Hair Therapy & Transplantation
Open Access
ISSN: 2167-0951
ISSN: 2167-0951
Review - (2020)Volume 10, Issue 2
Alopecia areata (AA) is suddenly occurring, non-scarring hair loss disease. There are many theories, and many implied factors, but the true pathogenesis of AA is still not clear. In this review we discuss therapy of AA, topical, systemic and biologics.
Few cases are presented with dermoscopic (trichoscopic) view of the scalp, and use of trichoscopy in prognosis of AA. This is a completely benign condition, but devastating for a patient and requires multidiscipline.
Alopecia areata; Dermoscopic; Trichoscopic; Anagen
Alopecia areata (AA) is suddenly occurring, non-scarring hair loss disease [1]. AA occurs in populations world – wide it estimates about 0.7 to 3.8 percent of outcome patients in dermatology clinics [2]. AA nearly affects males and females equally, although some studies show a significant males predominance in adult onset of AA [3].
The disease begin at any time of life, may begin as early as the first month of life [4], but the peak incidence between 20 and 50 years of age5. No reported cases of Congenital AA, but congenital triangular Alopecia can greatly mimic Alopecia Areata [5,6] (Figure 1).
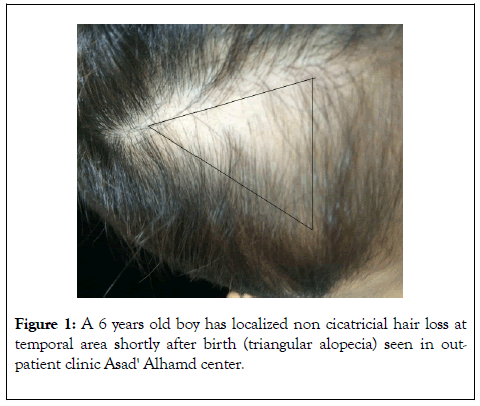
Figure 1: A 6 years old boy has localized non cicatricial hair loss at temporal area shortly after birth (triangular alopecia) seen in outpatient clinic Asad' Alhamd center.
Etiopathogenesis of alopecia areata
There are many postulated causes ofAA.AA is anautoimmune disease in genetically predisposed individuals which may triggered by psychological factors, but the accurate causes are still unrecognized.
Haircycle and AA
AA preferentially affects pigmented hair follicles in the anagen (growth) phase of the hair cycle, and when the hair regrows within the AA patches, it frequently grows back white or colorless. This phenomenon of “sudden whitening of the hair” is therefore ascribed to AA with an acute onset, and has been documented throughout history of some affected individual shaving that onset at times of profound sadness, stress, or fear [7].
Genetic factors
The genetic predisposition for alopecia areata is thought to be polygenic in nature, polygenic, means, multiple gene inheritance, that together influence a phenotypic trait [8]. In addition to these findings, the genome-wide association study confirmed previously reported associations of alopecia areata with human leukocyte antigen (HLA) genes [9].The HLADQB1* 03 allele, among others, may be an important marker for susceptibility to the disease [10]. Several susceptibility loci that have been associated with other autoimmune diseases (CTLA4, IL-2/IL-21, IL-2RA) also were identified, indicating that AA may share a common pathway with other autoimmune diseases [11].
Immunological factors
AA has been considered as an autoimmune disease due to an aberrant T-cell response against hair follicle self-antigens [12]. The disease represents a continuous reactivity of the pilar units which explains the chronicity of disease and frequent relapse. It was demonstrated that antibodies directed to hair follicle–associated target proteins have been detected in patients with AA [13],as grafting of hairless scalp from AA patients to nude mice results in dramatic regrowth of human hair [14]. This was explained by the removal of immunologic influence from the hair follicles, but does not distinguish whether a humoral or cellular immune pathogenesis underlies AA [15]. Both CD4+ and CD8+ T cell are implicated in AA,as CD4+T cells predominate in the infiltrate surrounding the hair follicle, while T cells within the follicular epithelium are predominantly CD8+ [16]. Clinical observations have long suggested that melanocyteassociated autoantigens may be targets in AA,and this explained why AA arises in pigmented hair only [17].
The potential importance of cytokines in AA
The histopathologic features of the disease consist of perifollicular lymphocytic infiltrates around anagen hair follicles, consisting of both CD4+ and intra-follicular infiltrates of CD8+ cells. Several studies have shown that within the cascade of pathogenesis of alopecia areata, cytokines and other molecules that coordinate cyclical hair growth were demonstrated as, presence of labeled cells with IL-1β, IL6, INF- γ, and GB antisense probes, in the mononuclear infiltrate around the hair follicles in AA patients [18].
Psychological trauma
Acute emotional stress may precipitate alopecia areata by activation of over expressed type 2b-corticotrophin releasing hormone receptors around the hair follicle leading to local inflammation [19]. Release of substance P-from the nerves in response to stress has been reported and the same is noted in the hair follicles in alopecia areata. Substance P degrading enzymes have been expressed in the hair follicles in both acute and chronic alopecia areata [20]. In more recent study an immunomodulatory neuropeptide in AA, was studied in a C3H/HeJ mouse model. It was demonstrated that expression of number of SP-immuno-reactive nerve fibers in skin during early stages of AA development, increased, compared to non-affected mice. However, during advanced stages of AA, the number of SP-immuno-reactive nerves and SP protein levels in skin are decreased [21].
Other factors: A variety of factors, such as infections, drugs, and vaccinations, have been implicated in triggering episodes of alopecia areata. Cytomegalovirus infections and hepatitis B vaccination were implicated, but further studies failed to confirm any correlation [22].In other hand AA was less frequently observed in people, taking diet rich in soy oil [23].
Alopecia areata monolocularisis a variant called "spot baldness” it was reported as clozapine-induced. In this variant the beginning phase of autoimmune process in AA, triggred by eosinophilicperi-bulbar infiltrates [24].
