, due to maintenance, causing enlargement and differentiation of certain capillaries and the regression of others [8].
Such heterogeneity may result in an increase or decrease in the total number of branches emanating from the AA. Quain reported a variant that increases the number of vessels arising from the AA, an instance in which the suprascapular and dorsal scapulae arteries originate directly from the AA and not from the subclavian artery [9]. A reduction of the number of vessels will occur when two of the usual branches of the AA share a common trunk of origin. The absence of any of the six branches of the AA will also lead to a decrease in the number of vessels arising from the AA. Huelke reported an 11.2% incidence of a common trunk for the circumflex humeral arteries.
There have been many reports of communication between the MCN and the MN, and several criteria have been employed to classify communication by the different authors. In classifying these communications, Le Minor used the idea of either presence or absence of the MCN, without any reference to the sites of communication, whereas Venieratos and Anagnostopoulus adopted a classification using the sites of communication.
Type I: Communications were proximal to the entry of the MCN into the coracobrachialis.
Type II: Communication was distal to the muscle.
On the other hand, Choi et al. based their classification in terms of either fusion or the occurrence of a supplementary branch between the 2 nerves. In a study of 138 cadavers, Choi et al. reported finding variations in 64 cadavers (46, 4%), of which 9 were bilateral and 15 unilateral. Variations were observed in 73 out of 276 arms (26.4%), with no statistical difference gender or lateral wise. Choi et al. classified three variational patterns between MN and MCN:
Pattern 1: Fusion of both nerves with a reported incidence of 13.1%.
Pattern 2: Presence of one supplementary branch between both nerves with a reported 75.4 % incidence.
Pattern 3: Two branches [10].
The coexistence of an absent SSA with the MN being formed from four roots is very rare and has not been reported. Absence of SSA alone is just 1.7%. In addition, the occurrence of the Le Minor Type 2 variant has not been reported. Knowledge of neurovascular variants in the upper limb is important to neurologists in explaining unusual neurological presentations, to trauma surgeons in the selection of appropriate surgical interventions, and to neuroradiologists in the interpretation of images.
The authors declare no competing interest.
Dedicated to my Late Professor and Mentor, Professor Adesegun Banjo.BSC (Anat) Makerere Univ., MBBS (Oxford) Ph.D. (PENN. MD (Oxford).
A great teacher, Mentor and Friend. Thank you for all you taught and lessons of life learnt from you.
Immense thanks to Pamela Walter, MFA Office for Professional Writing, Publishing, & Communication, Thomas Jefferson University for helpful resource guidance and professional help in proof reading and Manuscript editing.
And to the Human Gift, for contribution to knowledge even in death.
Citation: Olutayo A (2020) An Absent Subscapular Artery Co-Existing with Multiple Variants of the Brachial Plexus and Clinical Implications. Cell Dev Biol 2020; 9:206. doi: 10.24105/2168-9296.2020.9.206
Received: 07-Jul-2020 Accepted: 01-Aug-2020 Published: 05-Aug-2020 , DOI: 10.35248/2168-9296.2020.9.206
Copyright: © 2020 Olutayo A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.