Clinical feature of AA
Alopecia areata can be simply defined as normal scalp's skin except loss of hair, which means on examination, no dandruff, no scarring and no redness. AA is usually asymptomatic although patients may occasionally feel, pruritus or a burning sensation which may precede the loss of hair. Alopecia most commonly occurs on the scalp, but may be found on any hairbearing area. Short hairs broken off a few millimeters from the scalp (also known as exclamation point hairs) may be found at the edges of expanding patches (Figure 2) [25].
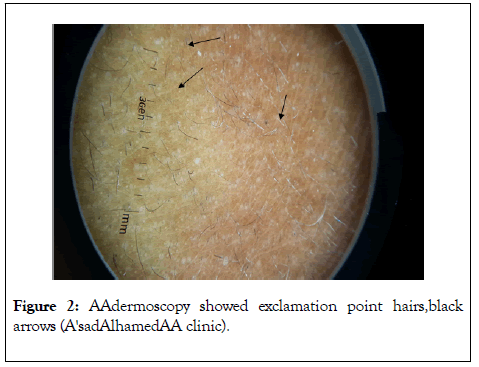
Figure 2: AAdermoscopy showed exclamation point hairs,black arrows (A'sadAlhamedAA clinic).
Severity of AA
Severity of alopecia areata can be emphasized from different aspects, as number and size of patches of hair loss, anatomical sites of scalp at which areata affecting and also at more specified way with SALT score. It is a quantitative tool for assessment of AA severity affecting scalp hair loss. In SALT, the entire scalp was divided into 4 parts based on the surface area, top (40%-0.4%), posterior (24%-0.24%), right side (18%-0.18%), and left side of scalp (18%-0.18%). Percentage of hair loss in each area is determined independently and is multiplied by the percentage of scalp covered in that area of the scalp.
SALT score is easily reproducible and validated, but it does not include hair pigmentation, body hair, and nail involvement [26].
SALT score for an adult male patient with multiple AA patches seen in our clinic( AA clinic A'sadAlhamed AA clinic)which involves all areas as right side, top, posterior and left side of scalp, the hair loss is 50%, 30%, 20% and 40%respectively, then the SALT score can be calculated=(50 × 0.18)+(30 × 0.4)+(20 × 0.24)+(40× 0.18)=9+12+4.8+7.2=32.7. This score indicated that is a sever AA case (Figure 3).
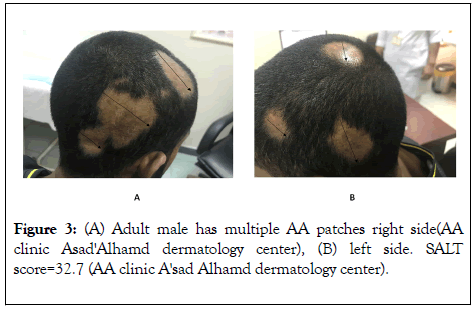
Figure 3: (A) Adult male has multiple AA patches right side(AA clinic Asad'Alhamd dermatology center), (B) left side. SALT score=32.7 (AA clinic A'sad Alhamd dermatology center).
An Automate SALT Score analysis via Computationtexture is now available for pediatric alopecia areata, which provides more information about the continuum of changes in density of hair seen in alopecia areata [27].
Severity of alopecia areata
Severity of alopecia areata can be divided according to number and sizes of patches as follows [28].
Mild: Three or less patches of alopecia with a widest diameter of <3 cm or disease limited to eyelashes and eyebrows.
Moderate: Existence of more than three patches of alopecia or a patch greater than 3 cm at the widest diameter without alopecia totalis or universalis.
Severe: Alopecia totalis or alopecia universalis.
Atypical forms of AA which may take specific distribution, and take certain names, like [29]:
Ophiasis pattern: A band-like area of alopecia extending across the occipital scalp may occur in some patients.
Sisaipho pattern: This is a rare pattern of alopecia areata, also known as ophiasisinversus, it presents with alopecia involving the frontal, temporal, and parietal scalp but spares hair along the scalp periphery. This distribution resembles the pattern of hair loss seen in androgenetic alopecia.
In a minority of cases, disease may progress to complete loss of scalp hair (alopecia totalis) and body hair (alopecia universalis).
Alopecia areata incognita (AAI)
Alopecia areata incognita (AAI) called acute diffuse and total alopecia of the female scalp (ADTAFS) is a new rare form of alopecia areata subtype starts with an acute, diffuse and total hair loss of the scalp in young women (20 to 40 years). In cases of alopecia areata incognita, the typical patchy distribution of hair loss in classical alopecia areata is absent, but abrupt and intense hair loss is characteristic [30]. Tosti et al, reported 70 patients with AAI, of whom 50 cases were histologically confirmed. While the clinical picture presented by this disease closely resembles that of telogen effluvium, specific clinical and dermoscopic findings of alopecia areata are invariably present along the disease course [31].There is a controversy regard the established diagnosis of alopecia areata incognita as a new entity of alopcea areata, even with trichoscopic finding of yellow dots observed in AAI (Figures 4 and 5) [32].
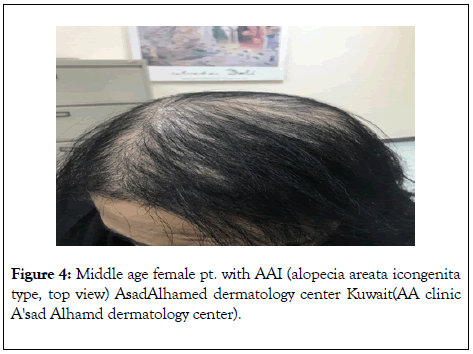
Figure 4: Middle age female pt. with AAI (alopecia areata icongenita type, top view) AsadAlhamed dermatology center Kuwait(AA clinic A'sad Alhamd dermatology center).
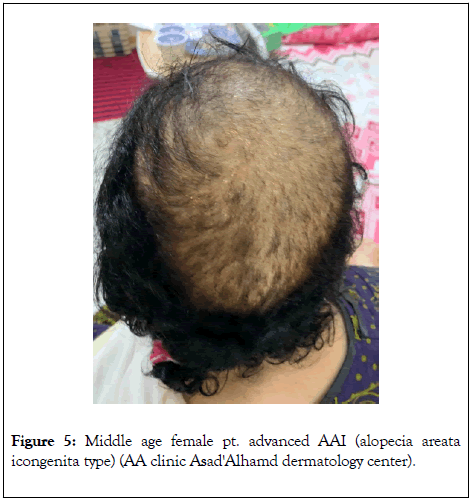
Figure 5: Middle age female pt. advanced AAI (alopecia areata icongenita type) (AA clinic Asad'Alhamd dermatology center).
The dermoscopic findings of AAI, are diffuse, round or polycyclic yellow dots, which is a specific feature of alopecia areata, and regrowing, tapered, terminal hairs [33]. Shown in the below Figure 6.
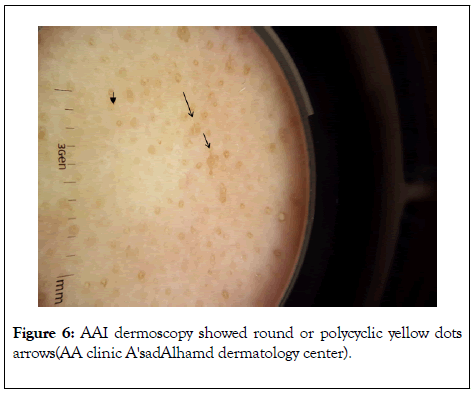
Figure 6: AAI dermoscopy showed round or polycyclic yellow dots arrows(AA clinic A'sadAlhamd dermatology center).
Linear AA is rare presentation of alopecia areata, and it published in medical literatures as a case report [34-36].
A young female patient 9 years old was presented to out patient clinic with this linear lesion of scalp for about one year (Figure 7). A thorough history taken especially about previous trauma, itching or hair traction by child herself (trichotillomania), also her mother asked if lesion was there since birth, but she denied. On examination, the lesion is in occipital area with slight pigmented skin and linear hair loss. A skin biopsy was taken and sends to pathology lab, which revealed non specific features. Patient lost follow up for about 4 months, then come with hair regrowth (Figure 8) without using any treatment as her mother confirmed (spontous resolution) which goes with linear AA.
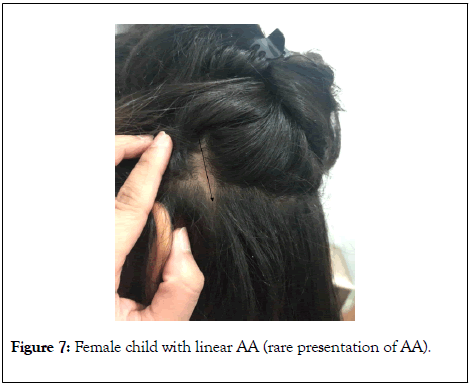
Figure 7: Female child with linear AA (rare presentation of AA).
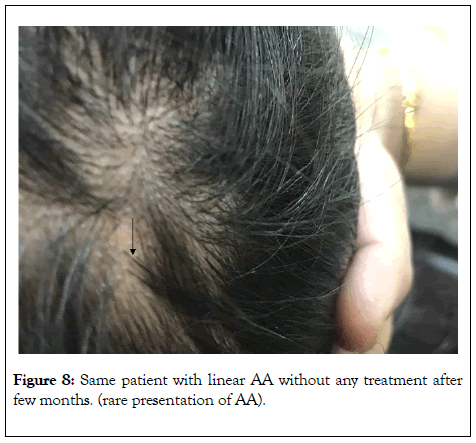
Figure 8: Same patient with linear AA without any treatment after few months. (rare presentation of AA).
Trichoscopic features in AA
Trichoscopy is an useful diagnostic tool in some cases of alopecia areata with atypical course of disease, where the diagnosis may not be established only on basis of clinical appearance [34].
Characteristic Trichoscopic features in noncicatricialalopecias :
• Hyperkeratotic plugs in hair follicles (yellow dots).
• Cadaverized hairs (black dots),
• Micro-exclamation mark hairs (visible when 1 mm or less in length).
• Dystrophic and regrowing hairs.
• Some-vellus hairs may also be present.
The average hair thickness is not significantly decreased and features of fibrosis may be seen in long-lasting AA [34]. As shown in below figures (Figures 9-12).
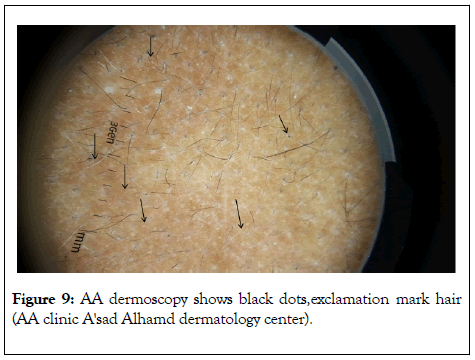
Figure 9: AA dermoscopy shows black dots,exclamation mark hair (AA clinic A'sad Alhamd dermatology center).
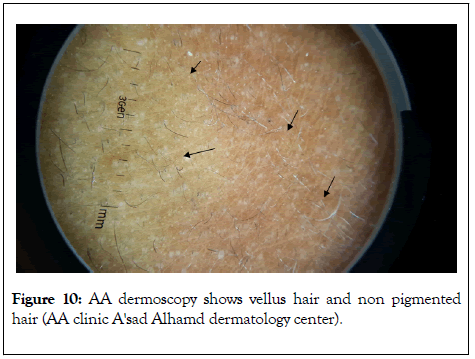
Figure 10: AA dermoscopy shows vellus hair and non pigmented hair (AA clinic A'sad Alhamd dermatology center).
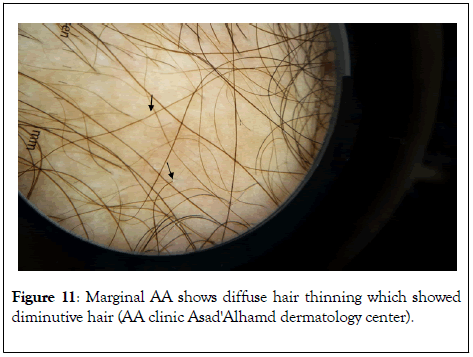
Figure 11: Marginal AA shows diffuse hair thinning which showed diminutive hair (AA clinic Asad'Alhamd dermatology center).

Figure 12: Severe AA dermoscopy showed short cadaverized hair (AA clinic Asad'Alhamd dermatology center).
Cicatricialalopecias (scarring alopecias)
Trichoscopy has a usefulness role in the clinical diagnosis of different types of scarring alopecia,cicatricial alopecias have specific trichoscopic features regardless their different etiology [35], as represented a diverse group of diseases characterized by a lack of follicular ostia and irreversible alopecia. In trichoscopy, fibrosis of follicular ostia is visible in the form of white dots (Figure 13) [36].
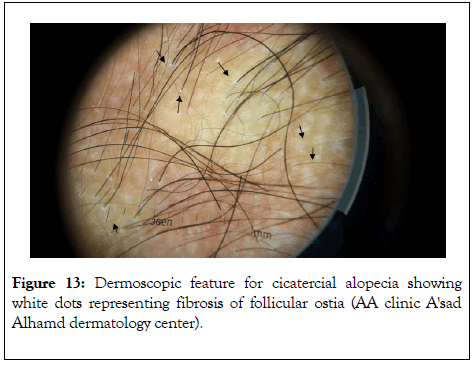
Figure 13: Dermoscopic feature for cicatercial alopecia showing white dots representing fibrosis of follicular ostia (AA clinic A'sad Alhamd dermatology center).
In more advanced stages of cicatercial alopecia these white dots coalesce to form a cohesive area lacking follicular ostia arrows in Figure 14.
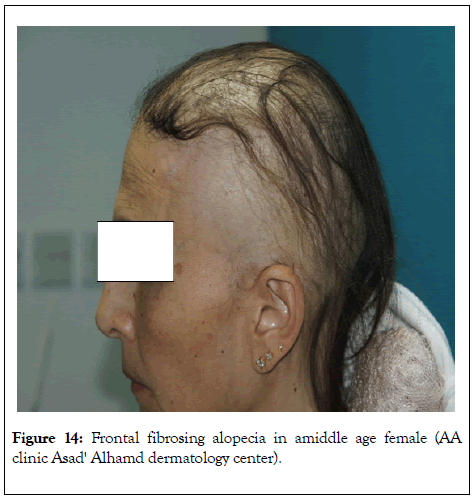
Figure 14: Frontal fibrosing alopecia in amiddle age female (AA clinic Asad' Alhamd dermatology center).
Frontal fibrosingalopciea
Frontal fibrosing alopecia (FFA) is scarring alopecia known firstly described in 1997 as a clinical variant of lichen planopilaris [37].Recently, a worldwide increase in the incidence of FFA has been observed [38].Trichoscopy is useful tool in FFA and for differential diagnosis between FFA and other scarring alopecia, especially presence of perifollicular erythema is considered a direct marker of disease activity (Figure 15) [39].
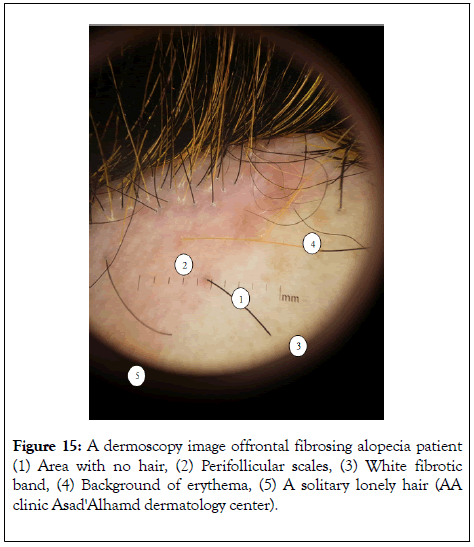
Figure 15: A dermoscopy image offrontal fibrosing alopecia patient (1) Area with no hair, (2) Perifollicular scales, (3) White fibrotic band, (4) Background of erythema, (5) A solitary lonely hair (AA clinic Asad'Alhamd dermatology center).
Histopathological staging in AA
The histopathologic features of AA depend on the duration of disease [40].
In the acute stage, bulbar lymphocytes surrounded terminal hairs in early episodes with presence of miniaturized hairs in repeated episodes.
In the subacute stage, decreased anagen and increased catagen and telogen hairs were characteristic.
In the chronic stage, decreased terminal and increased miniaturized hairs were found, with variable inflammation. During recovery, increasing numbers of terminal anagen hairs from regrowth of miniaturized hairs and a lack of inflammation were noted.
Extra-follicular manifestations in AA
Extra follicular involvement can be observed in alopecia areata, particularly in its more severe forms, comprising nail changes, eye involvement, and somereports of a possible relationship with salmon patch on nape of the neck [41].
Nail abnormalities: The clinical presentation of nail changes in AA varies according to the severity and localization of the lesion. Nail changes in AA are variable in incidence as it was reported from 7 and 66 percent of alopecia areata patients R [42]. The most common nail abnormality in AA is nail pitting resulting from the presence of easily detachable parakeratotic cells in the superficial layers of the nail plate. This change indicates a disturbance in the maturation and keratinization of the proximal nail matrix and results in nail depressions or pits [42].
Ocular disorders: Dry eye disease was reported in 84% of 32 alopecia areata studied patients compared in only 15% of 20 controls. T-cell mediated autoimmunity has a prominent role in the etiopathogenesis of alopecia areata and dry eye disease, as inflammatory mechanisms causing alopecia areata may trigger dry eye disease or vice versa [43].
Other autoimmune diseases: AA has been associated with other auto immune disorders such as vitiligo, lupus erythematosus and ulcerative colitis [44].
Thyroid autoimmunity has is the strongest association with AA among other autoimmune disorders has been with which occurs in 8 to 28 percent of patients [45]. Both alopecia areata AA and vitiligo are autoimmune diseases, and their coexistence in the same patient is not uncommon, as vitiligo has been reported to occur in 4.1% of patients of AA and is about 4 times more common in patients with AA than in the general population [46]. This is evidenced immunohistologically by the findings of helper T-lymphocytes and antibodies against abnormal hair bulb melanocytes in both two diseases [47]. Atopic disorders, particularly atopic dermatitis, have also been linked with alopecia areata, an association between AA and atopic dermatitis for the groups of patients suffering from atopic dermatitis with asthma and atopic dermatitis with asthma and allergic rhinitis [48].
Cancer risks among patients with AA
A Korean study demonstrated decreased risk of several cancers has been observed in patients with AA, that includes breast, colon, rectum, stomach, liver, and lung, but at the same time significantly an increased risk of thyroid cancer was there [49]. Also there was a significantly decreased risk of non-melanoma skin cancers (NMSC) in AA patients than controls, and a protective effect as reduced risk to melanoma skin cancers has been reported [50].
Genetic disorders associations
Down's syndrome (trisomy 21).There is an association of alopecia areata with Down's syndrome, as high frequency of alopecia areata in autoimmune polyglandular syndrome type I due to mutations of the autoimmune regulator (AIRE) gene on chromosome 21q22.3 and the finding of association with MX1, another gene in the Down's syndrome region of chromosome 21 indicate this area of the genome as a promising target for futurefamily based investigations [51]. In a study of 1000 institutionalized patients with Down syndrome, the prevalence of alopecia areata was approximately 6 percent [52].
Approximately 20 percent of people with alopecia areata have a family member who is also AA affected. Based on this, experts believe that some people have a genetic predisposition to the disease [53].
The rate of depression, stress, and neurosis was higher in AA patients than in the normal population [54]. An Iranian study showed a lower educational level in AA patient group compared with the control group, low education level consequently leads to personal and social problems and vice versa [55].
AA patients are extremely anxious patients, they are worry about time of hair regrowth. Reassurance and at same time the realistic expectations should be put between their hands. New therapeutic options should be used with cautious and also to be based on scientific evidence based studies,the patients should informed about these drugs and their side effects. Prognostic outcome of treatment of AA depends on history and examination of patients.
The onset of AA at younger age and long duration are bad prognostic factor, also positive family history of AA or other autoimmune diseases or atopy are bad prognostic factors. On examinations sever forms of alopecia (AU-AT) and ophiasis variant in addition to nail changes are bad prognostic factors [56].
Treatment of alopecia areata is dependent on age of patient as well as duration and the extent of scalp involvement. Treatments include steroids, topical immunotherapy, topical minoxidil, anthralin, and immune-suppressants. Each case must be dealt with on a customized individual basis. There are no FDA (Food and Drug Administration)-approved curative treatments for alopecia areata (AA). Many therapeutic options exist, but none are curative or preventive [57].
Psychological support
AA is associated with high psychiatric comorbidities and children are more vulnerable to psychological insultin are view of psychiatric problems in-patients with alopecia areata (AA) according to electronic database of MedLine/PubMed was done and found that, the rate of depression in children and adolescents with AA is up to 50% of patients. Generalized anxiety disorders rate was 39% for reported AAcases. AA is highly associated with obsessive compulsive disorder (35.7%) in children and adolescents. In other hand schizophrenia tended to be less seen in AA patients [58].So the combination of antidepressant citalopram with triamcinolone injection in patients with AA and Major Depresive Disorder (MDD) showed more effective than triamcinolone alone for the treatment of AA among patients with MDD [59].
Topical corticosteroids
Mid-potent to potent topical corticosteroids are usually used by dermatologist in AA, especially if the involved area is limited, as topical corticosteroids are far less effective in severe forms of AA like alopecia-totalis and alopecia universalis. Topical use of corticosteroids result in some hazards to patients like folliculitis, telangiectasia and atrophy also may occur rarely. There is relapse after stoppage of topical applications of steroid in about 37%-63% of cases [60].
Intralesional corticosteroids
Intralesional corticosteroids (preferably triamicinolone acetonideas it is less atrophogenic) are considered the firstlinetherapy, for adult AA patients with limited involvement. Triamcinolone acetonide should be given with certain precautions to achieve good response and at same time avoiding the side effects. The proper concentration, interval between injections and depth of steroid injection into the dermis are very important. Different concentrations are available (2.5-10 mg per ml) are the most suitable. Treatment given every 4-6 weeks with insulin syringe (0.5-inch long, 30- gauge needle) used to give the injections of 0.1 ml each approximately 1 cm apart, just beneath the dermis and a maximum of 3 ml in each visit. Treatment should be stopped if there is no improvement after 6 months. Side effects include transient atrophy and telangiectasia, which can be prevented by the use of smaller concentrations and volumes, minimizing the number of injections per site, and avoiding injecting too superficially [61].
Trichoscopy has a prognostic role in treatment of AA as patients with exclamation point hairs and a positive hair pull test respond better to intra-lesional corticosteroids (ILCs), as these reflect the active inflammation of the follicles [62]. Dermoscopy is also very useful to identify signs of early clinical response, adverse effects during intra lesional triamcinolone acetonide. In a study it demonstrated regrowth of new vellus hair at 4 weeks after ILCs. At12 weeks, complete disappearance was seen in tapering hairs, broken hairs and black dots whereas for yellow dots to disappear completely in all patches it took 16 weeks. The adverse effects were observed at an earlier stage using dermoscopy than clinically [63].
The scalp and face, respectively are the preferred site for injection, but dermatologist should take in consideration the delicate anatomy of face especially ocular area. Local injection of steroids, even at sites far from the eye, have been associated with the development of cataract, glaucoma, and even retinal and choroidal emboli [64]. Children younger than 10 years are not usually treated with ILCs because of pain localized at the injection sites, there are some options to reduce pain include the use of smaller gauge 30 G or 32 G needles, ice or cold compresses, also a prilocaine-free anesthetic is safe effective anesthetic creams in children (Figures 16 and 17) [65].
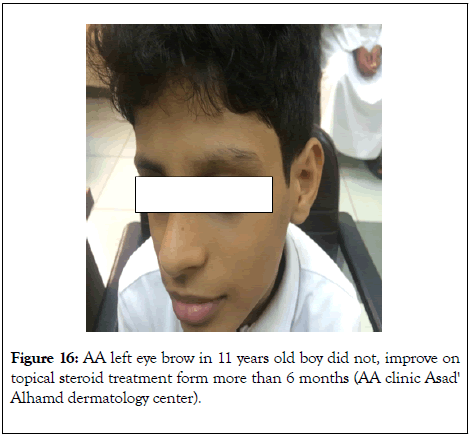
Figure 16: AA left eye brow in 11 years old boy did not, improve on topical steroid treatment form more than 6 months (AA clinic Asad' Alhamd dermatology center).
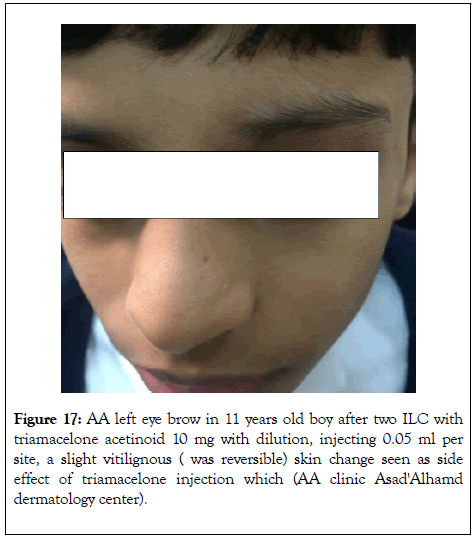
Figure 17: AA left eye brow in 11 years old boy after two ILC with triamacelone acetinoid 10 mg with dilution, injecting 0.05 ml per site, a slight vitilignous ( was reversible) skin change seen as side effect of triamacelone injection which (AA clinic Asad'Alhamd dermatology center).
Topical irritants and immune sensitizers
Anthralin: Anthralin is 1% cream can be used as short contact therapy. It's mechanism of action is unknown, but it depends on sensitization of skin which may trigger an inflammation by generating free radicals that have anti-proliferative and immunosuppressive actions [66]. It is applied daily for 15–20 min initially and then washed. The contact time is increased by 5 min weekly up to 1 h or until low-grade dermatitis develops. The contact time is then fixed and continued daily for at least 3 months before judging the response to treatment. It is effective therapy for AA and should be continued at least 9 months [67].Anthralin1% cream is safe in children with chronic, severe, treatment-refractory, extensive AA.
Minoxidil: Topicalminoxidil 5% solution or foam is frequently used with other therapeutic agents as an adjuvant therapy in AA.The mechanism by which minoxidil works, still unknown. Minoxidil has indirect action, as it may increase blood supply to hair follicle in dermal papilla through vascular vasodilation. Local irritation is another theory by which minoxidil works, even its vehicle component works in AA, when topically applied [68].
Previous studies did not show any beneficial action of topical minoxidil in severe forms of A.A (alopecia total is and alopecia universalis). Minoixidil side effects include contact dermatitis and hypertrichosis [69]. More recent study demonstrated more specified effects to minoxidil, as it has a direct action which is mitogenic effect on epidermal cells, both in vitro and in vivo. Plucked hair from men applying minoxidil showed increase in proliferation index which measured by DNA flow cytometry for anagen-phase hair bulbs. In vitro minoxidil also found to prolong the survival time of keratinocytes. Calcium influx normally enhances epidermal growth factors to inhibit hair growth, minoxidil may oppose this action, as it inhibit calcium entry, and finally in contray to the old theory local vasodilatation does not appear to play a primary role in hair growth associated with minoxidil [70].
Topical immunotherapy
Topical immunotherapy is used in severe and refractory AA, and showed promising results in these cases. Topical immunotherapy include dinitrochlorobenzene (DNCB), squaric acid dibutylester (SADBE), and diphencyprone (DPCP).The mechanism of action of topical sensitizers is poorly understood. Many theories have been suggested, including antigenic competition, perifollicular lymphocytes apoptosis, changes in the peribular CD4/CD8 lymphocyte ratio, and interleukin-10 secretion after diphenylcyclopropenone (DPCP) application [71].
Topical immunomodulators
Topical calcineurin; inhibitors, were developed for the treatment of inflammatory skin diseases. Pimecrolimus, is one of calcineurin; inhibitors,it is an ascomycin derivative, it acts as a cell-selective cytokine inhibitor developed for the treatment of inflammatory skin diseases [72]. Pimecrolimus cream is not expected to be effective for hair regrowth because it permeates no lower than the superficial dermis, which is an insufficient depth for targeting T cells involved in AA [72].In contrary another study showed that pimecrolimus cream 1% BID for two months duration, may be effective therapy for the treatment of alopecia areata [73].
Phototherapy
NB UVB has been included as a treatment option in some AA treatment guidelines [74].There is controversy of efficacy of this method in treatment of alopecia areata, although erythema induced by UVB is similar to other skin irritants used in the treatment, there is little evidence of efficacy in the literature [75]. PUVA (psoralen plus ultraviolet light A) is another optional treatment for AA, as it targeting the inflammatory infiltrate around hair follicles in AA. Topical PUVA showed a promising result in sever forms of AA (AA totalis or universalis), as 85% of patients had good to excellent response to the treatment [76].
Turban PUVASOL is a new method for phototherapy (turban psoralen with sunlight exposure), was found to be effective treatment in Alopecia Totalis in two reported cases [77].
Systemic therapy
Cortisteroids: Oral steroid can given to severe recalcitrant cases of AA, there is no specific dose regimen for AA, many regimens were tried as given short course of systemic prednisone in adult patient with body weight 60 kg, who given prednisone 40 mg tab. for three days only, then decreased by 5 mg every three days till 5 mg and discontinued. This regimen succeeded to regrow the hair [78].This very short steroid course selectively given to minimize the hazards of systemic steroid on human body if taken for long duration. Although the promising result of systemic steroid in hair regrowth in AA, the high relapse rate after discontinuation of therapy and side-effects during limited their use. In more recent study a high dose of prednisone a 300 mg asoralpulse therapy once-monthly for 3-6 months showed proper hair regrowth 82% of patients with extensive, affecting more than 40% of the scalp [79].
Methotrexate: Methotrexate was used for AA treatment, in regimen as psoriasis, it can be given in weekly dose (15-25 mg),it induced complete hair regrowth in about 57%,however it showed a higher number 63% of hair regrowth when combined with systemic steroidin low dose 10-20 mg [80].There is high incidence of relapse in AA after discontinuation of methotrexate, more than75% in addition to adverse-effects like elevated liver enzyme levels and gastrointestinal discomfort [81].
Oral cyclosporine: Oral cyclosporine is one of effective therapeutic options in severe AA cases in dose 2.5-6 mg/kg/d, as it showed a significant hair growth in patients that have the disease for less than four years [82].Its action through suppression of helper T cells activation. It also alters CD4/CD8 ratio, by these actions it clears immune cells targeting hair follicles and adjusts the balance of regulatory lymphocytes [83].Topical applying a lotion containing 250 mg of cyclosporine in 80 ml of isopropyl alcohol, 10 ml of propylene glycol, and 15 ml of distilled water once in a 23 years old patient with alopecia universalis. Hair regrowth was reported after about 10 months [84].
Alopecia areata: A new treatment modulaties
In the last few years, biologics drugs became one of golden stone therapy in autoimmune disease in rheumatology and also in multiple autoimmune dermatoses, so we can called it era of biologics. AA is one of dermatoses which biologics used as a new therapeutic line in control alopecia cases. Anti-TNF agents (etanercept and infliximab) were tried in AA cases, but they did not show any hair regrowth or prevent AA development [85], even there was worsening of AA cases in some patients receiving infliximab [86].
Tofacitinibvitrate (Xeljanz)
Tofacitinib, is an inhibitor of the enzyme janus kinase 1 (JAK1) and janus kinase 3 (JAK 3), which means that it interferes with the JAK-STAT signaling pathway, which transmits extracellular information into the cell nucleus, influencing DNA transcription, controlling the role, that cytotoxic T lymphocytes play in AA and the potential of JAK inhibition, through target the Janus kinase (JAK) pathway as a target for treatment [87].A retrospective cohort study of 90 adults taking tofacitinib at a dosage of 5-10 mg twice daily for 4 months or longer with or without prednisone (300 mg once monthly for three doses), 77% of patients showed improvement inform of hair regrowth (Figures18-20) [88].
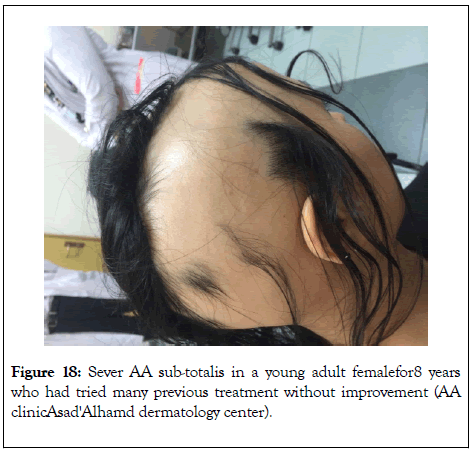
Figure 18: Sever AA sub-totalis in a young adult femalefor8 years who had tried many previous treatment without improvement (AA clinicAsad'Alhamd dermatology center).
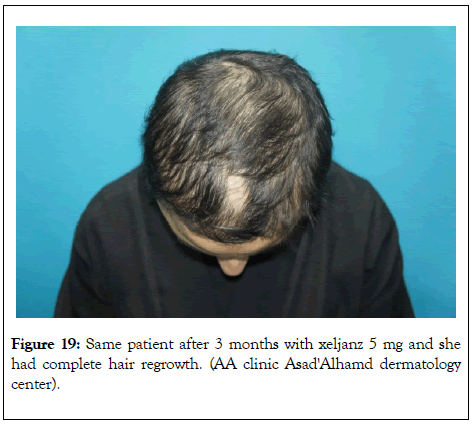
Figure 19: Same patient after 3 months with xeljanz 5 mg and she had complete hair regrowth. (AA clinic Asad'Alhamd dermatology center).
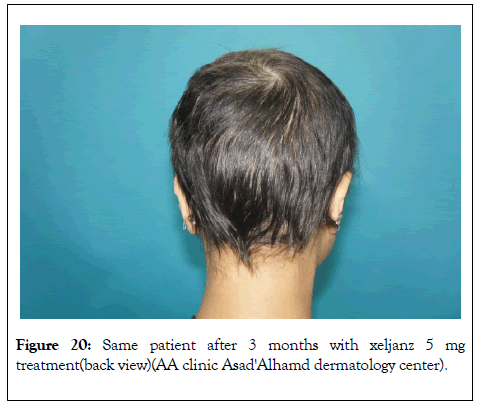
Figure 20: Same patient after 3 months with xeljanz 5 mg treatment(back view)(AA clinic Asad'Alhamd dermatology center).
Although tofacitinib is efficacious in the treatment of AA, but it has a lack of durability of effect after the discontinuation of therapy, resulting in hairloss (improvement inform of hair regrowths 21 and 22) [89].
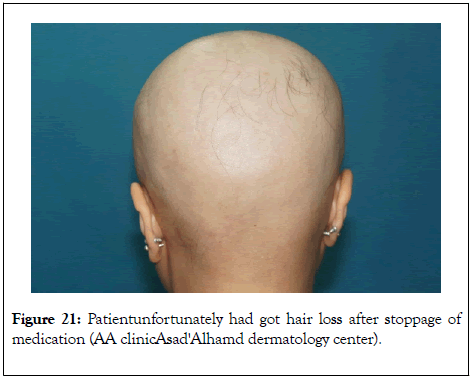
Figure 21: Patientunfortunately had got hair loss after stoppage of medication (AA clinicAsad'Alhamd dermatology center).
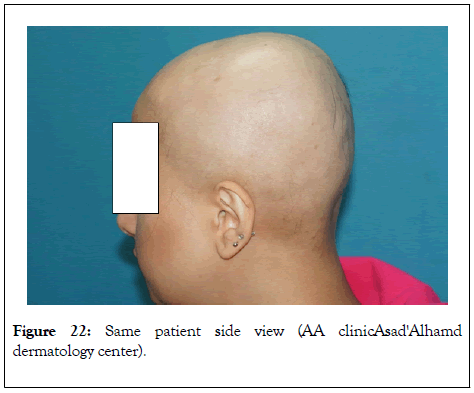
Figure 22: Same patient side view (AA clinicAsad'Alhamd dermatology center).
A case report of topical tofacitinib, Topical tofacitinib 2% in solution twice daily to the left upper eyelid eyelashes in young adult female in late 20s, who has AA of eye lashes and was not responded to previous treatments, after 4 months, there was near complete hair regrowth [90].
Stem cells in the skin
There is a newly emerging therapy depend on stem cell, called Stem Cell Educator therapy, it was done in an open-label, phase 1/phase 2 study, in nine patients with severe AA, the median age of patients was 20 years and median alopecia duration was 5 years. The patients ’ s blood were with-drawen and circulated through a closed-loop system, to separate mononuclear cells from the whole blood. Then expose the cells to brief interaction with adherent human cord blood-derived multipotent stem cells (CB-SC), these cells now called an “educated” autologous cell which returns back to the patient’s circulation. An improvement in the patients in form of hair regrowth and better quality of life [91].
Hair transplantation in AA
In 2005 Barankin and his colleagues, reported a successful trial of hair transplantation of eyebrow in a patient with AA [92].Another reported case of successful hair transplantation into the scalp with stationary AA for 10 months, in a 62 years old male patient with recalcitrant AA of scalp for 4 years duration [93].
Non-pharmacological therapy for AA (Hair camouflage)
Wigs: Wigs are easy and cheap options in AA patients, there two types either of natural human hair wigs versus synthetic hair wigs, of course the natural one looks more natural, and more stable to heat damage. Wefted, is well-known foundations, as it is cheapest, but the more expensive, more stable in color, moves like natural hair and styled as natural hair as it is from real human hair fibers [94].
Pigmented concealing powders, lotions and sprays
Topical hair fibers is analternative materials can be used to conceal thinning hair, they are positively charged particles of wool keratin that adhere to the negatively charged terminal and vellus hair fibers on the scalp [94].
Camouflage tattoo (micropigmentation)
Micropigmentation (dermagraphics or permanent make-up) is a procedure in which an injection of iron oxide pigment into the middle layer of the skin for long-lasting results. It must be done by a trained specialist. It can used for eyebrows AA, or even hairline [95].
Mesotherapy
Mesotherapy is non-surgical cosmetic medicine treatment that employs multiple injections of pharmaceutical and homeopathic medications, plant extracts, or vitamins. Hair mesotherapy can also be called “ mesoplasty ” or “ mesohair. In the hair mesotherapy, there is cocktail of whose effectiveness has been proved according to physician’s practice and experience [96].The active ingredients in the cocktail increase local microcirculation, provide nutritional input, slow down the programmed process of follicular involution, stimulate the hair ’ s environment through neddling and complement other treatments [97].
Laser treatment
Alopcia areata patients may get some benefit from laser therapy, this effect through laser with wave length same as ultraviolet, the excimer laser (wavelength of 308 nm),specially for non-regressive AA. Treatment sessions were done twice a week, for a maximum 24 sessions. There was maintained hair growth even after laser sessions stopped after 3 months [98].
Vitamins
In previous studies, it was found that serum vitamin D, zinc, and folate levels tend to be lower in patients with AA as compared to controls, specially vitamin D which might modify the immune response by inhibiting Th1 cell proliferation, the predominant T-helper cell-type in AAR [99].The evidence is conflicting or insufficient to suggest differences in levels of iron, vitamin B12, copper, magnesium, or selenium [100]. Prospective studies are needed to be done in order to establish a definitive clinical recommendation such as routine serum level testing, or therapeutic supplementation [101].
AA (according to my experience) is one of the most dermatological diseases, which patients themselves or their surroundings from family, friends or hairdressers, volunteer to give their advises to use some herbal substances which known as folkloric medications (wasafa in arabic) like, garlic or cutting the scalp skin before seeking a doctor ’ s advice. An ethnopharmacological survey of home remedies used for treatment of hair and scalp have been done by Zaid and his colleges. In their survey a 41 plants are known as a treatment of hair and scalp disorders belonging to 27 families; among them Lamiaceae and Rosaceae, which were the most commonly used in hair loss, dandruff, split hair endings and lice treatment.
Although AA is completely benign dermatosis, but it is not like that, for patients, whatever male or female. Our hair specially scalp, eyebrows and eye lashes are preciousgifts that giveus beauty, confidence, and make uslooked acceptable to ourselves and toothers. Alopecia areata is a common dermatosis and it is considered on top list presented to dermatologists as it accounts 2% of the dermatological consultations. Although it is a totally benign disorder and does not carry any morbidity or mortality risk to affected patients, but it emotionally devastating condition that as it affects their life quality. Psychoeducation, emotional support concurrently with different therapeutic lines are mandatory.
Citation: Almasry I, Al-Lafi A, Harbi R, Lazarevic V, Al Alawi G (2020) Alopecia Areata in Kuwaiti Patients with Dermoscopy View of Some Cases. Hair Ther Transplant. 10:153.
Received: 14-Jul-2020 Accepted: 28-Jul-2020 Published: 04-Aug-2020 , DOI: 10.35248/2167-0951.20.10.153
Copyright: © 2020 Almasry I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.